Journals
A papillary thyroid cancer with adrenal and cerebral metastases complicated by left hemiplegia after radioactive Iodine therapy
A B S T R A C T
Background
Distant metastases of thyroid cancer are rare and are usually pulmonary or skeletal. We report here the case of a patient who presented with a multi-metastatic thyroid cancer with unusual localizations, that was complicated by convulsions and left hemiplegia during a post-operative RAI (RadioActive Iodine) therapy.
Case presentation
A 71-year old male patient, with a past history of left hemithyroidectomy 30 years ago and no available histopathologic report. He presented with a left lower limb deficit that had begun about a year ago. A cerebral MRI found a fronto-parietal lesion. The neck ultrasound showed a 55mm nodule of the remaining right thyroid lobe. The CT scan showed multiple bilateral pulmonary nodules suspected of metastases, as well as a 77mm right adrenal mass. Biopsies of the left basal pulmonary nodule and adrenal gland weren’t conclusive. The blood tests showed normal adrenal function, and a serum Thyroglobulin (TG) concentration at 417 ng/mL. The principal diagnostic hypothesis was an adrenocortical tumor with cerebral, pulmonary and thyroid metastases. The patient underwent a right adrenalectomy through laparotomy and completion thyroidectomy at the same time. The histopathology demonstrated a follicular variant of papillary thyroid carcinoma with adrenal metastasis (pT3N0M1R0). The patient received 100mCi RAI therapy after LT4 withdrawal 2 months post operatively and 10 days after the last session of cerebral radiotherapy. The principal diagnostic hypothesis was an acute hypothyroidism caused by RAI therapy. The neurological deficit lasted 6 weeks followed by a full recovery. At 4 and a half years, the patient was still asymptomatic. The CT scan showed stability of all pulmonary and cerebral lesions. The TG was 3.9 ng/mL with persistently negative anti-thyroid antibodies, the TSH was 0.03 µU/mL (under 175 µg/day of Levothyroxin).
Conclusion
We reported a rare case of recurrent papillary thyroid cancer with adrenal, cerebral and pulmonary metastases. The patient underwent a completion thyroidectomy and an adrenalectomy. After receiving his RAI dose, he developed a left hemiplegia. The principal diagnostic hypothesis was an acute hypothyroidism caused by RAI. After all, the RAI therapy was beneficial despite this complication and the patient had since then improved to his pre-diagnostic state.
K E Y W O R D S
Thyroid cancer, adrenal metastasis, cerebral metastasis, RAI therapy, hemiplegia
Background
Distant metastases of thyroid cancer are rare and are usually pulmonary or skeletal. Their presence at the initial diagnosis is a poor prognostic factor regardless of the histologic type, and they entail a significant reduction in survival. We report here the case of a patient who presented with a multi-metastatic thyroid cancer with unusual localizations (cerebral, adrenal, and pulmonary), that was complicated by convulsions and left hemiplegia during a post-operative RAI (RadioActive Iodine) therapy.
Case Presentation
A 71-year old male patient, with a past medical history of type 2 diabetes diagnosed a year earlier, dyslipidemia, and left hemithyroidectomy 30 years ago with no available histopathologic report. He presented with a left lower limb deficit that had begun about a year ago. There was no history of weight loss nor headaches.
The physical examination showed a very active patient with no altered mental status and no malnutrition. A cerebral MRI found a solitary irregular fronto-parietal lesion without contrast uptake, with an important surrounding edema. There was also a 5-cm thyroid nodule.
The neck ultrasound showed a solid macronodule of the remaining right thyroid lobe, measuring 55 x 32 x 41 mm with the following characteristics: hypoechoic, heterogenous, with central and peripheral vascularization. There were no visible cervical lymph nodes. The FNA (Fine Needle Aspiration) of the thyroid nodule was non-conclusive.
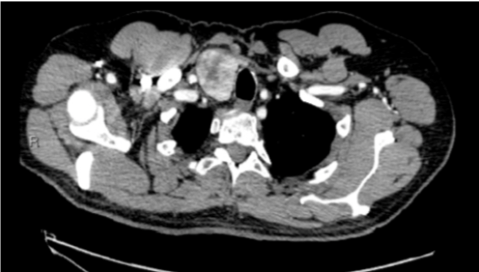
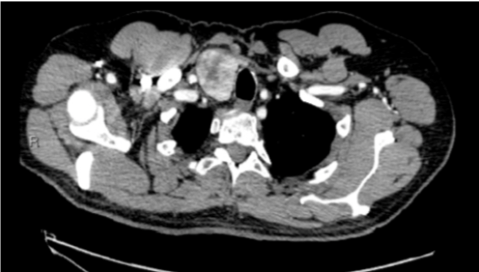
The full body CT scan showed a sizable thyroid nodule in the right lobe measuring 45 mm, without any pathologic cervical nor mediastinal lymph nodes. There were multiple bilateral pulmonary nodules suspected of metastases, as well as a right adrenal mass measuring 77 x 44 mm with a strong arterial vascularization and central necrosis, suspected initially as an adrenocortical tumor or a pheochromocytoma. Additionally, there were heterogenous para-aortic lymph nodes of 10 mm. There were no skeletal lesions.
The 18-FDG PET scan showed a hypermetabolic activity of the thyroid nodule and of a left basal pulmonary nodule, with a lesser intensity of the adrenal mass (less than that of the liver). An ENT (Ear-Nose-Throat) examination complete with a nasolaryngoscopy did not find any abnormalities. The vocal cords mobility was normal.
A biopsy of the left basal pulmonary nodule wasn’t conclusive.
A biopsy of the thyroid nodule found some cellular hyperplasia without signs of malignancy. The cells expressed the Thyroglobulin (TG) and the nuclear marker TTF-1 without expression of Calcitonin. There was no BRAF mutation.
The blood tests showed normal adrenal function, and a serum TG concentration at 417 ng/mL. At this point, the principal diagnostic hypothesis was an adrenocortical tumor with cerebral, pulmonary and thyroid metastases.
The patient underwent a right adrenalectomy by laparotomy and completion thyroidectomy at the same time. The para-aortic lymph nodes were not removed.
The postoperative course was simple, and the patient was discharged on the 6th postoperative day with a prescription of 150 µg/day of Levothyroxine.
Figures

The histopathology demonstrated a follicular variant of papillary thyroid carcinoma with adrenal metastasis. The thyroid capsule was not invaded but there were multiple vascular invasions. There were no peri-thyroidal nor peri-adrenal pathologic lymph nodes. The resection was complete with negative margins for both the thyroid and the adrenal gland, and the tumor was classified pT3N0M1 R0.
As for the cerebral metastasis, the patient received 3 doses of external radiotherapy 1 month post-operatively. Discussing the case in the TUTHYREF tumor board, a decision was made to administer a 100 mCi radioiodine therapy after LT4 withdrawal, so the Levothyroxin was stopped 5 weeks before the RAI session and was replaced by Cynomel 12,5 µg /day.
The patient received 100 mCi RAI therapy 2 months post-operatively and 10 days after the last session of cerebral radiotherapy, under the cover of corticosteriods.
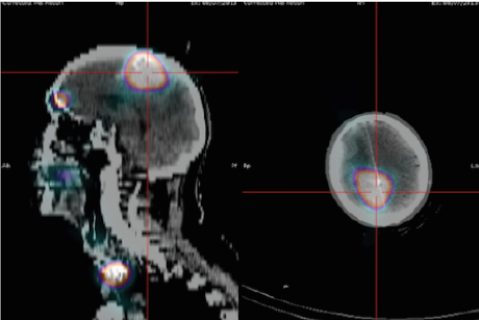
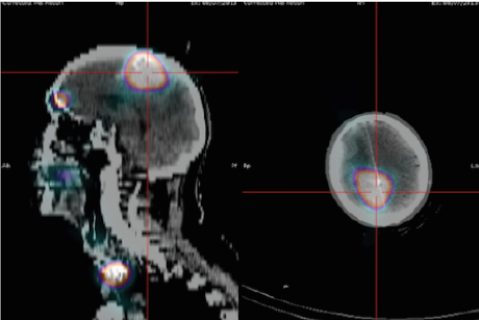
The blood work pre-RAI showed a serum TSH at 52 µU/mL, a TG at 322 ng/mL, and normal levels of anti-thyroid antibodies. The I131 scintigraphy found multiple localizations of hypermetabolic activities in the brain, neck, lungs, scapula, pancreatic tail, left adrenal gland, right para-iliac, and lower limbs.
Two days after administering the RAI dose, the patient developed a hemiplegia and a hemi-anosognosia, causing an accidental fall. An urgent cerebral CT scan showed comparable lesions to the pretreatment images. An EEG eliminated status epilepticus. The principal diagnostic hypothesis was an acute hypothyroidism caused by the RAI therapy. The patient was hospitalized in the endocrinology department then in a specialized reeducation unit. The neurological deficit lasted 6 weeks followed by a full recovery.
Two months after the RAI treatment, the serum TSH was 0.05 µU/mL under a suppressing treatment and the serum TG was 3.7 ng/mL. A CT scan of the chest, abdomen and pelvis 2 months after the I131-scintigraphy showed a partial response; the cervical lesions had disappeared, the para-renal nodule and the para-aortic lymph nodes had a 50% decrease in size, the pulmonary lesions had regressed partially and there were no new metastatic localizations. However, there was an incidental finding of a distal pulmonary embolism. A doppler-ultrasound of the lower limbs found sural and left common femoral DVTs (Deep Venous Thromboses). A low-molecular-weight heparin treatment was started by Innohep 0.7 mL/day for 6 months.
During a national tumor board discussion, it was decided to abstain from a second RAI dose considering the partial regression of metastatic lesions, and to follow up by a CT scan in 3 months.
At 5 months after the RAI therapy, the patient’s general condition had significantly improved to his pre-diagnosis level 2 years ago; the physiotherapy was stopped and the neuropsychologic evaluation was satisfying. A full-body CT scan found partial regression of pulmonary and cerebral lesions, with no other metastatic localizations. The TG was stable at 2.1 ng/mL, the T4 at 15.6 µU/mL and the TSH at 0.07 µU/mL. The thyroid-hormone replacement therapy was maintained by 175 µg/day of Levothyroxin.
A follow-up EEG was done after 1 year of the neurologic disorders, which was normal. At 1 and a half year of the surgery, the patient was asymptomatic. The chest-abdomen-pelvis CT scan showed stability of the 3 pulmonary nodules, a partial regression of the right frontal lesion, and a stability in the contrast uptake in the left temporo-occipital area of 2 mm.
At 3 and a half years, the patient was still asymptomatic. The CT scan showed stability of all pulmonary and cerebral lesions. At 4 years, the TG was 3.9 ng/mL with persistently negative anti-thyroid antibodies, the TSH was 0.03 µU/mL (under 175 µg/day of Levothyroxin). The HbA1C was 5.9%.
Discussion
Our initial diagnostic hypothesis was a multi-metastatic adrenocortical tumor, given that the biopsies from the thyroid and the lung were non-conclusive. Finally, the diagnosis was a recurrent follicular variant of papillary thyroid cancer with cerebral, pulmonary and adrenal metastases.
A few cases of adrenal metastasis of thyroid cancer are described in the literature. Blanchet et al reported 2 cases in a literature review the first was in a patient operated for a well-differentiated follicular carcinoma, then developed right adrenal metastasis 12 years after the surgery and the RAI therapy [1, 2]. The TG was measured regularly post-operatively, and it showed an elevation to 149 ng/mL then the diagnosis was made by an abdominal CT. The histopathologic analysis of the adrenal gland confirmed the diagnosis. The TG decreased to 0.9 ng/ml 5 months post-operatively. This case demonstrates the importance of long-term follow-up by TG in these cancers. The second case was a 66-year old patient diagnosed with an invasive Hürthle-cell carcinoma with synchronous metastasis at diagnosis [3]. Blanchet et al had then established a protocol for similar cases they begin with looking for incidentalomas, then in case of significant uptake on the full-body I131 scintigraphy and elevated TG, an adrenalectomy is indicated. Indeed, this technique of tumoral mass reduction should allow for a better result of the post-operative I131 and the suppressive hormonal therapy on the microscopic remnants of the tumor [1].
Zao et al described the case of a 57-year old patient operated for a follicular thyroid cancer followed by RAI therapy because of elevated TG level (890 µg/L) [4]. The SPECT/CT showed a positive signal in the cervical region, in both lungs, and an adrenal gland. Seven months later, the patient presented with neurological problems and the SPECT/CT showed cerebral metastases. Therefor he received a 2nd dose of RAI and a cerebral radiotherapy. The similarity here with our case is astounding, but this patient passed away afterwards. The authors’ conclusion was that the CT in addition to the I131 scintigraphy are the ideal imaging modalities to localize and confirm the unusual and rare metastatic lesions of differentiated thyroid cancer.
Fedala et al., reported the principal unusual localizations of metastatic differentiated thyroid cancers in a retrospective study of 485 patients collected over 26 years [5]. They are rare (1.85%), more common in women (67%) and in the follicular variant of papillary carcinoma (66%). The mean age of metastasis diagnosis is 53 years, 3 years after the initial diagnosis of thyroid cancer. In total, 55% of patients were at stage IV. The diagnosis of metastasis was made in 89% of cases through a metastatic work-up. In the remaining cases, the metastasis was the initial finding which led to the discovery of the thyroid cancer. The localizations were hepatic (55%), adrenal (44%), cerebral, cerebellar, renal and cutaneous (11%). They were symptomatic in 55% of patients and diagnosed in a context of multiple metastases (bone, lungs) in 67% of cases. The follow-up showed a 22% mortality rate, higher in case of adrenal metastasis (55%), and a morbidity of 78%. The median survival time was 3 years. In short, metastatic differentiated thyroid cancer are becoming more frequent, mostly asymptomatic, indicate a poor prognosis, and must be looked for in multi-metastatic contexts.
An article reported a multi-metastatic (bone, lungs) papillary thyroid cancer in a 47-year old patient with bilateral adrenal metastases, diagnosed during RAI therapy with I131 scintigraphy [6]. Bilateral adrenal tumors are classically suggestive of metastases [1].
An article reported the case of a 57-year old patient operated for adrenal metastasis of a follicular thyroid cancer with a heart thrombus. The follow-up showed diffuse metastases resulting in the patient’s death 9 months post-operatively. Follicular carcinomas represent about 20% of thyroid cancers, more frequently in women older than 50 years and in areas with iodine deficiency. Visceral metastases ate frequent while the adrenal localizations are exceptional [7].
Brient and al studied differentiated thyroid cancer with liver metastases in a series of 14 patients. The development of liver metastases from differentiated thyroid cancer is a very poor prognostic sign. Tyrosin Kinase Inhibitor chemotherapy, in particular, is promising in curing this type of metastasis in some patients [8].
The literature reports a case of thyroid metastasis of an adrenocortical tumor 41 years after the initial diagnosis of the original tumor [9]. Thyroid metastases are rare, representing less than 4% of all thyroid neoplasms, and can occur many years after the initial tumor diagnosis. Nixon et al. studied the origin and the treatment of thyroid metastases [10]. In their series, the clear-cell renal carcinoma was the most frequent, while in the post-mortem studies the pulmonary tumors were the culprit. Thyroidectomy could allow for a long-term local control when the thyroid metastasis is uniquely present, but it’s rarely indicated in case of multi-metastases. To resume, these are complex clinical situations that should be discussed in tumor boards and managed depending on the primitive cancer, the number of metastases and the existent comorbidities of the patient.
Mirallié et al. studied the management and prognosis of metastases to the thyroid gland. Intra-thyroidal metastases are rare, but the diagnosis should be kept in mind when patients have a history of cancer (mainly renal cancer). Numerous patients had had diffuse metastases [11].
At 4 years post operatively, our patient – who is multi-metastatic – is doing very well; he has no neurological symptoms, the TG is stable, the pulmonary and cerebral lesions have regressed partially, and all other metastatic foci have disappeared. Wang et al reported that the 5-year survival rate in patients with multi-metastatic thyroid cancer was less than that of patients with a single metastasis (15.3% vs 77.6% respectively, p < 0.001) [12].
RAI therapy was beneficial despite the acute neurological complication. In 6 weeks, the patient had regained his normal physical condition as the one before the diagnosis. A few cases of post-RAI convulsions were described in the literature but without a persistent neurologic deficit. To prevent this, the duration of the gap between the RAI therapy and the external cerebral radiotherapy as well as the treatment by IV corticosteroids (Solumedrol or even Mannitol) to reduce brain edema should be discussed.
Conclusion
We reported a rare case of recurrent papillary thyroid cancer with adrenal, cerebral and pulmonary metastases. The patient underwent a completion thyroidectomy and an adrenalectomy at the same time. After receiving his RAI dose, he developed a left hemiplegia. The main neurologic causes were eliminated (grand mal seizure and progression of cerebral lesions). The principal diagnostic hypothesis was an acute hypothyroidism caused by RAI therapy. Finally, the RAI therapy was beneficial despite this complication and the patient had since then improved to his pre-diagnostic state.
Declarations
List of abbreviations
RAI (RadioActive Iodine) therapy, MRI (magnetic resonance imaging), EEG (electroencephalogram), DVTs (Deep Venous Thromboses), (TG) Thyroglobulin, ENT (Ear-Nose-Throat)
Consent to publication
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.
Availability of data and materials
The availability of data and data sharing does not apply to this article, because no data set was generated or analyzed during this study.
Competing interests
The authors state that they have no competing interests.
Funding
The authors have no funding to declare.
Author’s contributions
EM and CC performed surgery and perioperative management of the patient. EM, ALF and SB wrote the manuscript. EM, CC and DD performed perioperative management of the patient. All authors have read and approved the final manuscript.
Article Info
Article Type
Case ReportPublication history
Received 4 July, 2018Accepted 18 July, 2018
Published 31 July, 2018
Copyright
© 2018 Le Fouler A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.02.006
Author Info
Corresponding author
Le Fouler AClinique de Chirurgie Digestive et Endocrinienne (CCDE), Institut des Maladies de l’Appareil Digestif (IMAD), Hôtel Dieu, CHU Nantes, Place Alexis Ricordeau 44093 Nantes CEDEX 1
Figures & Tables

References
1. Blanchet MC, Van Box Som P, Peix JL (1997) Adrenal gland metastases of thyroid cancers. 2 cases. Presse Medicale Paris Fr 1983 26: 1239-1240.
2. Girelli ME, Casara D, Rubello D, Piccolo M, Piotto A, et al. (1993) Metastatic thyroid carcinoma of the adrenal gland. J Endocrinol Invest 16: 139-141. [Crossref]
3. Orsolon P, Bagni B, Geatti O, Guerra UP (1996) An unusual adrenal metastasis secondary to Hürthle cell carcinoma of the thyroid. Clin Nucl Med 21: 312-315. [Crossref]
4. Zhao Z, Shen G, Liu B, Kuang A (2016) Unusual Adrenal and Brain Metastases from Follicular Thyroid Carcinoma Revealed by 131I SPECT/CT. Clin Nucl Med 41: e53-55. [Crossref]
5. Fedala NS, Kabour S, Yaker F, Ali LA, Haddam AEM, et al. (2014) Métastases inhabituelles des carcinomes thyroïdiens différenciés. Httpwwwem-Premiumcomdatarevues00034266v75i5-6S0003426614003990 [Internet]. Nov 10 [cited 2017 Feb 14].
6. Batawil N (2013) Papillary thyroid cancer with bilateral adrenal metastases. Thyroid Off J Am Thyroid Assoc 23: 1651-1654. [Crossref]
7. Paparel P, Tatou E, Krause D, Cognet F, Cercueil J-P, et al. (2004) Adrenal metastasis from follicular thyroid carcinoma with intra-cardiac thrombus. Progres Urol 14: 203-204. [Crossref]
8. Brient C, Mucci S, Taïeb D, Mathonnet M, Menegaux F, et al. (2015) Differentiated thyroid cancer with liver metastases: lessons learned from managing a series of 14 patients. Int Surg 100:490-496. [Crossref]
9. Valo I, Verrièle V, Giraud P, Lorimier G, Guyétant S, et al. (2004) Métastases thyroïdiennes d’un corticosurrénalome 41 ans après le diagnostic de la tumeur initiale. Ann Pathol 24: 264-267.
10. Nixon IJ, Coca-Pelaz A, Kaleva AI, Triantafyllou A, Angelos P, et al. (2016) Metastasis to the Thyroid Gland: A Critical Review. Ann Surg Oncol. [Crossref]
11. Mirallié E, Rigaud J, Mathonnet M, Gibelin H, Regenet N, et al. (2005) Management and prognosis of metastases to the thyroid gland. J Am Coll Surg 200: 203-207. [Crossref]
12. Wang LY, Palmer FL, Nixon IJ, Thomas D, Patel SG, et al. (2014) Multi-organ distant metastases confer worse disease-specific survival in differentiated thyroid cancer. Thyroid Off J Am Thyroid Assoc 24: 1594-1599. [Crossref]
