Comparison between Gastric Babble Sound and Chest X-Ray for Positioning in Nasogastric Tube Insertion on General Anesthesia for Oral and Maxillofacial Patients
A B S T R A C T
Objective: This study aimed to compare gastric babble sound with chest X-ray for positioning in nasogastric tube insertion on general anesthesia for oral and maxillofacial patients.
Methods: Fifty-six oral and maxillofacial patients with nasogastric tube on general anesthesia were included in this study. Length of nasogastric tube using gastric babble sound for positioning in nasogastric tube insertion on general anesthesia were compared with those using chest X-ray after general anesthesia. Furthermore, we evaluated the relationship between height, weight, Body Mass Index (BMI) and length of nasogastric tube using Pearson’s correlation test. A P value lower than 0.05 was considered as statistically significant.
Results: The incidences of adjustment after chest X-ray were 39.3 % (22/56 cases). Regarding cases of the adjustment after chest X-ray, over tube length cases was 90.9 % (20/22 cases, over length: 5.3 ± 1.8 cm) and under tube length cases was 9.1 % (2/22 cases, under length: -10 ± 0.0 cm). Furthermore, Height correlated with length of nasogastric tube using gastric babble sound for positioning in nasogastric tube insertion on general anesthesia (R = 0.505; p = 0.000) and length after adjustment using chest X-ray (R = 0.494; p = 0.000).
Conclusions: The chest X-ray seems to be useful for positioning in nasogastric tube insertion on general anesthesia for oral and maxillofacial patients.
Keywords
Nasogastric tube, chest X-ray, gastric bubble sound, general anesthesia, oral and maxillofacial lesions
Introduction
Nasogastric tubes still remain the easiest and the best way for gastrointestinal tract access [1]. There are various indications for the insertion of a nasogastric tube in anaesthetized and critically ill patients. However, insertion of a gastric tube in anesthetized, paralyzed, and intubated patients can be difficult [2]. Furthermore, inserting a nasogastric tube into unconscious patients can be challenging because these patients cannot cooperate with the operator [3]. The complications of misplacement are rare but very dangerous for the patients [4, 5]. Confirmation of the correct position in the stomach is warranted to avoid serious complications such as misplacement in the lung, and testing pH of aspirate from a tube is one of the techniques to confirm the tip position [6]. One causal factor is that in the National Patient Safety Agency (NPSA) guidance to place a tube, length is measured from nose to ear to xiphisternum (NEX); NEX is incorrect because it only approximates the nose to gastro-esophageal junction distance and is therefore too short [7]. The ultrasound exam appears to be a simple and rapid method for the recognition of the correct positioning of the nasogastric tube in critically ill patients [8].
An abdominal X-ray remains the golden standard, but X-ray interpretation has to be performed by a competent person and if there is any doubt of misinterpretation, the advice of a radiologist should be sought [9]. Furthermore, correct placement is verified using air insufflation [10]. However, to the best of our knowledge, the comparison between gastric babble sound and chest X-ray for positioning in nasogastric tube insertion on general anesthesia for oral and maxillofacial patients has not been reported in the literature. This study aimed to compare gastric babble sound with chest X-ray for positioning in nasogastric tube insertion on general anesthesia for oral and maxillofacial patients.
Materials and Methods
I Patients
This study was approved by the ethics committee of our institution. After providing written informed consent, 56 oral and maxillofacial patients (21 men and 35 women; age 17 to 85 years, mean age 61.4 years) with nasogastric tube on general anesthesia at our university hospital from April 2018 to March 2019.
II Chest X-ray Techniques
All the nasogastric tubes (CORFLO NASOGASTRIC / NASOINTESTINAL FEEDING TUBE WITH STYLET; HALYARD, USA) were positioned by the anesthetist by measuring the distance from the tip of the patient’s nose to the earlobe and from the earlobe to the xiphoid process (NEX). The anesthetist performed the stethoscopy of gastric babble sound in real time. The patients with nasogastric tube insertion were performed chest X-ray after general anesthesia for confirmation of positioning in nasogastric tube insertion. Chest X-ray were acquired with an X-ray machine (ROTANODE; Canon Medical Systems, Otawara, Japan) using the chest protocol at our hospital: tube voltage, 130 kV; tube current, 100 mA.
III Data Analysis
All chest X-ray images were evaluated by the anesthetist and radiologists, and any differences were resolved by forced consensus. Length of nasogastric tube using gastric babble sound for positioning in nasogastric tube insertion on general anesthesia were compared with those using chest X-ray after general anesthesia. Furthermore, we evaluated the relationship between height, weight, Body Mass Index (BMI) and length of nasogastric tube.
IV Statistical Analysis
Statistical analyses for relationship between height, weight, BMI and length of nasogastric tube were performed using Pearson’s correlation test. These analyses were performed with the statistical package IBM SPSS Statistics 26 (IBM Japan, Tokyo, Japan). A P value lower than 0.05 was considered as statistically significant.
Results
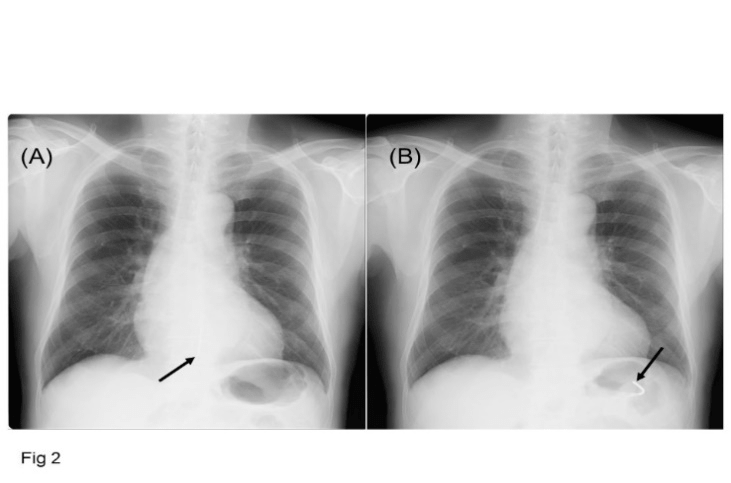
Characteristics of the oral and maxillofacial patients with nasogastric tube on general anesthesia is shown in (Table 1). The incidences of adjustment after chest X-ray were 39.3 % (22/56 cases). Regarding cases of the adjustment after chest X-ray, over tube length cases was 90.9 % (20/22 cases, over length: 5.3 ± 1.8 cm) and under tube length cases (Figure 1) was 9.1 % (2/22 cases, under length: -10 ± 0.0 cm). Table 2 shows relationship between height, weight, BMI and length of nasogastric tube. Height correlated with length of nasogastric tube using gastric babble sound for positioning in nasogastric tube insertion on general anesthesia (R = 0.505; p = 0.000) and length after adjustment using chest X-ray (R = 0.494; p = 0.000).
Table 1: Characteristics of oral and maxillofacial patients with nasogastric tube on general anesthesia.
|
Parameter |
Number of patients |
Mean ± standard deviation |
Range |
|
Age (years) |
56 (100 %) |
61.4 ± 19.8 |
17 - 85 |
|
Gender |
|
|
|
|
Men |
21 (37.5 %) |
|
|
|
Women |
35 (62.5 %) |
|
|
|
Primary diseases |
|
|
|
|
Neoplasms |
37 (66.1 %) |
|
|
|
Inflammatory conditions |
7 (12.5 %) |
|
|
|
Jaw deformity |
7 (12.5 %) |
|
|
|
Trauma |
5 (8.9 %) |
|
|
|
Hight (cm) |
56 (100 %) |
160.7 ± 10.5 |
142.1-182.0 |
|
Weight (kg) |
56 (100 %) |
59.8 ± 14.7 |
37.3-133.0 |
|
BMI (Body Mass Index) |
56 (100 %) |
23.0 ± 4.1 |
16.5-40.2 |
|
Length of nasogastric tube (cm) |
|||
|
Gastric babble sound |
56 (100 %) |
53.4 ± 5.0 |
45 - 70 |
|
Chest X-ray |
56 (100 %) |
51.9 ± 3.8 |
43 - 60 |
|
Adjustment after chest X-ray |
|||
|
Absence |
34 (60.7 %) |
|
|
|
Presence |
22 (39.3 %) |
|
|
|
Over tube length (cm) |
20 (90.9 %) |
5.3 ± 1.8 |
3 - 10 |
|
Under tube length (cm) |
2 ( 9.1 %) |
-10 ± 0.0 |
-10 |
Table 2: Relationship between height, weight, BMI and length of nasogastric tube.
|
Parameter |
Correlation coefficient (R) in length of nasogastric tube |
|
|
|
Gastric babble sound |
Chest X-ray |
|
Height |
0.505 (p = 0.000) |
0.494 (p = 0.000) |
|
Weight |
0.261 (p = 0.052) |
0.255 (p = 0.058) |
|
BMI (Body Mass Index) |
0.000 (p = 0.999) |
-0.026 (p = 0.850) |
Figure 1: Under tube length case of chest X-ray in an 83-year-old male with buccal mucosal carcinoma at pre-adjustment (A) and post-adjustment (B).
Discussion
The positioning of the gastric tube, which is often used in clinical practice, has not yet been standardized [8]. In the USA, the placement of the gastric tube is regularly controlled by checking X-ray images [9]. In many countries in Europe, correct placement is verified using air insufflation [10]. Several methods are suggested to verify the placement of gastric tube, such as the auscultation of bubbling sounds, the sampling of pH aspirates from the feeding tube, a chest X-ray and colorimetric capnography [11]. Therefore, we compared gastric babble sound with chest X-ray for positioning in nasogastric tube insertion on general anesthesia for oral and maxillofacial patients.
Taylor et al. showed that only the electromagnetic trace or possibly direct vision can show in real time whether the tip has safely reached the gastric body [4, 7]. Zatelli et al. indicated that the high sensitivity of the sonography in the verify correct positioning of gastric tube in the adult ICU patients [8]. Boeykens et al. evaluated the auscultatory method and pH measurement with a pH cut-off point of 5.5 after tube insertion and compared this with the ‘gold standard’: an abdominal X-ray [6]. They indicated that the auscultatory method is unreliable. In this study, the incidences of adjustment after chest X-ray were 39.3 %. Regarding cases of the adjustment after chest X-ray, over tube length cases was 90.9 % (over length: 5.3 ± 1.8 cm) and under tube length cases was 9.1 % (under length: -10 ± 0.0 cm). We consider that the chest X-ray should be useful for positioning in nasogastric tube insertion on general anesthesia.
NEX is incorrect because it only approximates the nose to gastro-esophageal junction distance and is therefore too short [7]. In this study, height correlated with length of nasogastric tube using gastric babble sound for positioning in nasogastric tube insertion on general anesthesia (R = 0.505; p = 0.000) and length after adjustment using chest X-ray (R = 0.494; p = 0.000). We consider that height should not be useful for positioning in nasogastric tube insertion on general anesthesia. There were several limitations of this study. The sample was relatively small. Further research is necessary to validate these results.
Conclusion
This study compared gastric babble sound with chest X-ray for positioning in nasogastric tube insertion on general anesthesia for oral and maxillofacial patients. The chest X-ray seems to be useful for positioning in nasogastric tube insertion on general anesthesia for oral and maxillofacial patients.
Conflicts of interest
The authors declare that they have no conflict of interest.
Article Info
Article Type
Research ArticlePublication history
Received: Thu 26, Dec 2019Accepted: Tue 07, Jan 2020
Published: Sat 11, Jan 2020
Copyright
© 2023 Ichiro Ogura. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDOA.2019.01.06
Author Info
Fumi Mizuhashi Hisato Saegusa Ichiro Ogura Makoto Oohashi Toru Oshikiri Yoshihiro Sugawara
Corresponding Author
Ichiro OguraDepartment of Oral and Maxillofacial Radiology, The Nippon Dental University School of Life Dentistry at Niigata, Niigata, Japan
Figures & Tables
Table 1: Characteristics of oral and maxillofacial patients with nasogastric tube on general anesthesia.
|
Parameter |
Number of patients |
Mean ± standard deviation |
Range |
|
Age (years) |
56 (100 %) |
61.4 ± 19.8 |
17 - 85 |
|
Gender |
|
|
|
|
Men |
21 (37.5 %) |
|
|
|
Women |
35 (62.5 %) |
|
|
|
Primary diseases |
|
|
|
|
Neoplasms |
37 (66.1 %) |
|
|
|
Inflammatory conditions |
7 (12.5 %) |
|
|
|
Jaw deformity |
7 (12.5 %) |
|
|
|
Trauma |
5 (8.9 %) |
|
|
|
Hight (cm) |
56 (100 %) |
160.7 ± 10.5 |
142.1-182.0 |
|
Weight (kg) |
56 (100 %) |
59.8 ± 14.7 |
37.3-133.0 |
|
BMI (Body Mass Index) |
56 (100 %) |
23.0 ± 4.1 |
16.5-40.2 |
|
Length of nasogastric tube (cm) |
|||
|
Gastric babble sound |
56 (100 %) |
53.4 ± 5.0 |
45 - 70 |
|
Chest X-ray |
56 (100 %) |
51.9 ± 3.8 |
43 - 60 |
|
Adjustment after chest X-ray |
|||
|
Absence |
34 (60.7 %) |
|
|
|
Presence |
22 (39.3 %) |
|
|
|
Over tube length (cm) |
20 (90.9 %) |
5.3 ± 1.8 |
3 - 10 |
|
Under tube length (cm) |
2 ( 9.1 %) |
-10 ± 0.0 |
-10 |
Table 2: Relationship between height, weight, BMI and length of nasogastric tube.
|
Parameter |
Correlation coefficient (R) in length of nasogastric tube |
|
|
|
Gastric babble sound |
Chest X-ray |
|
Height |
0.505 (p = 0.000) |
0.494 (p = 0.000) |
|
Weight |
0.261 (p = 0.052) |
0.255 (p = 0.058) |
|
BMI (Body Mass Index) |
0.000 (p = 0.999) |
-0.026 (p = 0.850) |
References
- Sanaie S, Mahmoodpoor A, Najafi M (2017) Nasogastric tube insertion in anaesthetized patients: a comprehensive review. Anaesthesiol Intensive Ther 49: 57-65. [Crossref]
- Ozer S, Benumof JL (1999) Oro- and nasogastric tube passage in intubated patients. Anesthesiology 91: 137-143. [Crossref]
- Zhao W, Ge C, Zhang W, Sun Z, Li X (2018) The important role of positioning in nasogastric tube insertion in unconscious patients: a prospective, randomized, double-blind study. J Clin Nurs 27: e162-e168. [Crossref]
- Taylor S, Allan K, McWilliam H, Manara A, Brown J et al. (2014) Confirming nasogastric tube position with electromagnetic tracking versus pH or X-ray and tube radio-opacity. Br J Nurs 23: 354-358. [Crossref]
- Isik A, Firat D, Peker K, Sayar I, Idiz O et al. (2014) A case report of esophageal perforation: complication of nasogastric tube placement. Am J Case Rep 15: 168-171. [Crossref]
- Boeykens K, Steeman E, Duysburgh I (2014) Reliability of pH measurement and the auscultatory method to confirm the position of a nasogastric tube. Int J Nurs Stud 51: 1427-1433. [Crossref]
- Taylor SJ, Allan K, McWilliam H, Toher D (2014) Nasogastric tube depth: the ‘NEX’ guideline is incorrect. Br J Nurs 23: 641-644. [Crossref]
- Zatelli M, Vezzali N (2017) 4-point ultrasonography to confirm the correct position of the nasogastric tube in 114 critically ill patients. J Ultrasound 20: 53-58. [Crossref]
- Metheny NA, Stewart BJ, Smith L, Yan H, Diebold M et al. (1999) pH and concentration of bilirubin in feeding tube aspirates as predictors of tube placement. Nurs Res 48: 189-197. [Crossref]
- Christen S, Hess T (1996) Is a clinical positional control for nasogastric tubes good enough? A prospective study of 43 patients. Dtsch Med Wochenschr 121: 1119-1122. [Crossref]
- Galbois A, Vitry P, Ait-Oufella H, Baudel JL, Guidet B et al. (2011) Colorimetric capnography, a new procedure to ensure correct feeding tube placement in the intensive care unit: an evaluation of a local protocol. J Crit Care 26: 411-414. [Crossref]
