Journals
Dangers of Videolaryngoscopy-Assisted Intubation: Risk for Multiple Otolaryngologic Complications
A B S T R A C T
Objectives
Discuss the management of upper airway injuries associated with videolaryngoscopy-assisted endotracheal intubation in a single tertiary care institution.
Emphasize the need for thorough otolaryngologic evaluation, to include direct laryngoscopy, given the potential for multiple concurrent injuries.
Methods
Case series and literature review.
Results
Six intraoperative consults were requested of the otolaryngology service regarding traumatic videolaryngoscope-assisted intubations at a single tertiary care institution. 3/6 patients had elevated BMI, and 5/6 patients had an ASA score of 3. All patients sustained a right sided injury, and 4/6 presented with concurrent injuries at multiple sites. All injuries were immediately appreciated after intubation. While 3/6 patients with pharyngeal lacerations were able to be closed with primary closure, 3/6 required palatoplasty due to transpalatal intubation.
Conclusion
Videolaryngoscopy has become an increasingly popular among anesthesia professionals for its ability to provide an improved view of the glottis without excessive anterior displacement of tongue and mandible. The reported incidence of videolaryngoscopy-related complications is 1%, the majority of which are minor. Significant palatal injuries are not uncommon and may require procedural intervention from an otolaryngologist. Transpalatal intubation creates a potential difficult-airway dilemma and may be treated with palatoplasty. Patients may present with multiple injuries to the aerodigestive tract, requiring thorough evaluation and procedural management. Proper training and direct visualization with insertion of the videolaryngoscope during intubation are essential. Otolaryngologists should be familiar with injury patterns seen in videolaryngoscope-assisted intubation trauma and strategies for treatment.
Keywords
laryngoscopy, videolaryngoscopy, traumatic intubation
Introduction
Videolaryngoscopy has become an increasingly popular among anesthesia professionals for its ability to provide an improved view of the glottis without excessive anterior displacement of tongue and mandible. Particularly in patients with perceived difficult airways (i.e., obese, status post head and neck irradiation), videolaryngoscopy is widely used to secure the airway [1, 2]. In contrast to direct laryngoscopy, videolaryngoscopy removes the need to have direct alignment of the laryngeal vestibule and the oral cavity [3]. This indirect method of laryngoscopy not only improves glottic visualization in otherwise unfavorable anatomic circumstances, but ideally allows for intubation to proceed with less pressure exerted on the base of the tongue [3-5]. The decreased force required to obtain glottic visualization has been suggested to lead to less cervical movement when compared to direct laryngoscopy, which is functionally advantageous in-patient populations with cervical spine precautions or limited mobility [3, 6]. However indirect visualization is not without its weaknesses, as the technique predisposes to inherent blind spots in the oropharynx, which increases the risk for injury [2, 7]. The reported incidence of videolaryngoscopy-related complications is 1%, the majority of which are minor injuries [8-11]. Significant palatal injuries are not uncommon, however, and often require procedural intervention from an otolaryngologist.
Methods
The present article details a case series performed at a single tertiary care institution over a two-year period. A literature review was also conducted, with keywords “videolaryngoscopy”, “intubation injury”, and “palatal trauma” reviewed. No statistical analysis was performed on the obtained data.
Results
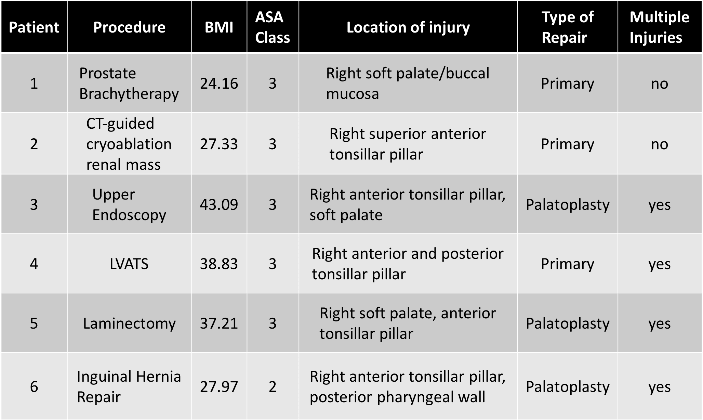
Six intraoperative consults were requested of the otolaryngology service regarding traumatic videolaryngoscopy-assisted intubations at a single tertiary care institution (Table 1). 3/6 patients had elevated BMI, and 5/6 patients had an ASA score of 3. All patients sustained a right sided injury, and 4/6 presented with concurrent injuries at multiple sites. All injuries were immediately appreciated after intubation. While 3/6 patients with pharyngeal lacerations were able to be closed with simple primary closure, 3/6 required palatoplasty due to transpalatal intubation. Palatoplasty was performed by incising the inferior or the superior ledge of the soft palate or the tonsillar pillar where the endotracheal tube had penetrated. To avoid extubating and to maintain a secure airway, a releasing incision along the soft palate allows the endotracheal tube to be freed. Once the endotracheal tube was secured away from the surgical field, the palatal flaps were then reapproximated using absorbable sutures.
Table 1
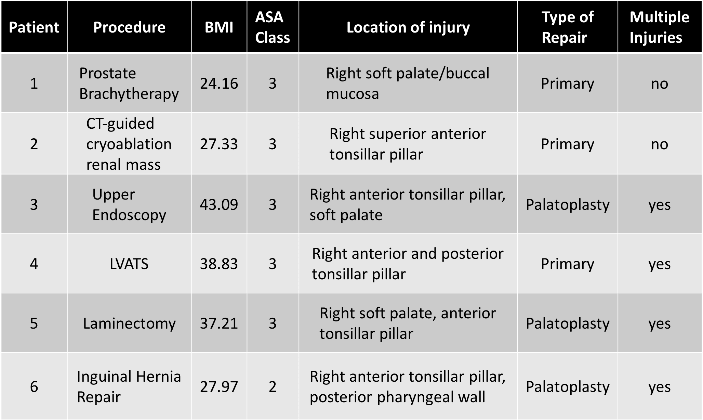
Discussion
While videolaryngoscopy has its advantages, the indirect visualization of oropharyngeal and laryngeal anatomy predisposes to injury [2]. The anatomic subsites most commonly injured with videolaryngoscopy include the tonsils, palate, and base of tongue [2]. In a 2017 study by Greer at al., over 14,500 intubations were compared: 1,713 videolaryngoscopy assisted intubations and 13, 147 direct laryngoscopies [2]. The authors found a statistically significant increase in palate injuries when indirect laryngoscopy was performed [2]. In line with the current author’s findings, the laterality of all injuries was right-sided, presumably secondary to placement of the endotracheal tube with the operator’s right hand [2, 12]. Interestingly, the vast majority of these injuries were not noted during the time of intubation, but rather discovered upon extubation or subsequent re-evaluation of the oral cavity [2]. Conversely, a second 2017 study failed to find any statistically significant difference in rate of injury between direct and indirect laryngoscopy, with the rate of injury 14.29% and 20.51%, respectively [10]. While not statistically significant, 1/5 patients in this study undergoing video-assisted laryngoscopy suffered minimal injury, accentuating the importance of proper training and careful technique.
Many authors suggest that injury most likely occurs during blind introduction of the endotracheal tube into the oropharynx, while the operator is focused on the video monitor instead of the oral cavity [12]. Thusly, emphasis has been placed on ensuring the endotracheal tube is directly seen passing into the oral cavity before attention is diverted to the video monitor [8]. Risk for injury can be further increased with the use of rigid stylets, and as such, softer malleable stylets are recommended [8, 12].
Most injuries secondary to traumatic intubation are minor, however serious trauma can occur during videolaryngoscopy-assisted intubation, requiring procedural intervention. While three out of the six patients in our case series had injuries amenable to simple laceration repair, the remaining three required palatoplasty. Currently, the consensus is that large, gaping injuries or perforated injuries with a hanging flap should undergo procedural intervention and repair [12]. Antibiotics should be considered on a case-by-case basis, however, are generally indicated for larger injuries over 1 cm or those that are contaminated [12]. Additionally, despite the close proximity of great vessels in the oropharynx, screening imaging studies are not indicated for asymptomatic patients [12]. There were no carotid injuries in our case series and neck imaging was not obtained. Finally, in the event of injury, extubation should not be performed until repair, hemostasis, and confirmation of no additional injuries has been accomplished [8, 12]. Confirmation of lack of additional injuries may require direct laryngoscopy or incising the involved tonsillar pillars or soft palate in order to safely retape the endotracheal tube and allow for full visualization of the oral cavity and palate.
The sequelae of unrecognized pharyngeal and palate injury include hemorrhage, infection, retropharyngeal abscess, and inability to perform safe extubation [2, 12]. The majority of patients in our case series presented with multiple injuries to the aerodigestive tract, requiring thorough evaluation and procedural management.
Conclusions
While most injuries secondary to traumatic intubation are minor, serious trauma can occur during videolaryngoscopy-assisted intubation, requiring procedural intervention. Blind entry into the oropharynx with an endotracheal tube during video laryngoscopy assisted intubation may cause soft tissue injury at multiple sites of the aerodigestive tract. In our case series, injuries occurred on the right and were more often associated with patients who had elevated BMI and ASA class. Transpalatal intubation creates a potential difficult-airway dilemma and may be treated with palatoplasty. Patients may present with multiple injuries to the aerodigestive tract, requiring thorough evaluation and procedural management. Proper training and direct visualization with insertion of the endotracheal tube during intubation are essential. Otolaryngologists should be familiar with injury patterns seen in video laryngoscopy-assisted intubation trauma and strategies for treatment.
Financial Disclosure
None
Conflict of Interests
None
Article Info
Article Type
Case ReportPublication history
Received: Thu 21, Feb 2019Accepted: Sat 16, Mar 2019
Published: Tue 02, Apr 2019
Copyright
© 2023 Jessica B. Howell. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.02.09
Author Info
Eric N. Appelbaum Jessica B. Howell Thomas S. Lee
Corresponding Author
Jessica B. HowellDepartment of Otolaryngology – Head and Neck Surgery, Virginia Commonwealth University, Richmond, VA, USA 401 North 11th Street, PO Box 980146, Richmond, VA, 23298
Figures & Tables
Table 1
References
- Yumul R, Elvir-Lazo OL, White PF, Sloninsky A, Kaplan M, et al. (2016) Comparison of three video laryngoscopy devices to direct laryngoscopy for intubating obese patients: a randomized controlled trial. J Clin Anesth 31: 71-77. [Crossref]
- Greer D, Marshall KE, Bevans S, Standlee A, McAdams P, et al. (2017) Review of videolaryngoscopy pharyngeal wall injuries. Laryngoscope 127: 349-353. [Crossref]
- Chemsian R, Bhananker S, Ramaiah R (2014) Videolaryngoscopy. Int J Crit Illn Inj Sci 4: 35-41. [Crossref]
- Niforopoulou P, Pantazopoulos I, Demestiha T, Koudouna E, Xanthos T (2010) Video-laryngoscopes in the adult airway management: A topical review of the literature. Acta Anaesthesiol Scand 54: 1050-1061. [Crossref]
- Bucx MJ, Scheck PA, Van Geel RT, Den Ouden AH, Niesing R (1992) Measurement of forces during laryngoscopy. Anaesthesia 47: 348-351. [Crossref]
- Maharaj CH, Buckley E, Harte BH, Laffey JG (2007) Endotracheal intubation in patients with cervical spine immobilization: A comparison of macintosh and airtraq laryngoscopes. Anesthesiology 107: 53-59. [Crossref]
- Nestler C, Reske AP, Reske AW, Pethke H, Koch T (2013) Pharyngeal wall injury during videolaryngoscopy-assisted intubation. Anesthesiology 118: 709. [Crossref]
- Thorley DS, Simons AR, Mirza O, Malik V (2015) Palatal and retropharyngeal injury secondary to intubation using the GlideScope® video laryngoscope. Ann R Coll Surg Engl 9: e67-e69. [Crossref]
- Cooper RM (2007) Complications associated with the use of the GlideScope video laryngoscope. Can J Anaesth 54: 54-57. [Crossref]
- Scholtis MP, Stoudt RS, Gavel TR (2017) A Randomized, Blinded, Clinical Study of Injury Incidence During Endotracheal Intubation: Comparison of GlideScope Video Laryngoscopy and Direct Laryngoscopy. AANA Journal 85: 445-451.
- Aziz M, Healy D, Kheterpal S, Fu R, Dillman D, et al. (2011) Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2004 Glidescope intubations, complications and failures from two institutions. Anesthesiology 114 :34-41. [Crossref]
- Pham Q, Lentner M, Hu A (2017) Soft Palate Injuries During Orotracheal Intubation with the Videolaryngoscope. Ann Otol Rhinol Laryngol 126: 132-137. [Crossref]
