Case Report: A Case of Acquired Symptomatic Arachnoid Cyst in an Elderly Patient
A B S T R A C T
Arachnoid cysts comprise approximately 1% of all intracranial space-occupying lesions and etiologies of its formation are believed to be both congenital and acquired. However, very few cases of symptomatic acquired arachnoid cyst have been reported so far in the elderly. Here we report a case of acquired symptomatic arachnoid cyst in an elderly patient.
We present here a case of 75 years-old male presenting with seizure-like episode. He was diagnosed bilateral subdural hygroma and left-sided arachnoid cyst by CT. However, he was performed CT 12 years ago, which showed no arachnoid cyst then. We performed microsurgical cyst excision and fenestration to the subarachnoid space. Postoperatively his condition has been excellent so far, with no cyst recurrence.
Keywords
Symptomatic acquired arachnoid cyst, elderly, seizure, microsurgical cyst excision
Introduction
Arachnoid cysts comprise approximately 1% of all intracranial space-occupying lesions and although the exact mechanism of its formation is unknown, both congenital and acquired mechanisms are widely believed to be involved [1, 2]. According to a congenital etiology, there is a hypothesis that the cyst can develop from the splitting or duplication of the arachnoid membrane [3]. In acquired arachnoid cysts, on the other hand, trauma and meningitis are believed to be major contributing factors [4]. However, very few cases of symptomatic acquired arachnoid cyst have been reported so far in the elderly [5]. Here we report a case of acquired symptomatic arachnoid cyst in an elderly patient.
Case Report
We present here a case of 75 years-old male with history of hypertension, dyslipidemia, aortic dissection, and bilateral subdural hygroma, presenting with a seizure-like episode. The patient denies any past head trauma or meningitis. While he was sleeping, he suddenly started to scream and became restless and unresponsive. He was brought to our hospital by ambulance. During transfer, his consciousness returned to baseline and he could speak normally. He was unconscious for approximately 30 minutes.
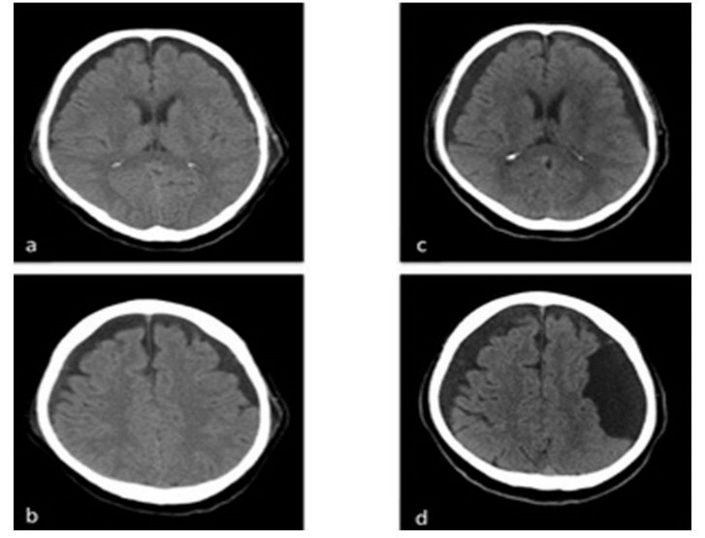
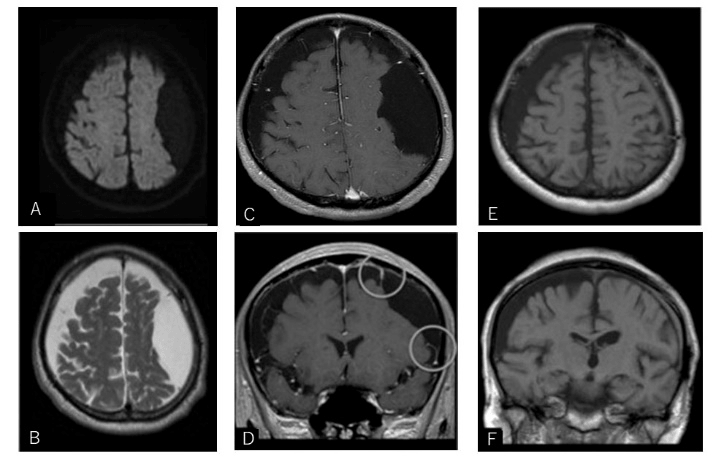
On admission to our hospital, he was completely neurologically intact with Glasgow Coma Scale score of 15 (E4V5M6). He was previously performed computed tomography (CT) 12 years ago for screening during his perioperative period of aortic dissection, which showed bilateral subdural hygroma, but no arachnoid cyst (Figure 1A, B). However, CT on admission showed a cystic lesion (40mm x 80mm) in left convexity in addition to bilateral subdural hygroma (Figure 1C, D). On magnetic resonance imaging (MRI), the cystic lesion showed hypo-intensity on diffusion weighted imaging (DWI) (Figure 2A) and almost iso-intensity to cerebrospinal fluid on T1 and T2 (Figure 2B-D). The cyst wall was not highlighted with Gadolinium (Figure 2C, D). Anterior coronal slice showed that the cyst extended all the way from near the longitudinal fissure to the sylvian fissure (Circles in Figure 2D). Taking into account all available information, we diagnosed him with acquired symptomatic arachnoid cyst. Because the cyst covered a large area of brain surface, we thought it would be better to resect as much of the cyst wall as possible, and therefore we performed microsurgical cyst excision. We performed an unusually extensive left frontotemporal craniotomy, all the way down from 2 cm left to the midline to the point where the Sylvian fissure can be seen. The characteristic capsule for chronic subdural hematoma was not present. We resected as much of the cyst wall as possible and cut the cyst membrane near the Sylvian fissure and the longitudinal fissure to connect to the basal cistern. During the operation, we confirmed that the compressed brain was returning back to the normal size due to decreased pressure.
The patient did develop one seizure on postoperative day 3, therefore we put him on 1000mg/day levetiracetam. MRI taken 6 months after surgery showing disappearance of the cyst and mass effect (E and F). During the 2 years since the surgery, there has been no cyst recurrence.
The value of 2D iU/S in assessing extent of resection of intracranial tumour remains unclear due to the absence of large case series and long-term follow-up data. Potentially, it could be used as a cheaper alternative to iMRI and post-operative MRI in resource poor settings, but clarification of whether it gives comparable data to the surgeon on extent of resection is still lacking. In this study, we aim to evaluate iU/S as an adjunct for resection of gliomas, aiming to clarify whether the extent of resection as measured by iU/S is comparable to the extent of resection as measured on the gold standard of a post-operative MRI scan.
Figure 1: Computed tomography (CT) performed 12 years ago demonstrated bilateral subdural hygroma, but no arachnoid cyst (A and B). CT on admission showed a left-sided cystic lesion in addition to bilateral subdural hygroma (C and D).
Figure 2: Magnetic resonance imaging (MRI) on admission (A-D); diffusion weighted imaging (A), T2 weighted image (B), T1 weighted image with Gadolinium axial image (C), and coronal image (D). MRI taken 6 months after operation: T1 weighted axial image (E), and coronal image (F)The left front-parietal cystic lesion showed with low intensity on diffusion weighted imaging (A), and almost with the same intensity as cerebrospinal fluid on T2 (B) and T1 (C and D). The cyst wall is not highlighted with Gadolinium (C and D). Anterior slice (D) revealed that the cyst extends all the way from near the longitudinal fissure to the sylvian fissure (Circles in Figure D). MRI taken 6 months after surgery illustrated disappearance of the cyst and mass effect (E and F). Sulci was seen equally well on both sides.
Discussion
Regarding acquired pediatric symptomatic arachnoid cyst, there are only a few case reports conclusively confirmed by previously taken images showing no arachnoid cyst. Therefore, some neurosurgeons believe that among the cases of arachnoid cyst categorized as congenital, there is actually a certain number of acquired cases because a trauma during the perinatal period or infancy can be a causative factor [2].
As for geriatric acquired symptomatic arachnoid cyst, there have been at least 60 cases reported so far [5], but it still appears to be very rare. Of note, we cannot rule out the possibility that among these approximately 60 cases, there are, mixed with the truly acquired ones, some cases where the cyst started congenitally but for certain reasons, it enlarged and became symptomatic only as the patient grew older. Our case seems extremely rare as we could conclusively prove that there was no cyst on previous imaging, and therefore we can say with absolute certainty it was acquired. Despite our best effort we could not find any other published case of geriatric symptomatic arachnoid cyst that can confirm without doubt its acquired origin. Although the intricacies of the mechanism of cyst formation remain unclear, we believe that a very trivial past trauma of which the patient was not aware was the contributing factor in this case. As for the formation of arachnoid cyst in children, there is a report that arachnoid cyst occurs 10 months to 6.2 years (mean 2.2 years) after head trauma [2]. To the contrary, there is no report about posttraumatic arachnoid cyst formation in the elderly, and it seems that chronic subdural hematoma, rather than arachnoid cyst, develops after head trauma in the elderly. Generally, asymptomatic arachnoid cysts without brain shift or increased intracranial pressure should be managed conservatively, while symptomatic cases, especially those associated with intracranial hypertension, hydrocephalus, and focal neurologic signs, are good candidates for surgery [2, 6]. Microsurgical cyst excision, endoscopic surgery, and cyst-peritoneal shunting are the major surgical options. Microsurgical cyst excision is preferred especially when a cyst is located in the cerebral convexity [7]. Although wide surgical removal is available, this method is most invasive and we cannot neglect the relatively high complication rates of cranial nerve palsy, cerebrospinal fluid leak, subdural hematoma, and infection [6]. Endoscopic surgery, on the other hand, is less invasive and has lower complication rate although it is at least as effective as microsurgical cyst excision [6]. Therefore, some authors recommend endoscopic surgery as a first line surgical option [2, 6]. However, it makes wide removal hard to achieve and it is difficult to control hemostasis with usual methods such as bipolar cautery because of limited visual access to surgical site [6, 7]. Cyst-peritoneal shunt is less invasive as well and is reported to be effective especially in children, however, selection of candidates should be prudent because of the possible specific complications of infection, shunt malfunction and dependency [2, 6, 7].
Although, it was difficult to decide the best treatment option, we determined it would be better to resect the extended cyst wall as widely as possible in order to prevent recurrence. Postoperatively, the mass sign remarkably disappeared immediately, and there have been no recurrences since.
Conclusion
We present a rare case of acquired symptomatic arachnoid cyst in an elderly patient, who was successfully treated by microsurgical cyst excision and fenestration to the subarachnoid space.
Funding
None.
Declaration of Interest
None.
Author Contributions
All co-authors are participating clinical investigators.
Ethics
The institutional review board approved this retrospective study and informed patient consent was not required.
Article Info
Article Type
Case ReportPublication history
Received: Tue 29, Oct 2019Accepted: Wed 13, Nov 2019
Published: Wed 27, Nov 2019
Copyright
© 2023 Ryosuke Sawaya. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.06.02
Author Info
Daisuke Shimbo Katsuyuki Asaoka Kazuki Uchida Koji Itamoto Masaaki Hokari Ryosuke Sawaya
Corresponding Author
Ryosuke SawayaDepartment of Neurosurgery, Teine Keijinkai Hospital, Sapporo, Japan
Figures & Tables
References
- Robinson RG (1971) Congenital cysts of the brain: Arachnoid malformations.Neurol Surg 4: 133–173.
- Choi JU, Kim DS (1998) Pathogenesis of arachnoid cyst (Congenital or traumatic). Pediatr Neurosurg 29: 260-266. [Crossref]
- Starkman SP, Brown TE, Linell EA (1958) Cerebral arachnoid cysts. J Neuropathol Exp Neurol 17: 484-500. [Crossref]
- Fobe JL, Nishikuni K, Gianni MA (1998) Evolving magnetic resonance spinal cord trauma in child from hemorrhage to intradural arachnoid cyst. Spinal Cord 36: 864-866. [Crossref]
- Suzuki M, Tamaki T, Toda S, Tsuchiya M, Kogure K et al. (2009) Delayed Recurrent Arachnoid Cyst of the Occipital Convexity in an Elderly Woman. Neurol Med Chir (Tokyo) 49: 134-137 [Crossref]
- Eun-Jung Lee, Young-Shin Ra (2012) Clinical and Neuroimaging Outcomes of Surgically Treated Intracranial Cysts in 110 Children. J Korean Neurosurg Soc 52: 325-333 [Crossref]
- Bulent Duz, Serdar Kaya, Mehmet Daneyemez, Engin Gonul (2012) Surgical Management Strategies of Intracranial Arachnoid Cysts: A single Institution Experience of 75 Cases. Turk Neurosurg 22: 591-598 [Crossref]
