Case Report: The Importance of Cystoscopic Evaluation and Management of Iatrogenic Lower Ureteric Injuries
A B S T R A C T
Four days after emergency caesarean section, a 26-year-old lady presents with severe right flank pain and is found to have right hydronephrosis. A right nephrostomy was inserted, but antegrade stent insertion failed. Cystoscopy revealed two sutures obstructing the right intramural ureter. These sutures were removed via the cystoscope using Holmium LASER. Immediate and follow up investigations showed resolution of the injury and normal urinary drainage. This case highlights the importance of cystoscopic assessment of iatrogenic lower ureteric injuries, and its role in their management.
Introduction
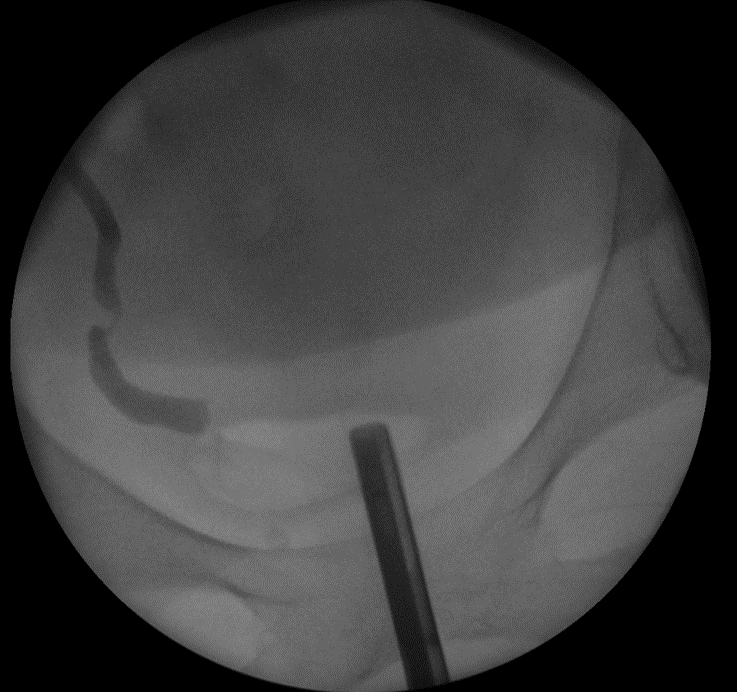
A 26-year-old previously nulliparous woman underwent caesarean section (CS). There were no perceived intra-operative complications. Day four post-operatively she returned complaining of severe right flank pain. She had no signs of sepsis and the laboratory tests revealed elevation of creatinine (140μmol/L). A contrast enhanced computerised tomography (CT) Urogram revealed right hydroureter and hydronephrosis (Figure 1) with a transition point in the right lower ureter. The differential diagnosis was of iatrogenic peri-ureteric inflammation or injury to the right distal ureter. On the ninth post-operative day, she underwent attempted insertion of an antegrade right ureteric stent. The interventional radiologist was unable to pass a guide wire past a demonstrable lower ureteric stricture (Figure 2). A nephrostomy was inserted. After multi-disciplinary discussion, with consideration of the difficulties of nephrostomy management in a new mother, we proceeded to rigid cystoscopy under general anesthetic (GA) to attempt retrograde ureteric stent insertion, or potentially a “rendez-vouz” mixed antegrade and retrograde approach.
Intra-Operative Findings
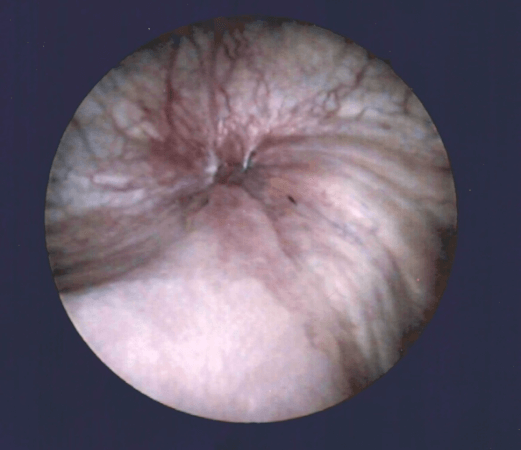
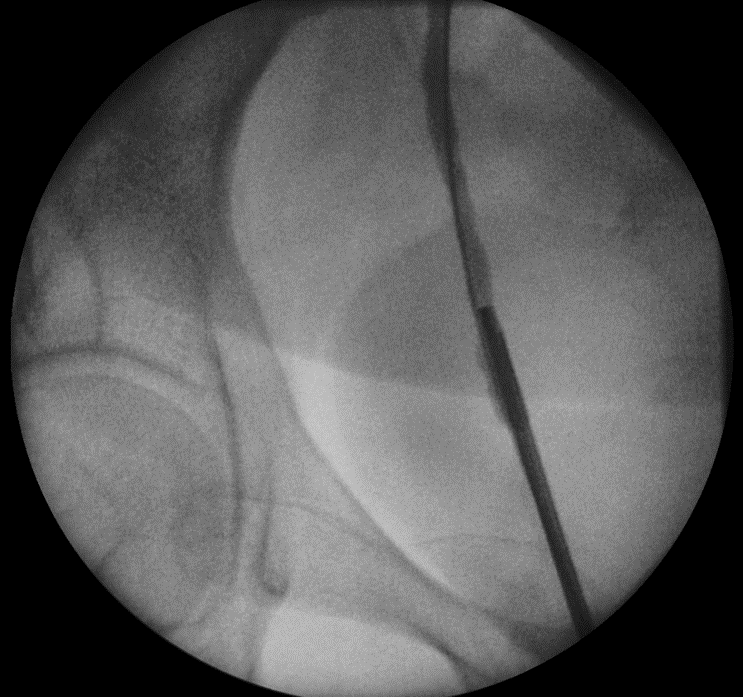
Rigid cystoscopy was performed thirteen days after her caesarean section. Cystoscopy revealed two sutures proximal to the right ureteric orifice causing an anterior ridge of the bladder wall in the region of the intra-mural right ureter (Figure 3). An antegrade right nephrostogram revealed this to be the site of ureteric obstruction (Figure 4). With difficulty and the aid of a ureteric catheter, we passed a guide wire retrograde past this point of obstruction to the right kidney. A 400 micrometer Holmium LASER fiber was inserted via the cystoscope and used to break each suture at its most superficial point, with great care taken to avoid laser injury to the underlying bladder mucosa. Sutures were removed with biopsy forceps. This resulted in resolution of the previously seen ridge, and efflux of urine from the right ureteric orifice. Antegrade (Figure 5) and retrograde ureterograms confirmed free flow of contrast. A 7Fr/24mm right ureteric stent was inserted and the right nephrostomy was removed. The blood parameters, including creatinine, normalized two days after our procedure, her pain improved, and she was discharged.
Figure 1: CT Urogram showing right hydroureter and hydronephrosis.
Figure 2: Fluoroscopy image of antegrade right ureterography with attempted guide wire insertion passed lower ureteric stricture. The interventional radiologist was unable to pass this stricture.
Figure 3: Cystoscopy image of two sutures (red arrow) obstructing the right intramural ureter proximal to the right ureteric orifice (green arrow), causing it to be distorted.
Follow Up
3 months later, our patient returned for elective cystoscopy, removal of right ureteric stent, retrograde ureterography and ureteroscopy. The area where the sutures had previously injured the intramural ureter and bladder appeared cystoscopically normal. Retrograde ureterography revealed a normal passage of contrast through a good caliber lower ureter (Figure 6). Ureteroscopy revealed a macroscopically normal right ureter. She did not therefore require replacement of her ureteric stent. She will return for MAG-3 Renogram to ensure there is no delayed stricture in 6 months’ time, with a view to possible discharge.
Figure 4: Antegrade and retrograde ureterograms intra operatively prior to removing sutures. Red arrow shows transition point of contrast in correspondence with macroscopic findings of sutures here.
Figure 5: Antegrade ureterogram following removal of sutures. No transition point present.
Figure 6: Follow up retrograde right ureterography via ureteroscope inserted in right ureteric orifice. Normal flow of contrast retrogrades and macroscopically the ureter looked normal at the previous site of injury.
Discussion
This case highlights the benefit of retrograde endoscopic assessment of lower ureteric injuries. Our novel technique allowed for the early, minimally invasive correction of the ureteric injury using a LASER without the need for major reconstructive surgery. Cesarean sections are increasing in incidence in the UK [1]. This exposes the patient to increased risks of injury to urinary tract including ureteric injury, fistula and retroperitoneal urinoma formation. The incidence of ureteric injury in obstetric surgery is variable, between 0.03 and 0.35% [2]. The incidence is higher in gynaecological and colorectal surgery, and the lower ureter is most commonly affected [2, 3]. Management of these injuries is best done immediately intra operatively, prior to the onset of inflammation and scarring, but 50-70% present in the post-operative period [3]. Early management focuses on de-obstructing the kidney proximal to the damaged ureter with a nephrostomy [4]. A ureteric stent could be inserted antegradely or retrogradely and has the ability to help de-obstruct the damaged ureter, or potentially heal the injury. As demonstrated in our case, insertion of the stent is likely to be difficult. Successful antegrade insertion may negate the need for a cystoscopy.
Delayed management can be endoscopic, laparoscopic or open. Endoscopic procedures can include long term ureteric stents, for which 4 in 5 patients will have stent related symptoms, or balloon dilatation of the ureteric strictures [5]. Endoscopic options can only be considered if a stent is already in place [3]. Reconstructive surgery depends on the anatomical site; in the lower ureter this is most commonly done via ureteroneocytostomy with or without a vesico-psoas hitch, used to bridge the gap of a longer affected segment. There are significant drawbacks to having a nephrostomy at any stage of life, including pain, urine leakage from urine stoma bags, difficulty changing bags, infections and blockage [5]. These complications will likely be amplified in a new mother tending to her child. Our patient only required a nephrostomy for 4 days and a ureteric stent for 3 months. Retrograde endoscopic assessment of lower ureteric injuries can aid both diagnosis and management early in iatrogenic ureteric injuries. We avoided the need for major surgery, and early follow up has shown resolution of her injury. In future practice, we will perform cystoscopy/retrograde ureterogram in the initial management iatrogenic lower ureteric injuries.
Article Info
Article Type
Case ReportPublication history
Received: Fri 14, Feb 2020Accepted: Fri 28, Feb 2020
Published: Fri 13, Mar 2020
Copyright
© 2023 Struan Gray. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2020.01.06
Author Info
Corresponding Author
Struan GrayThe Royal Bolton NHS Foundation Trust, Minerva Road, Farnworth, Bolton, UK
Figures & Tables



References
- Wise J (2018) Alarming global rise in caesarean births, figures show. BMJ 363: k4319. [Crossref]
- Rajasekar D, Hall M (1997) Urinary tract injuries during obstetric intervention. Br J Obstet Gynaecol 104: 731-734. [Crossref]
- Burks FN, Santucci RA (2014) Management of iatrogenic ureteral injury. Ther Adv Urol 6: 115-124. [Crossref]
- Lask D, Abarbanel J, Luttwak Z, Manes A, Mukamel E (1995) Changing trends in the management of iatrogenic ureteral injuries. J Urol 154: 1693-1695. [Crossref]
- Joshi HB, Stainthorpe A, MacDonagh RP, Keeley FX, Timoney AG et al. (2003) Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J Urol 169: 1065-1069. [Crossref]
