A Giant Left Common Iliac Artery Aneurysm with Endovascular Repair: A Case Report
A B S T R A C T
Common iliac artery aneurysm (CIAA) is a very rare entity, but with potentially disastrous evolution, aneurysm rupture or distal embolization. A specific management, surgical or endovascular procedure, is required. We present a case with a huge distal left common iliac artery aneurysm, in which the diagnosis was made incidentally during a weekly ultrasound examination, in spite of impressive dimensions, 9 cm diameter. The patient was then examined by 128- Slices computed tomography and angio-coronarography. Despite the attractive anatomy for direct surgery with resection of the aneurysm and restoration of the iliac tract through the interposition of a tubular prosthesis, due to the previous pathology of the patient with necrotizing fasciitis in the left lower limb and abdominal wall, endovascular intervention was decided. Because, the big size of the left common iliac artery aneurysm, located distally, with tortuosity of the left common iliac artery as well external iliac artery (EIA), permeable left internal iliac artery (IIA), extensive intra-aneurysmal thrombosis, endovascular procedure was complex and particular. The peculiarities of the case and the complex endovascular technique, with the placement of a stent graft on the infrarenal abdominal aorta, extended on both common iliac arteries, embolization of the left internal iliac artery and extension of the left arm on the external iliac artery, are described in this presentation.
Keywords
Isolated iliac artery aneurysm, endovascular aneurysm repair, stent-graft, coil embolization, amplatzer vascular plug
Introduction
Isolated iliac artery aneurysms comprise only 0.4% to 1.9% of all intra-abdominal aneurysms (estimated prevalence 0.008%-0.03%). In clinical series the prevalence is between 2, 2 -7, 8%, but abdominal aortic aneurysm (AAA) is associated in 30-40 % with common iliac artery aneurysms extension [1]. Majority of the abdominal aortic and iliac artery aneurysms are found incidentally by getting images of the abdomen echography or computer tomography for something else. Natural evolution can be catastrophic with aneurysm rupture and high mortality over 50%, (even with emergency surgery), visceral and neural compression and distal thrombus embolization [2]. For this reason, surgical or endovascular management is indicated when the aneurysm diameter is over 35 mm. If there’s pain or tenderness of the aneurysm or there’s back pain, surgery is done regardless of size.
Until recently, the surgical approach was the single choice for isolated iliac artery aneurysm, with aneurysm resection, Dacron graft interposition and preservation of internal iliac artery integrity, whenever possible [3]. In our times, the endovascular treatment of aneurysms has entered the routine arsenal of vascular surgery. Several new endovascular techniques have been proposed to preserve the IIA, including “bell-bottom” iliac limbs, the sandwich or double-barrel technique, the cross-chimney technique, and, more recently, the development of iliac branch devices [4].
Case Report
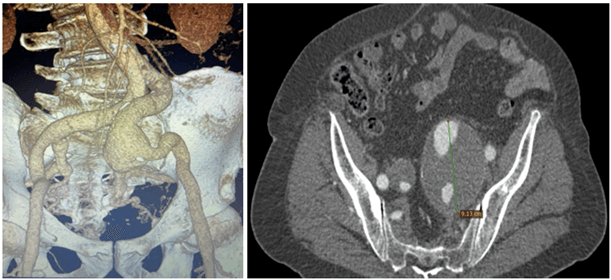
A 69-year-old patient, known to have a left thigh injury in 2005, with secondary necrotizing fasciitis that included the lateral face of the left thigh and ½ lower abdominal wall (surgical intervention and abdominal adherences), with grade II hypertension, grade I obesity (BMI = 34, 5Kg/m2), was diagnosed by incidentally abdominal echography and after 128- Slices Computer Tomography examination; with a huge distal left comon iliac artery aneurysm ~ 90 mm, tortuosity of the common and external iliac arteries on the both sides, open internal iliac artery bilateral. The femoral artery, external iliac and right common joint with straight trajectory, without tortuosity, with an average diameter of the straight common iliac artery of approximately 20 mm. The average diameter of the bilateral common femoral arteries is about 12 mm (Figure 1). Normal coronary on angio-coronarography examination.
Figure 1: Isolated distal left common iliac artery huge aneurysm, 9 cm diameter with iliac artery tortuosity.
Surgical expertise is performed and in spite of enticing iliac anatomy, due to the old pathology at the level of the lower abdominal floor - necrotizing fascia with the absence of the abdominal muscles at this level), contraindicates the surgical intervention. At this point, the interventional closure of the iliac artery aneurysm with a stent-graft is considered.
Due to the large diameter of the left common iliac artery (there are currently no such large diameter stent-grafts, and the large caliber difference between the left common iliac artery-20 mm and the left external iliac artery-16mm) it is decided that the only possible interventional solution is placement of an abdominal aortic stent-graft with extension on the right common iliac and extension to the left common and external iliac artery. Due to the short length of the shaft and the large diameter of the prosthesis to be able to place it by crossover from the right common femoral artery, it is considered the only viable solution to place an infrarenal graft stent with extension to the right common iliac artery and left external iliac.
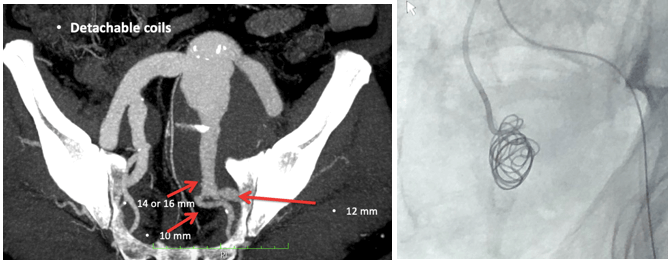
Selective cannulation of the ipsilateral left common iliac artery is attempted, without success due to severe tortuosity in the left external iliac artery and the presence of bifurcation aneurysm. It is then decided to crossover the cannulation of the left common iliac artery (due to its more favourable trajectory), which is performed with a vertebral catheter. At this level an Axium coil of 25mm / 50cm is placed, then 3 pieces of handmade coil from the Teflon guide of 0.035 are placed (Figure 2).
Figure 2: First coil placement on the left internal iliac artery.
Due to the severe tortuosity in the left external iliac artery, it is decided to place the main body, which has a larger caliber compared to the prosthesis extensions in the left external iliac artery (15F versus 13F), on the right common femoral artery, re-cannulation from the level of the left common femoral artery, the placement of an extension up to the bifurcation of the 22 mm straight common iliac artery (which arteries have a diameter of 15F), and the left placement of an extension of 12mm as initial diameter then continued to the external iliac with an extension of 14mm (strategy determined by the need to create a greater stability of the extension at the level of the aneurysm). Main body endograft Ovation ALTO 26 mm diameter and length 80 mm (Endologix LLC California, USA.) is placed through the right approach in the infrarenal abdominal aorta.
Then the left arm of the prosthesis is re-canulated, the extension Ovatio 22 / 160mm prosthesis, then left with an Ovatio 12 / 160mm prosthesis, then extends to the left external iliac with an Ovatio 14 / 120mm prosthesis, after 10 minutes the prosthesis is reset, with complete retraction to the left common iliac bifurcation, it is then extended to the distal left external iliac artery with an Ovatio 12 / 160mm prosthesis, post-dilated with a 12 / 40mm balloon at 4-8atm bilaterally. When withdrawing the left superstitious guide, the prosthesis is re-placed with the withdrawal of this up to the bifurcation. Control injection highlights the filling of the aneurysm completely, which is why it is decided to extend the prosthesis to the left common femoral artery in the proximal 1/3.
The left brachial approach is then performed, an adrenal multipurpose catheter is placed, then with a hydrophilic guide of 0.035 '' it is crossed in the left extension to the left common iliac artery, then the catheter is advanced and the guide is changed with a guide of 0.014 '' of 300 cm, it is advanced distally from the first 2 extensions, it is caught with a snare and it is externalized through the left sheath, then the intra-prosthetic vertebral catheter is placed, then the hydrophilic guide of 0.035'' is advanced in the ascending aorta, then it is changed with the guide super style Lunderquist, then the prosthesis is extended to the left communal femoral artery with an Ovatio 12 / 160mm prosthesis, postdilated with a 14 / 40mm balloon, with the retraction of the prosthesis after 15 'to the distal external iliac artery, control injection highlights sealing of the aneurysm, reason for which it is decided to complete the procedure, the 2 approach holes are closed with a proglide, then after the haemostasis the patient is transported to the salon.
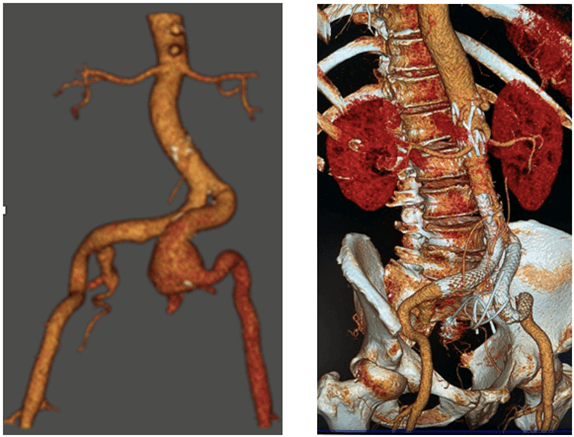
The ProGlide sutures were cinched down to close the arterial access without problems. The anticoagulation was reversed, and palpable distal pulses were noted in the extremity on completion of the procedure. Evolution after procedure was uneventful and 1-month CT- control shows; good position of the stent graft and no leaks (Figure 3).
Figure 3: Postoperative one month CT, showing good position of stent graft and no leaks.
Discussion
Aneurysm is defined as enlargement of the artery to a diameter of more than 1.5 cm normal diameter. Incidence is different, with aneurysm location; ascending aorta and the following segments, as well as all the arterial branches (carotid, intracerebral, visceral arteries, iliac arteries, femoral and distal branches). Isolated iliac artery aneurysm at autopsy estimates 0,03 and clinical prevalence 2,2-7,8 % [4].
Etiology is the common question of the patient and family, in special for young cases. The most common cause of IAA is atherosclerosis. Other etiology include trauma, infection, dissection, excessive athletic effort (bicycle racing), para-anastomotic graft failure, connective tissue disorders such as Marfan syndrome and Ehlers-Danlos syndrome. In case of very young patients with arterial aneurysms with an inherited connective tissue disorder, requires the patient’s family screening and counselling, close follow-up [5]. The aneurysm development on his natural evolution IAA consists of progressive expansion with eventual rupture, and the risk of rupture and death, compression around and distal embolism. Long time the aneurysm is asymptomatic or can mimic neurologic, genitourologic, and gastrointestinal symptoms due to external compression [6]. On the mean time with intravascular procedure development, some authors (Sakamoto), based on the anatomic features of the aneurysm and the complexity of endovascular option, suggested a different types of iliac artery aneurysm and internal iliac artery approach [2]. Endovascular repair of isolated IAAs is a minimally invasive alternative to open repair, in special cases when the open surgery is prohibited. New design of stent-graft, particular dimension, combination of branch-vessel, even for internal iliac artery, coil embolization has the potential to reduce perioperative morbidity and mortality, especially in high-risk patients [7].
Compared with surgical repair, endovascular repair of iliac artery aneurysms results in decreased length of stay, local anaesthesia, no intensive care stay, lower blood transfusion requirement, less complication (bleeding, infection) and similar intermediate-term results [8]. Patency of stent graft over 90% and freedom over 80 % at 5 years after stent graft implantation, are considered good results. Preoperative CT imaging provides a roadmap for customization of endovascular grafts for safe exclusion of the aneurysmal sac with preservation of the hypogastric artery and post- procedure to assess the stent position and leaks [9].
Technical success for EVAR cases is defined as successful endograft deployment with secure fixation and patency, and absence of leaks. In 2010, the Ovation Abdominal Stent Graft System has offered a new sealing concept, achieved by a sealing ring filled with polymer 13 mm from the renal arteries and the latest version with shorter now skirt 7mm, in 2020 [10].
Conclusion
Our case report proves that endovascular repair of iliac artery aneurysms has made fantastic progress, possible by improvements in technology and endovascular techniques. The endovascular treatment strategy should be mainly based on the particular anatomical features, the aneurysm location, size, combination with contralateral iliac artery, patency of internal iliac artery on both sides and customization of endovascular grafts for safe exclusion of the aneurysmal sac with preservation of the hypogastric artery. Technical modifications to the endograft, this new Ovation Alto stent graft, could allow for accommodation of a more comprehensive range of patient’s pathology. When classical surgical approach of this aneurysm, is not a choice then endovascular repair could be a safe and minimally invasive alternative and seems to be associated with fewer complications.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Sat 31, Dec 2022Accepted: Fri 20, Jan 2023
Published: Fri 03, Feb 2023
Copyright
© 2023 Marian Gaspar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JICOA.2023.01.01
Author Info
Marian Gaspar Laurentiu Pascalau Gianmarco De Donato
Corresponding Author
Marian GasparDepartment of Cardiovascular Surgery, Institute of Cardiovascular Disease, Timisoara, Romania
Figures & Tables
// 
References
1. Wanhainen A,
Verzini F, Van Herzeele I, Allaire E, Bown M et al. (2019) Editor's Choice -
European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines
on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur J Vasc
Endovasc Surg 57: 8-93. [Crossref]
2. Sakamoto I,
Sueyoshi E, Hazama S, Makino K, Nishida A et al. (2005) Endovascular Treatment
of Iliac Artery Aneurysms. RadioGraphics 25: S213-S227. [Crossref]
3. Wang W, Wu J, Shao
J, Xu F, Chen Y et al. (2021) Single-Center Experience in the Endovascular
Management of the Combination of Isolated Common and Internal Iliac Artery
Aneurysms. Front Surg 15: 693233. [Crossref]
4. Wu T, Lee JT (2016)
Evolution of Endovascular Management of Common Iliac Artery Aneurysms. Supplement
to Endovascular Today 15: 3-7.
5. Skopin II,
Arakelyan VS, Tchurikov NA, Belyaev AM (2021) A giant left internal iliac
artery aneurysm in a patient with Loeys-Dietz syndrome. Interact Cardiovasc
Thorac Surg 33: 832-833. [Crossref]
6. Patel NV, Long GW,
Cheema ZF, Rimar K, Brown OW et al. (2009) Open vs endovascular repair of
isolated iliac artery aneurysm: A 12-Years experience. J Vasc Surg 49:
1147-1153. [Crossref]
7. Chaer RA, Barbato
JE, Lin SC, Zenati M, Kent KC et al. (2008) Isolated iliac artery aneurysms: A
contemporary comparison of endovascular and open repair. J Vasc Surg 47:
708-713. [Crossref]
8. Hoo AS, Ryan L,
Neville R, Mukherjee D (2018) Customized endovascular repair of common iliac
artery aneurysms. J Vasc Surg Cases Innov Tech 4: 278-282. [Crossref]
9. Valente T, Rossi G, Rea G, Pinto A, Romano L et al. (2014) Multidetector CT Findings of Complications of Surgical and Endovascular Treatment of Aortic Aneurysms. Radiol Clin North Am 52: 961-989. [Crossref]
10. de Donato G, Pasqui E, Panzano C, Galzerano G, Cappelli A et al. (2021) Early Experience with the New Ovation Alto Stent Graft in Endovascular Abdominal Aortic Aneurysm Repair. EJVES Vasc Forum 54: 7-12. [Crossref]
