A Rare Case of Osteoma Cutis in the Auricular Pinna: Clinical Presentation and Management Considerations
Introduction
Osteoma cutis is a rare and benign dermatological condition characterized by the presence of bone in the dermis or subcutaneous tissue [1]. This results in the development of firm, hard nodules or plaques on the skin's surface. The bony growths can vary in size, texture, and appearance. Osteoma cutis is typically benign and asymptomatic, but it can cause cosmetic concerns for affected individuals. Several factors have been associated with its development. Primary osteoma cutis occurs when there are no pre-existing lesions. Genetic factors have been associated with the primary type such as the GNAS1 gene mutation [2]. This gene plays a role in regulating bone growth and development; it is a key regulatory gene implicated in progressive osseous heteroplasia and albright hereditary osteodystrophy [2, 3]. Primary osteoma cutis can also manifest either independently or in conjunction with metabolic syndrome [4, 5].
Secondary osteoma cutis is linked to inflammatory processes, scars, dysembryoplasia, or neoplasms. Trauma, inflammation, tattoos, or certain skin conditions, such as acne or scleroderma, have been identified as potential triggers for the formation of bone tissue within the skin [6-8]. This is evident in the diverse locations where osteoma cutis can develop, such as the facial region in females and the scalp or chest area in males. While these factors are associated with osteoma cutis, the condition remains rare and occurs sporadically in most cases. In this paper, we present a rare case of an osteoma cutis of the auricular pinna following a self-inflicted piercing, highlighting the treatment approach employed to address this condition.
Case Presentation
A 27-year-old female patient presented herself for an otorhinolaryngology examination due to the appearance of a swelling on the right auricular pinna that had been present for the past six months since August 2022. During the medical history interview, the patient revealed that she had self-inserted a piercing in the affected area. The patient was a heavy smoker, consuming approximately 30 cigarettes per day, and also reported alcohol and unspecified drug use. The piercing was traumatic and resulted in the formation of an otohematoma within three days. The hematoma was subsequently drained and treated with antibiotic and anti-inflammatory therapy, along with a compressive dressing. However, the patient did not attend the follow-up appointments, and there is no further information available regarding the progression and healing.
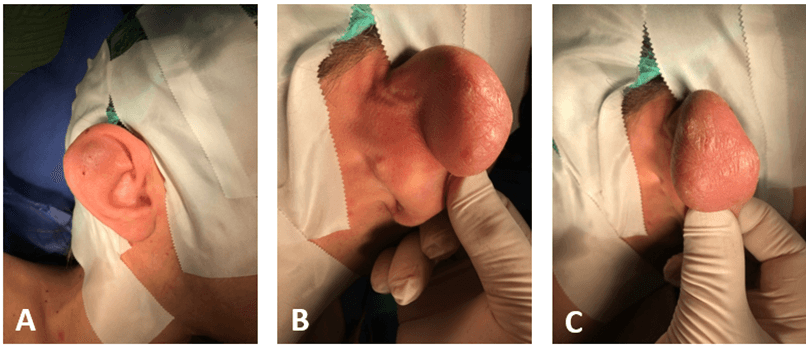
After six months, the patient returned for a check-up with the presence of a mass on the upper part of the auricular pinna. The mass measured approximately 5 × 3 × 2 cm, covered with slightly reddened skin. The patient states that the swelling had gradually increased in size and was characterized as non-painful, firm to touch, and exhibited limited mobility both superficially and deep within the tissues (Figure 1). No radiological imaging was conducted, as the otorhinolaryngologist suspected the presence of a cystic collection during the clinical examination. Therefore, the decision was made to proceed with draining the swelling. However, despite the administration of local anaesthesia using lidocaine with epinephrine, the needle insertion for drainage caused significant discomfort to the patient. Due to the intensity of the pain experienced, it was decided to proceed with a surgical intervention under general anaesthesia for the complete removal of the mass.
Figure 1: Pre-operative osteoma cutis of the auricular pinna. A) Lateral wall; B) Medial wall; C) Posterior wall.
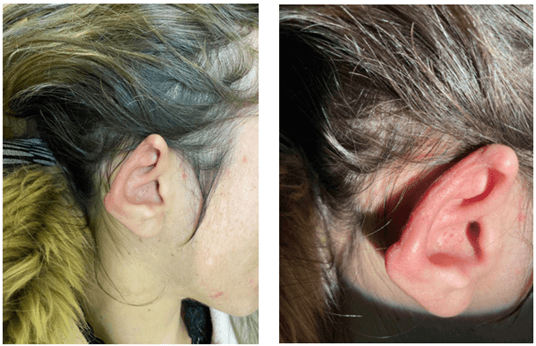
There were a voluminous neoformation, hard to the touch, adherent to the planes based in the helix region. After infiltration of the helix and concha region with a local anaesthetic, an incision was made along the posterior margin of the helix surrounding the voluminous neoformation. Identification and cleavage of the capsule from the lesion until healthy tissue is identified. Excision "en bloc" with the skin. A good hemostasis and suture for planes were made. Unfortunately, it was not possible to spare the overlying skin of the auricular pinna during the procedure, as the mass was inseparable from it. Upon incision, the lesion exhibited an elastic consistency with a hard central core (Figure 2). The patient's post-operative course was uneventful, and she experienced relief from the swelling. Follow-up consultations were scheduled to monitor the healing process and ensure the absence of any complications (Figure 3).
Figure 2: Osteoma cutis of the auricular pinna. A) Osteoma cutis before incision. B) Osteoma cutis after incision. C) Osteoma cutis with visible hard central core.
Figure 3: Post-operative auricular pinna lateral wall.
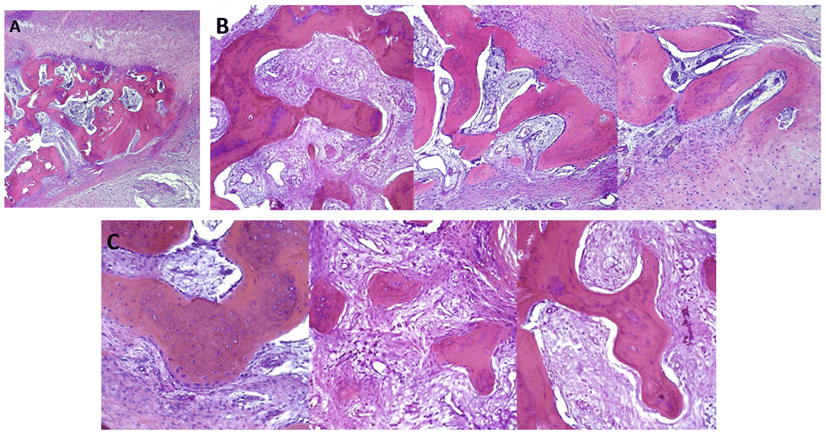
The histological examination described macroscopically a fibrocartilaginous tissue of the auricular lobe covered by a 4.5 × 2.7 × 2.5 cm cutaneous area affected by an increased consistency lesion with irregular and blurred calcified areas, ulcerated, measuring 2 × 1.5 cm. The pathology in the report described "the specimen, displays a concentric structure composed of lymphomonocytic inflammatory tissue at the periphery with abscess areas and, in the central zone, sclerotic tissue with osseous metaplasia. No signs of malignancy observed.
Conclusion
Chronic inflammatory process with abscess formation, reactive fibrotic features, and evidence of osseous metaplasia resembling (osteoma cutis) (Figure 4). After the first appointment, the patient decided not to attend the subsequent follow-up and declined to give consent for a genetic investigation to search for the GNAS1 gene.
Figure 4: Osteoma cutis, microscopic view. A) x4 magnification; B) x10 magnification; C) x20 magnification.
Discussion
In this case report, we explored the clinical manifestations, diagnostic approaches, and treatment strategies pertaining to osteoma cutis, a rare disorder marked by the formation of fully developed bone within the dermal layers. The case under examination focused on a patient who experienced the development of osteoma cutis in the auricular pinna subsequent to a traumatic self-induced piercing. The diagnosis was corroborated through histological analysis, revealing the existence of mature osseous tissue within the lesion.
The etiology of osteoma cutis continues to be an area of active investigation. Numerous theories have been postulated, encompassing genetic mutations and precipitating factors such as trauma. Our case lends support to the notion that trauma, exemplified here by the self-inflicted piercing, may serve as a catalyst for anomalous bone development within the dermis. This observation corroborates previous research highlighting analogous instances [6, 7]. Osteoma cutis is a rare condition characterized by the formation of mature bone within the skin. It can present either as a primary condition or secondary to other underlying factors such as genetic mutations, inflammatory processes, scars, dysembryoplasia, or neoplasms. The pathogenesis of osteoma cutis is still not fully understood, but various mechanisms have been proposed. Some studies have shown an association between osteoma cutis and GNAS1 gene mutations [2, 3]. GNAS1 is a key regulatory gene involved in progressive osseous heteroplasia and albright hereditary osteodystrophy. These mutations can lead to the abnormal activation of osteoblasts and subsequent ectopic bone formation in the skin.
Notably, cartilage formation is typically absent, as the predominant mechanism of bone formation in osteoma cutis involves membranous ossification. Within the lesion, osteoblasts, osteoclasts, and osteocytes may be observed, and in larger deposits, haversian systems can be identified. Histopathologically, osteoma cutis exhibits distinct features, including the presence of dense eosinophilic deposits within the subcutaneous tissue and dermis [9]. Clinically, osteoma cutis manifests as solitary or multiple, asymptomatic lesions ranging in size from 0.1 cm to 5 cm. These formations can appear as papules, plaques, nodules, or miliary lesions, exhibiting a firm consistency upon palpation [10]. Four clinical variants of osteoma cutis have been described in the literature: solitary, widespread, plate-like, multiple miliary osteomas [11].
Clinical investigation plays a crucial role in raising diagnostic suspicion, with potential indicators including the evaluation of calcium and parathyroid hormone levels, especially in primary forms like albright hereditary osteodystrophy. Radiographic and CT imaging studies are valuable tools for assessing the presence of osseous tissue, with cone-beam CT offering high diagnostic accuracy for osteoma cutis. Nevertheless, a conclusive diagnosis can only be achieved through histological examination [10]. The literature describes different treatment modalities for osteoma cutis, which vary based on the severity, extent, location, and underlying cause of the condition. Two approaches have been suggested: non-invasive and invasive. Non-invasive treatment involves the application of topical tretinoin cream, although it is primarily effective for small and superficial lesions. Invasive treatment options, such as dermabrasion, surgical excision, erbium laser, CO2 laser, or curettage, are employed for biggest lesions [12, 13].
Management of osteoma cutis typically involves surgical excision, especially in cases where the mass causes discomfort or aesthetic concerns. In our case, considering the involvement of the auricular pinna and the substantial size of the lesion, we opted for this approach. Long-term follow-up is crucial in cases of osteoma cutis to monitor for recurrence or any associated complications. Further research is warranted to better understand the underlying mechanisms of osteoma cutis and optimize management strategies. This includes elucidating the role of genetic factors, investigating potential biomarkers for early diagnosis, and exploring alternative treatment options. Collaborative efforts across disciplines and multi-center studies may provide valuable insights into the pathogenesis, diagnosis, and management of this rare condition. The lack of genetic analysis does not allow us to conclusively determine whether this is a primary or secondary case of osteoma cutis, although the clinical history suggests the latter hypothesis. We acknowledge that the management of this case may not have been flawless, but given the rarity of the condition, we did not have sufficient experience to confidently approach the diagnostic and therapeutic aspects.
In conclusion, the case presented highlights the role of trauma as a triggering factor and emphasizes the challenges in surgical management when the overlying skin is involved. Long-term follow-up and patient compliance are essential for monitoring outcomes and assessing potential complications. Continued research is necessary to enhance our understanding of the pathogenesis and improve the management of osteoma cutis. Nonetheless, our case could prove valuable in contributing to the current scientific literature on this rare condition. Few studies are available precisely due to its rarity, and no cases have been reported in the literature concerning its presentation in the auricular pinna.
Conflicts of Interest
None.
Funding
None.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Article Info
Article Type
Case ReportPublication history
Received: Mon 23, Oct 2023Accepted: Fri 17, Nov 2023
Published: Mon 04, Dec 2023
Copyright
© 2023 Cosimo Galletti. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2023.06.01
Author Info
Daniele Portelli Mariagrazia Ferrisi Francesco Ciodaro Guido Fadda Bruno Galletti Cosimo Galletti
Corresponding Author
Cosimo GallettiResident of Department of Adult and Development Age Human Pathology “Gaetano Barresi”, Unit of Otorhinolaryngology, University of Messina Via Consolare Valeria, Messina, Italy
Figures & Tables

References
1.
Limaiem F, Sergent SR
(2023) Osteoma Cutis.
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. [Crossref]
2.
Elli FM, Barbieri AM,
Bordogna P, Ferrari P, Bufo R et al. (2013) Screening for GNAS genetic and
epigenetic alterations in progressive osseous heteroplasia: first Italian
series. Bone 56: 276-280. [Crossref]
3. Ward S, Sugo E,
Verge CF, Wargon O (2011) Three cases of osteoma cutis occurring in infancy. A
brief overview of osteoma cutis and its association with
pseudo-pseudohypoparathyroidism. Australas J Dermatol 52: 127-131. [Crossref]
4. Thielen AM, Stucki
L, Braun RP, Masouyé I, Germanier L et al. (2006) Multiple cutaneous osteomas
of the face associated with chronic inflammatory acne. J Eur Acad Dermatol
Venereol 20: 321-326. [Crossref]
5. Amorim GM, Falcão
EMMFMM, Quintella DC, Cuzzi T, de Magalhães TC et al. (2017) Primary isolated
osteoma cutis of the face. Dermatol Online J 23: 13030/qt4zz8d3tm. [Crossref]
6. Pignolo RJ,
Ramaswamy G, Fong JT, Shore EM, Kaplan FS (2015) Progressive osseous
heteroplasia: diagnosis, treatment, and prognosis. Appl Clin Genet 8:
37-48. [Crossref]
7. Basu P, Erickson
CP, Calame A, Cohen PR (2019) Osteoma Cutis: An Adverse Event Following Tattoo
Placement. Cureus 11: e4323. [Crossref]
8. Vashi N, Chu J,
Patel R (2011) Acquired plate-like osteoma cutis. Dermatol Online J 17:
1. [Crossref]
9. Delaleu J,
Cordoliani F, Bagot M, Bouaziz JD, Vignon Pennamen MD et al. (2020) Miliary
osteoma cutis of the face. Ann Dermatol Venereol 147: 313-315. [Crossref]
10. Alhazmi D, Badr F,
Jadu F, Jan AM, Abdulsalam Z (2017) Osteoma Cutis of the Face in CBCT Images. Case
Rep Dent 2017: 8468965. [Crossref]
11. Orlando G, Salmaso
R, Piaserico S (2019) A Case of Secondary Osteoma Cutis Associated with Lichen
Planopilaris. Acta Derm Venereol 99: 1190-1191. [Crossref]
12. Cohen AD, Chetov T, Cagnano E, Naimer S, Vardy DA (2001) Treatment of multiple miliary osteoma cutis of the face with local application of tretinoin (all-trans-retinoic acid): a case report and review of the literature. J Dermatolog Treat 12: 171-173. [Crossref]
13. Fulton Jr JE (1987) Dermabrasion-Loo-punch-excision technique for the treatment of acne-induced osteoma cutis. J Dermatol Surg Oncol 13: 655-659. [Crossref]
