A Lethal Case of a 3B Stage Emphysematous Pyelonephritis
A B S T R A C T
Emphysematous pyelonephritis (EPN) is a rare, necrotising infection of the renal parenchyma, leading to the accumulation of gas within the kidney and in the perinephric space. Patients with diabetes account for 85-100% of cases. The current treatment is one of the potent antimicrobial therapies together with kidney drainage and fluid resuscitation. Nephrectomy should be considered if patients deteriorate or do not improve on conservative treatment. We report a case of 62-year-old woman with multiple comorbidities, with a diagnosis of EPN whose condition did not improve despite the standard treatment approach.
Keywords
Emphysematous, pyelonephritis, nephrectomy, diabetes
Introduction
Emphysematous pyelonephritis (EPN) is a type of necrotizing infection that results in the production of gas in the renal parenchyma, renal collecting duct, or perinephric tissue [1]. Proliferating bacteria produce carbon dioxide and hydrogen during the fermentation process, which manifests as gas bubbles visible on CT [2, 3]. The most common pathogen causing this condition is the bacterium E. coli [3]. This disease occurs most commonly in patients with uncontrolled diabetes. Studies in the last two decades show a very high mortality rate of 21% for this condition [4].
Case Presentation
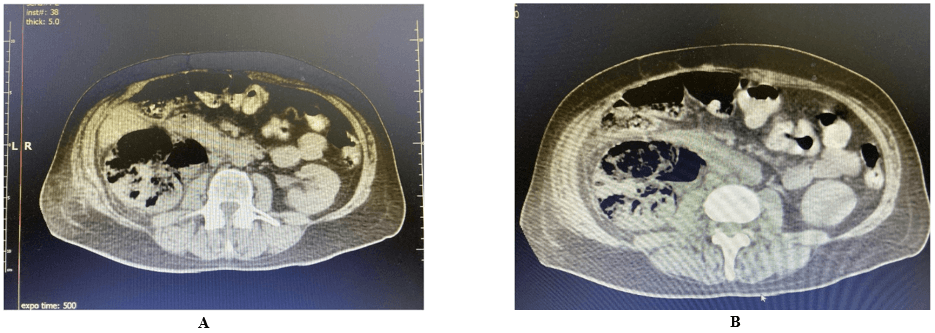
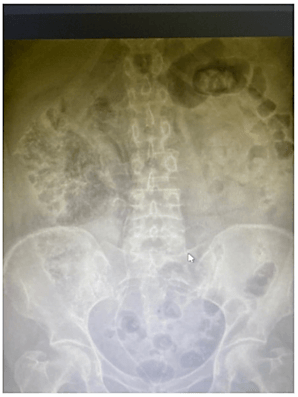
A 62-year-old female patient was transferred to the department of urology at the University Hospital in Zielona Góra from the Hospital Emergency Ward in Żary. Suspected EPN of the right kidney was diagnosed (Figures 1 & 2). The patient was admitted urgently to the department of urology. The patient had concomitant diseases: chronic coronary syndrome, chronic heart failure with ejection fraction (EF) 20%, myocardial damage of nonischaemic etiology, permanent atrial fibrillation, arterial hypertension and type 2 diabetes mellitus after surgical treatment of pancreatitis. The patient was urgently qualified for surgery. URS-L dex + DJ dex procedure was performed. The deposits were removed from the lower part of the right ureter and a DJ dex catheter was inserted. While in the urology department, the patient was connected to an insulin pump, and recorded sugar levels were 270-370 mg/dl. A central catheter was placed and levonor infusion was started. Cardiology, anaesthesiology, and diabetes consultations were also performed. Blood cultures were performed and antibiotic therapy with meronor and vancomycin was administered. Fluid therapy was also administered. The patient’s condition was severe; after another anaesthetic consultation, she was transferred to the intensive therapy unit. On day 4 at the University Hospital, nephrectomy was performed, and death occurred on the same day.
Figure 1: A & B) CT images presenting the accumulation of gas within the right kidney.
Figure 2: X-ray abdomen revealing gas in the right retroperitoneum.
Discussion
A patient aged 62 years was admitted with suspected EPN of the right kidney with associated deposits in the lower right ureter. Patients affected by this rare disease usually have multiple comorbidities. Our patient was burdened with chronic cardiovascular diseases, including chronic coronary syndrome, chronic heart failure with an ejection fraction of 20%, hypertension, and type II diabetes mellitus, which occurs in approximately 90% of patients with EPN. Blood glucose levels during hospitalization ranged from 270-370 mg/dL. The presence of comorbidities affects the prognosis of patients and correlates unfavourably with surgical treatment. This is due to the fact that patients requiring surgical treatment often have an unfavourable qualification for surgery related to comorbidities. Nephrectomy is performed because of the need to attempt to save the patient's life [5]. Gas-forming nephritis is a dangerous and rapidly progressive condition [2, 3]. It should be noted that an approach using antibiotic therapy in combination with drainage has a high success rate of up to 80% of patients. This type of treatment is referred to as kidney salvage therapy because it does not require nephrectomy [5]. It is also important to note that antibiotic therapy alone is associated with the highest mortality rate. Early nephrectomy in EPN has also been found to be a predictor of mortality [5].
Due to the environment in the kidney, antibiotic therapy should be directed against gram-negative bacteria [1]. In our patient, Meropenem and vancomycin were used empirically. Fluid therapy was also included. Blood cultures were taken for targeted antibiotic therapy. In severe conditions leading to sepsis, treatment management includes additional drainage, as monotherapy with antibiotics is associated with an increased risk of treatment failure [1, 2]. Urgent URS-L of the right kidney was performed, followed by placement of a DJ catheter. Due to multi-morbidity, the patient underwent cardiology consultation and norepinephrine treatment was started. Nephrectomy is used in patients whose condition does not improve despite antibiotic therapy, fluid therapy and drainage and there is a high likelihood of generalized infection [3, 5]. The classification of EPN is based on three models: Michaeli et al., Wan et al., and Huang and Tseng. The radiological classification according to Wan et al. and Huang and Tseng are based on CT scanning, while the model of Michaeli et al. refers to plain radiograph and intravenous pyelogram. For clinical applications, in our opinion, the classification according to Huang and Tseng seems to be very practical. It is divided into 4 classes. Class one involves gas present only in the collecting system, class two involves gas present only in the parenchyma, and class three is divided into subclasses A and B. Subclass A includes extension of gas into the parenchymal space, while subclass B includes extension of gas into the appendicular space. Class four describes EPN in single kidney disease or bilateral kidney disease.
Another classification using computed tomography is that developed by Wan et al. The first is associated with renal necrosis in which gas is present but no fluid. The second is parenchymal gas associated with fluid in the renal parenchyma, perinephric space, or collecting system. CT is considered to be the most effective diagnostic method for EPN [3]. Based on Huang and Tseng's classification, a CT-based therapeutic regimen was developed. This scheme assumes that KUB and ultrasonography can be performed beforehand. Then the developed scheme assumes that the clinical picture is assigned to one of the classes according to Huang and Tseng. The use of an algorithm for the management of EPN based on the Huang & Tseng clinical-radiological classification allows us to undertake therapeutic approaches that are beneficial to the patient [3]. In our clinical case, the patient was treated with antibiotic therapy along with drainage. Only as a result of the ineffectiveness of this method, according to the management scheme and current knowledge, the decision was made to perform nephrectomy. Unfortunately, due to the severe general condition of the patient, who was transferred to the intensive care unit before the procedure, death occurred.
Conclusion
Gas-forming nephritis (EPN) is a rare disease. In our case, death occurred despite standard management. This shows that general condition, age, and concomitant diseases have a significant effect on the outcome of treatment.
Competing Interests
None.
Article Info
Article Type
Case ReportPublication history
Received: Fri 11, Jun 2021Accepted: Tue 29, Jun 2021
Published: Wed 28, Jul 2021
Copyright
© 2023 Maciej Salagierski. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2021.07.07
Author Info
Jakub Szczepanski Jaroslaw Rysz Maciej Stroczynski Aras Almohammad Krzysztof Smigaj Maciej Salagierski
Corresponding Author
Maciej SalagierskiDepartment of Urology, Collegium Medicum, University of Zielona Gora, Zielona Gora, Poland
Figures & Tables
References
1. Li S, Wang J, Hu J, He L, Wang C (2018) Emphysematous pyelonephritis and
cystitis: A case report and literature review. J Int Med Res 46:
2954-2960. [Crossref]
2. Sharma PK, Sharma R, Vijay MK, Tiwari P, Goel A et al. (2013)
Emphysematous pyelonephritis: Our experience with conservative management in 14
cases. Urol Ann 5: 157-162. [Crossref]
3. Ubee SS, McGlynn L, Fordham M (2011) Emphysematous pyelonephritis. BJU
Int 107: 1474-1478. [Crossref]
4. Zhang Y, Zang GQ, Tang ZH, Yu YS (2015) EMPHYSEMATOUS PYELONEPHRITIS. Rev Inst Med Trop Sao Paulo 57: 368. [Crossref]
5. Deoraj S, Zakharious F, Nasim A, Missouris C (2018) Emphysematous pyelonephritis: outcomes of conservative management and literature review. BMJ Case Rep 2018: bcr2018225931. [Crossref]
