Journals
A rare case of spontaneously resolved gastric outlet obstruction
A B S T R A C T
Purpose: Gastric outlet obstruction (GOO) rarely occurs after surgery. Even rarer, in cases of living donor liver transplantation (LDLT). Adhesive bands causing obstruction can be managed conservatively, failing so, will require surgical intervention. We describe a rare case of GOO due to adhesion band that resolved spontaneously after more than a month of conservative management.
Method: A 71-year-old gentleman undergone living donor liver transplantation (LDLT) in our institution. 2 months post-operatively, he developed gastric outlet obstruction. Water soluble contrast meal performed revealed hold up of contrast in first and second portion of duodenum (D1/D2) likely due to adhesions.
Results: He was started on total parenteral nutrition (TPN) to build up his nutritional status and planned for gastric-jejunal (GJ) bypass as his symptoms did not resolve after a week. However, one month later, his condition improved drastically, and he was able to tolerate diet. A repeat water-soluble contrast meal showed a complete resolution of GOO more than 1 month after clinical presentation.
Conclusion: In the event gastric outlet obstruction in a malnourished patient, conservative treatment with TPN and ‘drip and suck’ may be beneficial and can lead to spontaneous resolution without surgery required.
Keywords
Gastric outlet obstruction, Spontaneous, Resolved.
Introduction
Intestinal obstruction following surgery occurred commonly due to adhesions [1]. It can initially be treated conservatively with the “drip and suck” method that will result in resolution of symptoms. In cases where conservative management fail, surgery is the mainstay of treatment. The threshold for surgery is usually 5-7 days. We report a rare case of spontaneously resolved intestinal obstruction 1 month after presentation.
Case Reports
A 71-year-old gentleman with past medical history of chronic hepatitis B complicated with multifocal hepatocellular carcinoma underwent living donor liver transplant (LDLT) in our institution. He had a stormy post-operative period with bile leak from both ductal system as well as intra-abdominal collections. He was treated with percutaneous drainage of abdominal collections and endoscopic retrograde cholangiopancreatography (ERCP) with insertion of stent into the common bile duct bypassing both leaks.
During follow up computed tomography (CT) scan of liver 2 months’ post-transplant, he was found to have stenosis of the transplanted hepatic artery and was thus admitted under Transplant Surgery care for further evaluation and treatment. He was started on intravenous (IV) heparin which was subsequently converted to subcutaneous enoxaparin. During the same admission, he also developed gastric outlet obstruction (GOO) with symptoms of persistent vomiting and high nasogastric tube (NGT) aspirates. Two nasojejunal tube (NJT) insertion under fluoroscopic guidance was attempted but failed. He was found to have oedematous pylorus and a possible D1/D2 stricture.
He was then started on total parenteral nutrition (TPN) to improve his nutritional for pre-op optimization. His albumin level at that point of time was only 26 g/dl. His transaminases were also elevated, ranging between 350 -400IU/l. Other laboratory investigations were unremarkable. Water soluble contrast meal revealed a hold up in D1/D2 likely due to adhesions and stricture (Figure 1). Trials of oral feeds were attempted gradually. His condition was variable throughout the admission as he had alternating days of good tolerance of oral feeds with days of persistent vomiting. A repeat water-soluble contrast meal which was conducted 3 weeks later still showed persistent held up in the D1/D2 region.
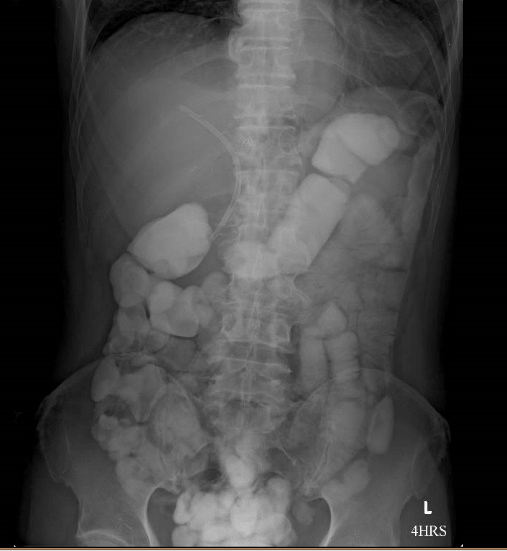
He was then planned for a gastro-jejunal (GJ) bypass as his condition will unlikely improve. Miraculously, over the course of a week, his condition improved drastically with no episode of vomiting. His oral intake was escalated to soft diet and he was able to tolerate well. Repeat water soluble contrast study showed complete gastric emptying of contrast at 4 hours with no evidence of gastric outlet obstruction (Figure 2). The previously noted narrowing of the duodenal calibre had also disappeared and the small bowel transit time is normal. His GOO had spontaneously resolved after more than 1 month of clinical presentation.
Figure 1: Persistent hold up of contrast in gastric and D1/D2
Figure 2: Complete gastric emptying with no evidence of gastric outlet obstruction
Discussion
Gastric outlet obstruction (GOO) is a clinical syndrome comprising of abdominal pain and postprandial vomiting due to mechanical obstruction. The incidence of intestinal obstruction after abdominal operations is reported to be about 3-5 % [2]. Intestinal obstruction after LDLT is even rarer, reported to be about 1.2 % [3]. Different causes of intestinal obstruction after LDLT have been reported. Intestinal obstruction due to incarcerated Petersen’s hernia following Roux-en-Y hepaticojejunostomy for biliary reconstruction, diaphragmatic hernia, enterolith causing obstruction and internal hernia of small bowel around trans-anastomotic biliary catheter had all been reported in the literature [2, 4-7]. In our case, the cause of intestinal obstruction is likely due to adhesions based on the onset of symptoms 2 months after surgery.
The mainstay of diagnosis for GOO is water soluble contrast studies. It is a well-known therapeutic and diagnostic tool. The appearance of water-soluble contrast in the colon on a plain abdominal X ray within 24 hours of its administration predicts resolution of intestinal obstruction [8]. Recommendations on duration of conservative management were variable. Some suggested a short observation of 24-48 hours while some authors suggest a longer duration, with the upper limit of 5 days [9]. However, if the symptoms prolonged beyond one week, it is unlikely to resolved. The peculiarity in our case was that his symptoms persisted for more than a month, and while surgery was planned with pre-op nutritional support, he achieved full resolution of symptoms.
Surgery is the mainstay of treatment for non-resolving gastric outlet obstruction secondary to adhesion. As in our case, his symptoms persisted for 1 month without any signs of resolution. Gastrojejunostomy (GJ) has been proven to show favourable outcome and relieves many symptoms [1]. In a report by Blachar et al, a total of 19 patients had bowel obstruction after liver transplantation and only two resolved without surgery [3]. However, to our surprise, his condition improved, and his symptoms resolved spontaneously while we were building up his nutrition for surgery. Our hypothesis is that the adhesion bands could have resolved due to the ongoing immunosuppressant. Another probability could be shrinkage of part of the liver from hepatic artery stenosis causing less obstruction on the duodenum.
Conclusion
To our knowledge, this is the first case of gastric outlet obstruction spontaneously resolved 1 month after presentation. The added rarity of this case is our patient had undergone living donor liver transplant and no similar case had been reported in the literature. We concluded that gastric outlet obstruction secondary to adhesion band in D1/D2 can resolve spontaneously following a period of conservative management.
Consent
Informed consent was obtained from participating individual included in the report
Conflict of Interest
The authors declare that they have no conflict of interest.
Article Info
Article Type
Case ReportPublication history
Received: Mon 04, Feb 2019Accepted: Thu 21, Feb 2019
Published: Mon 11, Mar 2019
Copyright
© 2023 Tan Hiang Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.01.013
Author Info
Corresponding Author
Tan Hiang JinDepartment of General Surgery, Singapore General Hospital, Singapore
Figures & Tables

References
- Duron JJ, Silva NJ, du Montcel ST, Berger A, Muscari F, et al. (2006) Adhesive postoperative small bowel obstruction: incidence and risk factors of recurrence after surgical treatment: a multicenter prospective study. Ann Surg 244: 750-757. [Crossref]
- Abdel Wahab M, Shehta A, Adly R, Elshoubary M, Salah T, et al. (2018) Internal hernia of the small intestine around biliary catheter after living-donor liver transplantation: A case report. Int J Surg Case Re 49: 158-162. [Crossref]
- Blachar A, Federle MP (2001) Bowel obstruction following liver transplantation: clinical and ct findings in 48 cases with emphasis on internal hernia. Radiology 218: 384-388. [Crossref]
- Liu CL, Lo CM, Chan SC, Fan ST, Wong J (2004) Internal hernia of the small bowel after right‐lobe live donor liver transplantation. Clin Transplant 18: 211-213. [Crossref]
- Sakamoto S, Goto R, Kawamura N, Yasuyuki K, Masaaki W, et al. (2017) Petersen’s hernia after living donor liver transplantation. Surg Case Rep 3: 89. [Crossref]
- Okajima H, Hayashida S, Iwasaki H, Suda H, Takeichi T, et al. (2007) Bowel obstruction due to diaphragmatic hernia in an elder child after pediatric liver transplantation. Pediatr Transplant 11: 324-326. [Crossref]
- Mukai S, Onoe T, Tashiro H, Ohdan H (2015) Small bowel obstruction due to an unconjugated ursodeoxycholic acid enterolith following living donor liver transplantation: report of a case. Hepatol Res 45: 818-822. [Crossref]
- Abbas S, Bissett IP, Parry BR (2007) Oral water soluble contrast for the management of adhesive small bowel obstruction. Cochrane Database Syst Rev 18: CD004651. [Crossref]
- Seror D, Feigin E, Szold A, Allweis TM, Carmon M, et al. (1993) How conservatively can postoperative small bowel obstruction be treated? Am J Surg 165: 121-125; discussion 125-126. [Crossref]
