A Rare Case of an Intraluminal Abscess of the Umbilical Artery as Differential Diagnosis for Omphalitis in Newborns
A B S T R A C T
Omphalitis is an infection of the umbilicus and/or the surrounding tissue. It occurs predominantly in the newborn period. Sometimes a persistent urachus can cause an abscess in the umbilical region. Intraluminal abscesses of the umbilical vessels are not commonly described as a differential diagnosis for omphalitis in newborns. Here we present a rare care case of an intraluminal abscess of the umbilical artery of a newborn. After operative exploration and incision of the abscess, further antibiotic treatment was needed until blood cultures showed no further bacterial growth.
Keywords
Omphalitis, abscess, patent urachus, umbilical infection
Introduction
Omphalitis is an infection of the umbilicus and/or the surrounding tissue and occurs predominantly in the newborn period [1]. The incidence is higher in home births and reaches up to 21.7 % in developing countries [2, 3]. The devitalized tissue of the umbilicus can easily be colonized by several bacteria. There is sufficient evidence that the application of antiseptic to the cord reduces bacterial colonization while specific antiseptics vary in effectiveness depending on their antibacterial properties, the mode or frequency of application, the concentration of the antiseptic used and the degree of contamination in the environment [4]. Risk factors for omphalitis and a poor prognosis are unplanned home birth or septic delivery, low birth weight, prolonged rupture of membranes, umbilical catheterization, and chorioamnionitis [5]. Severe complications are necrotizing fasciitis, peritonitis with intra-abdominal abscesses or hepatic abscesses and the development of an adhesive intestinal obstruction [6]. Whereas mortality is low in high-income countries, high mortality rates of up to 59% have been reported in patients with omphalitis complicated by necrotizing fasciitis [7, 8].
Typical differential diagnoses are patent urachus, umbilical granulomas with serosanguinous drainage and easy bleeding after trauma and funisitis [1]. Abscesses of the umbilical artery are not commonly known as a differential diagnosis for omphalitis. Probably due to improved umbilical care with close inspections of the umbilical region by healthcare professionals, intraluminal abscesses of the umbilical arteries are today a rare observed disease. We could not find publications addressing this pathology in recent years in literature. Here we present a rare case of a newborn with an abscess of the umbilical artery and the further postoperative treatment.
Case Report
A 19-days old newborn was presented by his parents in our emergency department on the advice of their children’s doctor. The parents reported they had recognized a swelling of the umbilicus and umbilical blennorrhea with leakage of turbid liquid since this day. The umbilicus fell off about one week ago. Since then, the parents have recognized recurring wetting of the umbilical region. Besides this, no other problems were mentioned. The patient was drinking well and the diaper had been wet all the time. The patient was a term infant, the pregnancy had been uneventful and all examinations at a pediatrician had been normal.
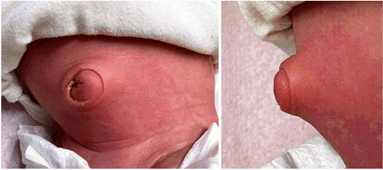
Clinical examination revealed a swollen, bulged umbilicus with induration and perifocal erythema without any current secretion (Figure 1). This region was sensitive to pressure. Besides this, the general condition was only slightly reduced, the capillary refilling time was lower by 1 second, the fontanelle was normal. The newborn had a normal constitution (weight 3.8 kg (94th percentile), length 53 cm (88th percentile), head circumference 37 cm (96th percentile)) and the temperature was normal (37.8°C).
Figure 1: Umbilical region (left: frontal view, right: side view) of the newborn with protrusion of the umbilicus and remnants of turbid discharge out of the umbilicus.
Sonography was performed and revealed an abscess in the umbilical region with a diameter of around 2 cm behind the abdominal wall. Blood tests showed normal Leukocytes (5.0 [5-19.5/nl]) but CRP was elevated up to 46 mg/l [1.0-5.0mg/l]. Besides this, we found no pathologies. Due to the clinical, chemical and sonographic aspects, we suspected an infected patent urachus and performed an operative exploration on the same day. Perioperatively, the patient was given antibiotic prophylaxis with ampicillin and gentamicin. While the patent urachus showed no signs of inflammation, we identified the left umbilical artery as the inflammatory focus: The artery was thickened and showed purulent discharge. The vessel was ligated near its origin out of the iliac artery, where it appeared normal, and the inflammatory narrowed part was excised. The inconspicious urachus was excised.
Postoperatively, we began an intravenous antibiotic treatment with piperacillin and tazobactam intravenous for two days which was changed to oral Amoxicillin and Clavulanic acid for another two days as we received the first microbiological results from the intraoperative swab, where Staphylococcus aureus had grown. On the day after surgery, the temperature increased to a maximum of 38.4°C but then continuously dropped until normal. The newborn was stable at all times and drank well. The postoperative course was completely uneventful. Due to positive blood culture (again Staphylococcus aureus), we decided to treat with intravenous Flucloxacillin according to sensitivity testing for another 5 days until blood cultures showed no further bacterial growth. No further problems were seen in a follow-up examination 7 months later in our hospital.
Discussion
Omphalitis is an infection of the umbilicus and/or the surrounding tissue. It occurs predominantly in the newborn period. Sometimes, when the physiological involution of normal embryologic tissues, which connects the developing bladder to the umbilical cord, fails, a patent infected urachus can cause an abscess in the umbilical region. Intraluminal abscesses are not commonly described as a differential diagnosis for omphalitis in newborns. In our case, an intraluminal abscess of the umbilical artery was found intraoperatively, and antibiotic treatment was performed until blood culture showed no more bacterial growth.
The abscess formation of the extracorporeal part of the umbilical has been published in other species. Collatos et al. described an abscess in the external umbilical remnant and umbilical vein remnant in a yearling colt [9]. Due to the physiological drying of the cord with resulting poor blood supply, it is likely that especially the extracorporeal umbilical cord to become vulnerable to infections and abscesses. In our case, the abscess was localized in the intracorporeal part of the umbilical artery. Manipulation with resulting contamination of the vessels is known to be a risk factor for infections, while this rarely leads to intraluminal abscess formation. Despite this, Kotnis et al. reported a case where a remnant of an arterial catheter in the umbilical artery caused recurrent umbilical infections [10]. In our case, there was no insertion of a catheter reported, so these cases are hardly comparable.
In 1957 Isabella Forshall published a manuscript about septic umbilical arteritis and summed up earlier cases of umbilical sepsis all around the world [11]. Since umbilical care has been improved during the last decades, the occurrence of septic umbilical arteritis nowadays has dropped significantly. She presented a case series of four newborns aged between 2 days to 4 weeks, one infant aged 7 weeks and another child aged 4.5 years with septic umbilical arteritis.
Half of the patients died. In most cases, death occurred early after the onset of symptoms, whereas mortality was higher in the newborn population. Nearly all of the children showed purulent discharge out of the umbilicus. Additionally, the newborn refused to feed and often had poor general conditions. The oldest patient (4.5 years) showed purulent discharge out of the umbilicus for 3 months and probably, the abscess of the umbilicus had remained quiescent until the child was 4 years old. In consequence, this patient is hardly comparable to the younger patients, where the symptoms were more acute and manifested far earlier. Staphylococcus pyogenes had grown in 5 cases and other bacteria which could be isolated were “diphteroids” and “paracolon bacillus”. In three cases, the left umbilical artery showed an abscess. In the other cases, the abscess was located either in the right or in both arteries.
Faridi et al. reported that in most cases of simple omphalitis, Gram-negative organisms were responsible for omphalitis whereby, Klebsiella was the commonest Gram-negative organism [12]. In a later publication, Sawardekar reported Staphylococcus aureus, Escherichia coli and Klebsiella spp. showed to be the most common bacteria in their collective [2]. Additionally, this has been supported by an earlier study [5]. Interestingly, Forshall described in most cases that a Gram-positive organism was grown as it is in our case [11]. Despite this, in our case Staphylococcus aureus has been isolated in the swab and the blood culture. Staphylococcus aureus is commonly known to cause abscesses of the skin and soft tissue [13]. In conclusion, the empiric choice of antibiotics after incision of an abscess of the umbilical artery should include Staphylococcus aureus.
As mentioned previously, omphalitis is, depending on the health care, a common problem in the newborn period. A patent urachus is more likely to cause symptoms like discharge out of the umbilicus than an intraluminal abscess in the umbilical vessels. To exclude the possibility of the formation of an abscess, every newborn with omphalitis should be examined with sonography. If an abscess is present, surgical treatment should be indicated in a timely manner since these umbilical intraluminal abscesses are reported to cause high mortality in newborns and young infants.
Article Info
Article Type
Case ReportPublication history
Received: Thu 13, Jan 2022Accepted: Fri 28, Jan 2022
Published: Thu 24, Feb 2022
Copyright
© 2023 Markus Denzinger. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2022.01.07
Author Info
Markus Denzinger Katharina B M Schenk Patricia Reis Wolfertstetter Clemens Memmel Domitille Stark Christian Knorr
Corresponding Author
Markus DenzingerDepartment of Pediatric Surgery, Klinik St. Hedwig, Steinmetzstraße, Regensburg, Germany
Figures & Tables
References
1. Painter K, Anand S,
Philip K (2021) Omphalitis. In: StatPearls, Treasure Island (FL): StatPearls
Publishing. [Crossref]
2. Sawardekar KP
(2004) Changing spectrum of neonatal omphalitis. Pediatr Infect Dis J
23: 22-26. [Crossref]
3. Mir F, Tikmani SS,
Shakoor S, Warraich HJ, Sultana S et al. (2011) Incidence and etiology of
omphalitis in Pakistan: a community-based cohort study. J Infect Dev Ctries
5: 828-833. [Crossref]
4. Mullany LC,
Darmstadt GL, Tielsch JM (2003) Role of antimicrobial applications to the
umbilical cord in neonates to prevent bacterial colonization and infection: a
review of the evidence. Pediatr Infect Dis J 22: 996-1002. [Crossref]
5. Güvenç H, Aygün AD,
Yaşar F, Soylu F, Güvenç M et al. (1997) Omphalitis in term and preterm
appropriate for gestational age and small for gestational age infants. J
Trop Pediatr 43: 368-372. [Crossref]
6. Ameh EA, Nmadu PT
(2002) Major complications of omphalitis in neonates and infants. Pediatr
Surg Int 18: 413-416. [Crossref]
7. Zupan J, Garner P,
Omari AAA (2004) Topical umbilical cord care at birth. Cochrane Database
Syst Rev 2004: CD001057. [Crossref]
8. Hsieh WS, Yang PH,
Chao HC, Lai JY et al. (1999) Neonatal necrotizing fasciitis: a report of three
cases and review of the literature. Pediatrics 103: e53. [Crossref]
9. Collatos C, Reef
VB, Richardson DW (1989) Umbilical cord remnant abscess in a yearling colt. J
Am Vet Med Assoc 195: 1252-1254. [Crossref]
10. Kotnis R, Salloum
A, Hitchcock R (2000) Retained umbilical artery catheter presenting as an
umbilical abscess. Arch Dis Child Fetal Neonatal Ed 83: F77. [Crossref]
11. Forshall I (1957)
Septic umbilical arteritis. Arch Dis Child 32: 25-30. [Crossref]
12. Faridi MM, Rattan A, Ahmad SH (1993) Omphalitis neonatorum. J Indian Med Assoc 91: 283-285. [Crossref]
13. Kobayashi SD, Malachowa N, DeLeo FR (2015) Pathogenesis of Staphylococcus aureus abscesses. Am J Pathol 185: 1518-1527. [Crossref]
