Arthroscopic Management of Pigmented Villonodular Synovitis of the Hip: A Case Report
A B S T R A C T
Background: Pigmented villonodular synovitis, particularly of the hip joint, has been historically treated via open synovectomy. However, an arthroscopic approach to management has been trailed successfully in recent years and has demonstrated encouraging outcomes.
Case Presentation: We report the case of a 17-year-old man with pigmented villonodular synovitis of the right hip who underwent arthroscopic treatment. He remains well 5 years later with no signs of recurrence. We discuss the advantages and disadvantages of arthroscopically managed pigmented villonodular synovitis as well as the recent literature surrounding this topic. We also explain a technical tip during hip arthroscopy to access these difficult lesions.
Conclusion: Arthroscopy can be used for hip pigmented villonodular synovitis treatment. These lesions may also be accessed by extending the hip to 10 degrees and releasing the traction. There is evidence to suggest that arthroscopically managed pigmented villonodular synovitis carries better outcomes and lower morbidity rates compared to an open approach in suitable cases.
Keywords
Pigmented villonodular synovitis, arthroscopy, synovectomy
Background
Pigmented villonodular synovitis (PVNS) is a rare, benign proliferation lesion of the synovium primarily affecting large joints. With an incidence of around 1.8 million, its aetiology remains unclear [1, 2]. It has traditionally been treated via open synovectomy, regardless of the affected joint [3]. However, an arthroscopic approach to management has been adopted for localised nodular lesions in recent years due to the advantages it poses over an open approach. With advancing arthroscopic tools, surgical technique, and careful patient selection, there is strong evidence to suggest that complication rates with an arthroscopic approach are <1% [4]. Further evidence also suggests a lower recurrence rate with an arthroscopic approach, with a case series of 13 patients with arthroscopically managed hip PVNS reporting a recurrence rate of 7.7% (mean follow-up time of 63 months). In comparison, a systematic review of PVNS treated by open synovectomy, including a total of 81 patients, reported a recurrence rate of 17.8%. Mean time to revision was also significantly longer in patients who underwent synovectomy with arthroplasty (4.5 years) compared to those who underwent synovectomy alone (3.9 years) [5]. Multiple other case reports and case series have also reported good outcomes at long-term follow-up in arthroscopically managed PVNS, including lower recurrence rates, better preservation of joint function, and fewer post-operative complications in some suitable cases [6-9].
However, certain lesions may prove difficult to access arthroscopically depending on their location, such as the hip. In such cases, technical modifications in applying traction may be necessary to allow for introduction of the arthroscope and other instruments to the area. However, the traction itself can cause soft tissue damage either directly or as a result of compression of the perineal area [10]. Furthermore, there is risk of damaging the sciatic nerve given its proximity. Herein, we describe a case of successful arthroscopically managed hip PVNS in which a technical tip was utilised to access the lesion.
Case Study
A 17-year-old gentleman presented with right-sided lower back pain of a few months’ duration, including pain at night. He managed his back and hip pain with occasional ibuprofen. His usual medications included etoricoxib and omeprazole, and no allergies were noted. Examination revealed him to be very tall and thin. Passive flexion of the hips was limited by lower back pain to 110°. Hip extension in the prone position was also restricted to 10-15° secondary to lower back discomfort. Abduction and adduction were globally reduced, and the entirety of the sacrum was tender, particularly over the sacroiliac joints. There was no pain in the hip itself. Gait examination revealed a relatively normal foot progression angle and a degree of stiffness to both legs, but no antalgia. Otherwise, impingement provocation tests were negative, and there was no elicitable psoas clunk on bicycle testing.
MR imaging of the right hip raised the possibility of an intra-articular lesion, and this was therefore reimaged 2 months later via MR arthrogram. This revealed a 22x8x14mm intracapsular nodular lesion in the posterior right hip, although this was felt not to be the cause of his symptoms. This raised the faint suggestion of an intra-articular synovial sarcoma. An incidental small anterior labral tear was also noted. No calcification was seen on the x-ray. Following two discussions at our local multidisciplinary team meetings, the decision was made for hip arthroscopic assessment and biopsy, as CT-guided biopsy would have been challenging. The patient had also been consented for open hip surgery should the arthroscopy fail.
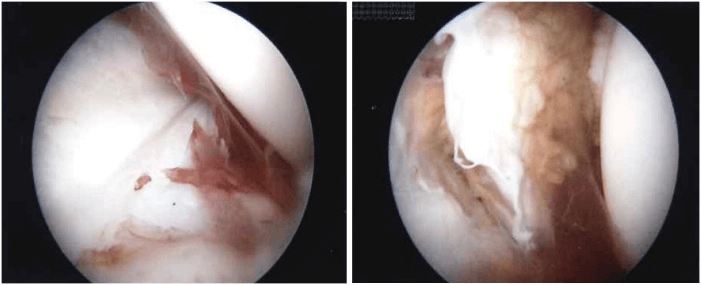
Figure 1: A tumor is identified during the arthroscopy.
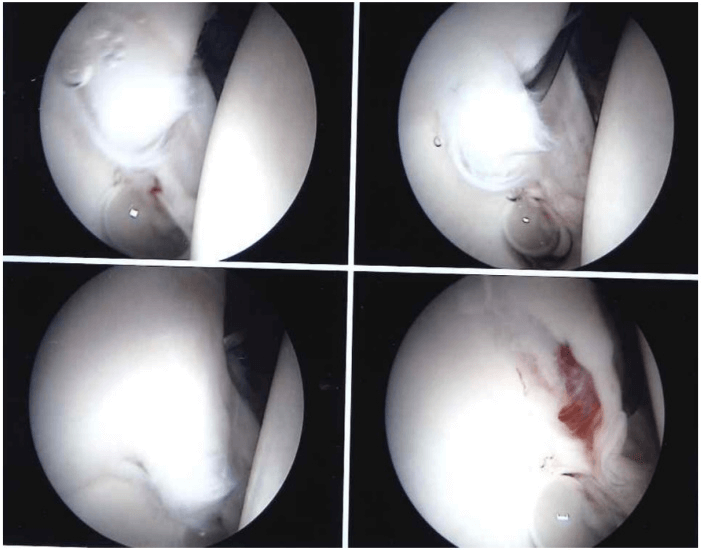
Figure 2: A small labrum tear as well as the tumor can be visualized via the central compartment.
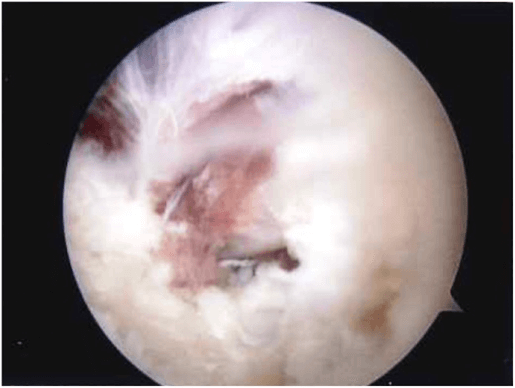
The operation was performed under general anaesthetic, and local anaesthetic was inserted in the portal site before entry. Two posterolateral, one anterior, and one superior port was used to assess the hip joint and lesion. The posterior compartment was visualized via the superior port and accessed via a posterolateral port. A nodular lesion was identified (Figure 1), and an irregular piece of tan tissue measuring 8x7x6mm was taken and sent for histology. As a technical modification, during hip arthroscopy, the traction had to be reduced, and the hip put in 10 degrees of extension and a new posterolateral portal was used to access the nodule. This manoeuvre allowed for some slack within the hip to allow insertion of the instruments. In the normal position of traction during hip arthroscopy, the lesion could not be accessed. This portal had to be inserted very carefully bearing in mind the proximity of the sciatic nerve. Although not a routine portal, it is indicated in cases such as these. Examination of the central compartment revealed a small anterior labrum tear (Figure 2), but no labrum detachment. There was also an area of fibrous thickening around the ligamentum teres. Arthrowand was used for ablation of the labrum tear and the remaining lesion (Figure 3). The operation lasted a total of approximately 2.5 hours.
Figure 3: Tumor has been removed, and the lesion has been cauterized.
Histology revealed foci of mononuclear multinucleate macrophages in a dense fibrous stroma. Some cells contained hemosiderin and other lipids, and there was a suggestion that the disease process extended into synovial villi in some places. The appearances were in keeping with nodular synovitis with features suggestive of PVNS. Our patient was observed overnight and discharged the following day. He made a complete recovery without any need for analgesia or physiotherapy and remains well 5 years following discharge without any recurrence.
Discussion
PVNS is a rare, benign proliferation lesion of the synovium primarily affecting large joints. With an incidence of around 1.8 million, its aetiology remains unclear [1, 2]. It has traditionally been treated via open synovectomy, regardless of the affected joint [3]. However, an arthroscopic approach to management has been adopted for localised nodular lesions in recent years due to the advantages it poses over an open approach. With advancing arthroscopic tools, surgical technique, and careful patient selection, there is strong evidence to suggest that complication rates with an arthroscopic approach are <1% [4]. Further evidence also suggests a lower recurrence rate with an arthroscopic approach, with a case series of 13 patients with arthroscopically managed hip PVNS reporting a recurrence rate of 7.7% (mean follow-up time of 63 months). In comparison, a systematic review of PVNS treated by open synovectomy, including a total of 81 patients, reported a recurrence rate of 17.8%. Mean time to revision was also significantly longer in patients who underwent synovectomy with arthroplasty (4.5 years) compared to those who underwent synovectomy alone (3.9 years) [5]. Multiple other case reports and case series have also reported good outcomes at long-term follow-up in arthroscopically managed PVNS, including lower recurrence rates, better preservation of joint function, and fewer post-operative complications in some suitable cases [6-9].
However, certain lesions may prove difficult to access arthroscopically depending on their location, such as the hip. In such cases, technical modifications in applying traction may be necessary to allow for introduction of the arthroscope and other instruments to the area. However, the traction itself can cause soft tissue damage either directly or as a result of compression of the perineal area [10]. Furthermore, there is risk of damaging the sciatic nerve given its proximity.
In this case report, we describe the successful arthroscopic approach to the management of nodular synovitis/PVNS of the hip. Our patient presented with lower back pain exacerbated by sitting and standing and relieved by laying down. He also complained of night pain which, without ibuprofen, would wake him from sleep. Although clinically and radiographically suspected to be a labral tear, a nodular lesion was also visualized, although this was not felt to be the cause of his symptoms. Interestingly, our patient gave a history of bilateral pneumothoraces earlier that year which were treated with a pleurodesis procedure. A thoracic epidural was given at the time, and symptoms started soon after.
The lesion was situated in the posterior part of the right hip, making access in the normal position of traction difficult. Indeed, the lesion proved unreachable, and a technical adjustment was therefore necessary. Traction was reduced and the hip extended to around 10 degrees, and a new posterolateral port was established. This allowed for successful access to the nodule, with the superior port being used for visualization of the lesion. Interestingly, a small anterior labrum tear was identified upon examination of the central compartment. Given the nature of our patient’s symptoms, this labrum tear may have been the root cause, with the PVNS being completely incidental. Arthrowand was used for ablation of the lesions, and a sample taken for histology.
Our patient was discharged the following day and required minimal analgesia. He remains symptom free with no signs of recurrence 5 years later. Baseline function returned to normal without any need for physiotherapy. Assessment after 1 year revealed that external rotation of the right hip was reduced by approximately 25% compared to the left. Otherwise, there was full range of motion, and the remainder of the examination was unremarkable. The present case highlights the value of arthroscopic treatment of PVNS and contributes to the current evidence for this method of management. We particularly note the short hospital stay, resolution of symptoms, lack of post-operative complications, and lack of recurrence after 5 years. Utilizing our technical tip allowed for open synovectomy to be avoided, which could have resulted in a less favourable outcome.
Conclusion
Arthroscopy is an effective treatment option for PVNS of the hip. We have also shown that extending the hip to 10 degrees and releasing the traction can allow for access to these lesions. Arthroscopically managed PVNS has been shown to have more positive outcomes and lower morbidity rates compared to an open approach in suitable cases.
Acknowledgements
We would like to thank all staff members involved in the patient’s care.
Abbreviation
PVNS: Pigmented Villonodular Synovitis
Author Contributions
OE drafted the manuscript. SS and AP participated in the diagnosis and treatment of this patient. AP revised the manuscript. All authors approved the final version of the manuscript.
Funding
None.
Availability of Data and Materials
None.
Ethical Approval
The privacy of the patient was considered, and the manuscript does not include any identifying information.
Consent
Verbal informed consent was obtained from the patient for the publication of this report and accompanying images.
Competing Interests
None.
Article Info
Article Type
Case ReportPublication history
Received: Tue 03, Nov 2020Accepted: Sat 14, Nov 2020
Published: Wed 02, Dec 2020
Copyright
© 2023 Ashok S Paul. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.12.04
Author Info
Omar El-Omar Sanat Shah Ashok S Paul
Corresponding Author
Ashok S PaulThe Regional Sarcoma Centre, Manchester Royal Infirmary, Manchester, UK
Figures & Tables
References
- Temponi EF, Barros AAG, Paganini VO, Barbosa VAK, Badet R et al. (2017) Diffuse pigmented villonodular synovitis in knee joint: diagnosis and treatment. Rev Bras Ortop 52: 450-457. [Crossref]
- Kapoor C, Jhaveri M, Soni R, Shah M, Rathi P et al. (2016) Pigmented Villonodular Synovitis of the Knee Joint: A Case Report. Cureus 8: e816. [Crossref]
- Xie GP, Jiang N, Liang CX, Zeng JC, Chen ZY et al. (2015) Pigmented Villonodular Synovitis: A Retrospective Multicenter Study of 237 Cases. PLoS One 10: e0121451. [Crossref]
- Harris JD, McCormick FM, Abrams GD, Gupta AK, Ellis TJ et al. (2013) Complications and Reoperations During and After Hip Arthroscopy: A Systematic Review of 92 Studies and More Than 6,000 Patients. Arthroscopy 29: 589-595. [Crossref]
- Levy DM, Haughom BD, Nho SJ, Gitelis S (2016) Pigmented Villonodular Synovitis of the Hip: A Systematic Review. Am J Orthop 45: 23-28. [Crossref]
- Willimon SC, Schrader T, Perkins CA (2018) Arthroscopic Management of Pigmented Villonodular Synovitis of the Hip in Children and Adolescents. Orthop J Sports Med 6: 232596711876311. [Crossref]
- Dines JS, DeBerardino TM, Wells JL, Dodson C, Shindle M et al. (2007) Long-term Follow-up of Surgically Treated Localized Pigmented Villonodular Synovitis of the Knee. Arthroscopy 23: 930-937. [Crossref]
- Hufeland M, Gesslein M, Perka C, Schröder J (2018) Long-term outcome of pigmented villonodular synovitis of the hip after joint preserving therapy. Arch Orthop Trauma Surg 138: 471-477. [Crossref]
- Aurégan JC, Bohu Y, Lefevre N, Klouche S, Naouri J et al. (2013) Primary arthroscopic synovectomy for pigmented villo-nodular synovitis of the knee: Recurrence rate and functional outcomes after a mean follow-up of seven years. Orthop Traumatol Surg Res 99: 937-943. [Crossref]
- Frandsen L, Lund B, Nielsen TG, Lind M (2017) Traction-related problems after hip arthroscopy. J Hip Preserv Surg 4: 54-59. [Crossref]
