A Dramatic Relief from Cluster Headache by Classic Bloodletting Acupuncture Evidenced by Thermography Analysis: A Case Report
A B S T R A C T
Background: Cluster headache is a severe headache, which causes severe impairment in the quality of life of the patients. Here, we report a successful experience of relieving cluster headache by puncturing the superficial engorged venules of the ipsilateral leg.
Case presentation: This 72-year-old female with severe refractory cluster headache came from the United States to Taiwan to search for alternative therapy. Her headache was characterized by excruciating, stabbing pain on the left head, primarily around the orbital area with extension to temporal and occipital area, and accompanied with left nasal obstruction. Based upon the classic acupuncture method, her headache was dramatically and totally relieved by puncture upon superficial engorged venules of ipsilateral leg.
Conclusion: This case reminded us that classic bloodletting acupuncture could be an alternative strategy for cases with refractory cluster headache. Besides, the connection between leg engorged venules and head suggesting the existence of some novel reflex, worthy of investigation in the future.
Keywords
Acupuncture, bloodletting, headache, thermography, case report
Background
Cluster headache is a severe headache, which causes severe impairment in the quality of life of patients [1]. Some patients show poor response to standard medical treatment and then search for help from alternative therapy. Here, we report the first successful experience of relieving cluster headache by puncturing the superficial engorged venules of the ipsilateral leg.
Case Presentation
This 72-year-old female with a long history of intermittent headache for 60 years came from the United States to Taiwan due to severe refractory headache with slow progression for half a year. Her headache is characterized by excruciating, stabbing pain on the left head, primarily around the orbital area, extending to the temporal and occipital area, and accompanied with left nasal obstruction. She suffered a headache attack almost every day. She used to take 3 tablets of acetaminophen (500mg) for headache attack, but the therapeutic effect gradually decreased. Therefore, the patient came to our out-patient-department for help. According to the International Classification of Headache Disorders 3rd edition (ICHD-3) diagnostic criteria and her clinical features, she was diagnosed with chronic cluster headache.
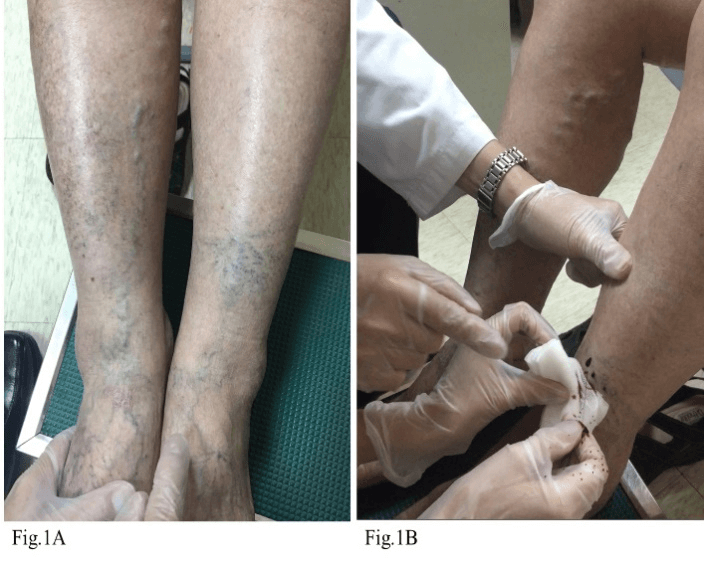
During inspection, a group of engorged venules was found at the anterior part of her left lower leg (Figure 1A), which was much different from the varicose veins on her right leg [2]. These aberrant venules were designated as Xue-Lo (blood-intermeridian in classic acupuncture), which is believed to be associated with chronic, refractory disorder in a traditional Chinese medicine bible, the Yellow Emperor’s Inner Classic. According to the meridian theory, the area involved in her headache and the location of the aberrant venules belonged to the same energy pathway, known as stomach meridian, which suggests that the management of the venules could be beneficial for her refractory cluster headache [3].
Figure 1: Engorged venules and the procedure of bloodletting acupuncture. A) A group of engorged venules was found at the anterior part of the patient’s left lower leg, which was much different from the varicose veins on her right leg. B) We applied a classic acupuncture technique known as bloodletting acupuncture, Lo-Tzu (Intermeridian-Puncture), to puncture the group of venules on the left lower anterior leg, and a total of 10 ml of blood was spilled from the puncture site.
Therefore, we applied a classic acupuncture technique known as Lo-Tzu (Intermeridian-Puncture) to puncture the aberrant venules of the left leg. By aseptic procedure, a 22-gauge needle was used to puncture the group of venules on the left lower anterior leg (Figure 1B). A total of 10 ml of blood was spilled from the puncture site. Ten minutes later, the pain score of headache decreased from the visual analogue scale (VAS) 80/100 mm to VAS 20/100 mm.
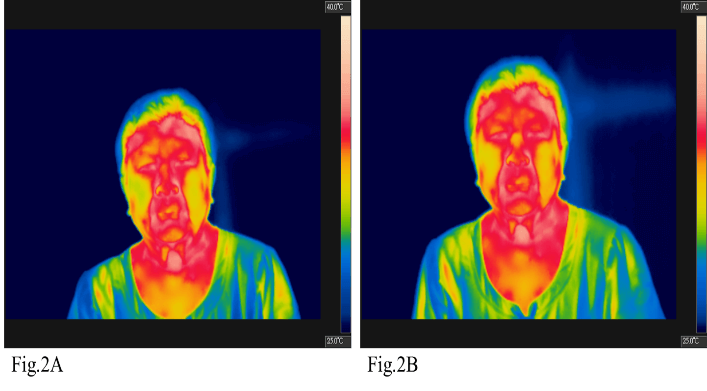
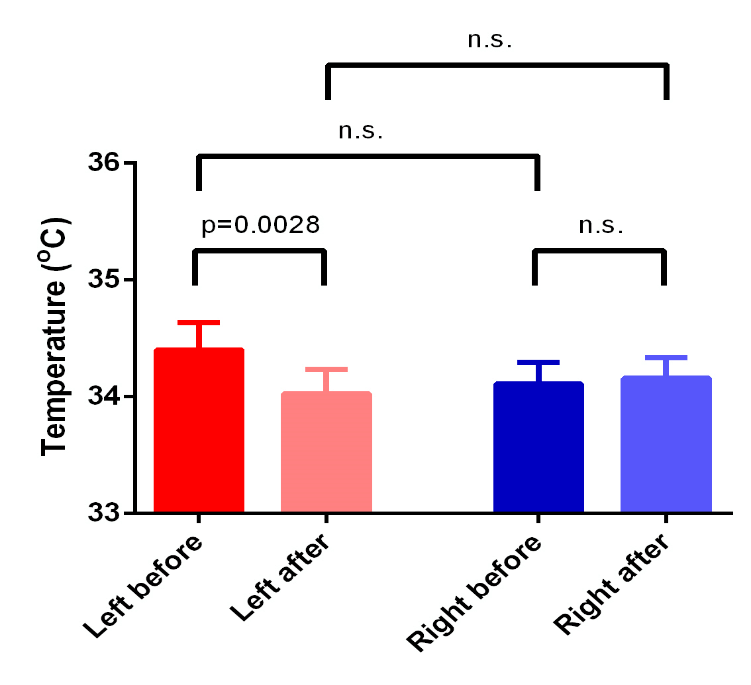
Moreover, her left nasal obstruction subsided, and significant decrease of facial temperature was found by thermography. Obviously, the yellow zone of nasal base is broader in (Figure 2B) compared with (Figure 2A). Furthermore, based upon thermography of acupoints on the face {[BL-1; Jingming], [BL-2; Zanzhu], [GB-14; Yangbai], [EX-HN5; Taiyang], [LI-20; Yingxiang], [TE-23; Sizhukong], [GB-1; Tongziliao], [ST-1; Chengchi], [ST-2; Ssupai], [ST-3; Chuliao], [ST-4; Titsang], [EX-HN4; Yuyao], according to World Health Organization (WHO) standardization of acupuncture nomenclature.}, all acupoints showed reduced temperature after bloodletting acupuncture and had significant difference (Table 1) (Figure 3). One week later, she returned to our clinic and reported being able to decrease the dosage of acetaminophen (500mg) from 21 tablets a week to only one tablet a week. The second bloodletting acupuncture upon the ipsilateral leg was performed. Two weeks later, she reported no more headache attack. Thereafter, she went back to the United States of America.
Figure 2: Temperature difference between before and after bloodletting acupuncture monitored by thermography. There is a significant decrease in facial temperature after the treatment of bloodletting acupuncture found by thermography. Obviously, the yellow zone of nasal base is broader in Figure 2B compared with Figure 2A, which means the temperature around the nasal base after treatment is lower than before.
Table 1: Comparison of the temperature of 12 sites before versus after bloodletting acupuncture treatment. We compared the facial temperature of 12 acupoints before versus after bloodletting acupuncture treatment by thermography. All acupoints showed reduced temperature after bloodletting acupuncture and had a significant difference.
|
|
Left |
Right |
||||
|
Acupoints |
Before (℃) |
After (℃) |
Difference |
Before (℃) |
After (℃) |
Difference |
|
BL-1; Jingming |
34.9 |
33.7 |
-1.2 |
34.8 |
34.1 |
-0.7 |
|
BL-2; Zanzhu |
34.1 |
33.8 |
-0.3 |
34.5 |
34.2 |
-0.3 |
|
GB-14; Yangbai |
34.6 |
34.2 |
-0.4 |
34.0 |
34.0 |
0.0 |
|
EX-HN5; Taiyang |
34.2 |
34.1 |
-0.1 |
33.6 |
33.4 |
-0.2 |
|
LI-20; Yingxiang |
35.7 |
35.5 |
-0.2 |
35.3 |
35.6 |
+0.3 |
|
TE-23; Sizhukong |
35.0 |
34.7 |
-0.3 |
34.2 |
34.3 |
+0.1 |
|
GB-1; Tongziliao |
35.1 |
34.2 |
-0.9 |
33.2 |
33.6 |
+0.4 |
|
ST-1; Chengchi |
34.7 |
34.3 |
-0.4 |
34.5 |
34.2 |
-0.3 |
|
ST-2; Ssupai |
34.0 |
33.7 |
-0.3 |
33.7 |
33.8 |
+0.1 |
|
ST-3; Chuliao |
32.6 |
32.5 |
-0.1 |
33.3 |
33.8 |
+0.5 |
|
ST-4; Titsang |
33.5 |
33.4 |
-0.1 |
34.6 |
35.0 |
+0.4 |
|
EX-HN4; yuyao |
34.4 |
34.2 |
-0.2 |
33.6 |
33.9 |
+0.3 |
|
Mean |
34.400 |
34.025* |
-0.375 |
34.108 |
34.158﹢ |
0.050 |
|
SD |
0.812 |
0.725 |
|
0.649 |
0.607 |
|
|
SEM |
0.235 |
0.209 |
|
0.187 |
0.175 |
|
*P < 0.005, 95% confidence interval of this difference from 0.160 to 0.590.
﹢P =0.6427, 95% confidence interval of this difference from -0.281 to 0.181.
Figure 3: Comparison of the facial temperature of left and right side before versus after bloodletting acupuncture treatment. According to the temperature of 12 acupoints before versus after the bloodletting acupuncture treatment, we could see a significant difference on her left side, which was her headache and nasal obstruction attacked side. The significant difference of temperature may provide evidence of dramatic relief after bloodletting acupuncture. This observation reminded us to explore further the connection between the effectiveness of bloodletting acupuncture and temperature difference in the future.
Discussion and Conclusion
Cluster headache is a severely painful headache, which causes severe impairment in the quality of life of patients. Current standard medical treatment for cluster headache includes steroid, verapamil, lithium, and valproic acid. Unfortunately, some patients show poor responses to the standard medical treatment and then seek help from alternative therapy. Acupuncture is one of the most well-known alternative therapy. Fofi et al. showed some significant improvement in acupuncture for cluster headache [4]. Although Cochrane review and United Kingdom National Institute for Health and Care Excellence recommend acupuncture as a prophylactic treatment for migraine and tension headache, the effectiveness for cluster headache remains unclear [5].
Bloodletting acupuncture (BLA) is a classical acupuncture method, according to the traditional Chinese medicine bible, the Yellow Emperor’s Inner Classic. As known, bloodletting acupuncture, which targets superficial engorged venules, is different from the conventional acupuncture, which targets acupoint [6, 7]. Bloodletting acupuncture can relieve the qi and blood stasis in the meridians by bleeding a little amount of blood. To our surprise, this classic bloodletting acupuncture therapy significantly relieved the refractory headache of our patient.
To date, the mechanism underlying the ipsilateral connection between the leg and the head remained unclear. Hardebo et al. noticed that cerebrospinal fluid (CSF) opioid levels may increase after manual acupuncture or electroacupuncture in cluster headache patients [8]. Neurotransmitters through CSF or bloodstream may be the possible explanation for traditional acupuncture theory, which chooses ipsilateral or contralateral distal acupoints to treat target lesion.
Apart from the CSF and bloodstream mechanism, the nerve conduction pathway should be considered. By the interneuron target in the spinal cord, there are two types of reflexes. The first is the ipsilateral reflex – central reflex activity stays on the same side of the spinal cord. The second is the contralateral reflex – afferent stimulus enters on one side, and efferent motoric exit on the other. In our case, BLA on left leg venules causes relief of the headache on the left side, which suggests the existence of ipsilateral reflex. However, the nervous network connecting the leg to the head remains unknown and warrants future studies.
Previously, Sherrington has described the phenomenon of intersegmental reflex, also known as long reflex [9]. In traditional Chinese medicine theories, there are some meridians going through head and legs, connecting to inner organs. Those meridian routes may be similar to intersegmental reflex. Intersegmental reflex means a spinal reflex arc in which the afferent (sensory) and efferent (motor) nerves are connected by different dermatomes of the spinal cord. According to our observation, using bloodletting acupuncture on the left leg engorged venules can relieve ipsilateral headache. Sherrington long reflex could be the possible explanation of the effect of bloodletting acupuncture via meridian routes. Recently, a human intersegmental reflex from intercostal afferents to scalene muscles was also found [10]. This phenomenon may be considered the explanation of meridians in the human body. These findings provide the route for intersegmental reflex between the leg and the head but needs further investigation in the future.
To our current knowledge, we propose that the engorged venules on the leg send some afferent information to the head via intersegmental reflex to aggravate the headache. Therefore, while bleeding the engorged venules resulted in decrease of pressure in the venules, there would be less stimulation transmitted, and, hence, the headache resolved. Though the real mechanism connecting the leg engorged venules and the head is unknown to date, this case reminded us that classic bloodletting acupuncture could be an alternative strategy for cases with refractory cluster headache and a further investigation might discover a novel reflex route between the leg and the head in the future.
Ethical Approval and Consent to Participate
We had appropriate permissions of pictures, video, and data from the patient.
Consent for Publication
To clarify the publication of this case report, we gave and explained informed consent to this patient. We obtained verbal consent and informed consent for publication written in Chinese. The patient signed her name in both Chinese and English. A copy of the written informed consent for publication of this case report is available in the appendix.
Availability of Data and Materials
The datasets during and analysed during the current study are available from the corresponding author on reasonable request.
Competing Interests
None.
Funding
The authors declare that they do not receive other funding for this research. All the resources of this article provided by Kaohsiung Medical University Chung Ho Memorial Hospital.
Author Contributions
Ya Ling Yang and Yu Chien Wu were major contributors in writing the manuscript. Huang Lung Lin directed the procedure of acupuncture and bloodletting acupuncture. Chung Jen Chen analysed the patient data and instructed writing the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors are very grateful to our patient, Miss Yeh. Without her encouragement, the manuscript may not publish and share with the world. We also thank Dr. Chun-Hsiang Tan, neurologist expert from the department of neurology in Kaohsiung Medical University Hospital for statistical advisement and the critically English proofreading for this manuscript.
Abbreviations
ICHD-3: International Classification of Headache Disorders 3rd edition
VAS: Visual Analogue Scale
WHO: World Health Organization
BLA: Bloodletting Acupuncture
CSF: Cerebrospinal Fluid
Article Info
Article Type
Case ReportPublication history
Received: Mon 18, May 2020Accepted: Wed 03, Jun 2020
Published: Mon 15, Jun 2020
Copyright
© 2023 Chung-Jen Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.06.10
Author Info
Chung-Jen Chen Huang-Lung Lin Ya-Ling Yang Yu-Chien Wu
Corresponding Author
Chung-Jen ChenCollege of Medicine, Kaohsiung Medical University, Taiwan, Republic of China (R.O.C.)
Figures & Tables
Table 1: Comparison of the temperature of 12 sites before versus after bloodletting acupuncture treatment. We compared the facial temperature of 12 acupoints before versus after bloodletting acupuncture treatment by thermography. All acupoints showed reduced temperature after bloodletting acupuncture and had a significant difference.
|
|
Left |
Right |
||||
|
Acupoints |
Before (℃) |
After (℃) |
Difference |
Before (℃) |
After (℃) |
Difference |
|
BL-1; Jingming |
34.9 |
33.7 |
-1.2 |
34.8 |
34.1 |
-0.7 |
|
BL-2; Zanzhu |
34.1 |
33.8 |
-0.3 |
34.5 |
34.2 |
-0.3 |
|
GB-14; Yangbai |
34.6 |
34.2 |
-0.4 |
34.0 |
34.0 |
0.0 |
|
EX-HN5; Taiyang |
34.2 |
34.1 |
-0.1 |
33.6 |
33.4 |
-0.2 |
|
LI-20; Yingxiang |
35.7 |
35.5 |
-0.2 |
35.3 |
35.6 |
+0.3 |
|
TE-23; Sizhukong |
35.0 |
34.7 |
-0.3 |
34.2 |
34.3 |
+0.1 |
|
GB-1; Tongziliao |
35.1 |
34.2 |
-0.9 |
33.2 |
33.6 |
+0.4 |
|
ST-1; Chengchi |
34.7 |
34.3 |
-0.4 |
34.5 |
34.2 |
-0.3 |
|
ST-2; Ssupai |
34.0 |
33.7 |
-0.3 |
33.7 |
33.8 |
+0.1 |
|
ST-3; Chuliao |
32.6 |
32.5 |
-0.1 |
33.3 |
33.8 |
+0.5 |
|
ST-4; Titsang |
33.5 |
33.4 |
-0.1 |
34.6 |
35.0 |
+0.4 |
|
EX-HN4; yuyao |
34.4 |
34.2 |
-0.2 |
33.6 |
33.9 |
+0.3 |
|
Mean |
34.400 |
34.025* |
-0.375 |
34.108 |
34.158﹢ |
0.050 |
|
SD |
0.812 |
0.725 |
|
0.649 |
0.607 |
|
|
SEM |
0.235 |
0.209 |
|
0.187 |
0.175 |
|
*P < 0.005, 95% confidence interval of this difference from 0.160 to 0.590.
﹢P =0.6427, 95% confidence interval of this difference from -0.281 to 0.181.
References
- Matthew S Robbins, Amaal J Starling, Tamara M Pringsheim, Werner J Becker, Todd J Schwedt (2016) Treatment of Cluster Headache: The American Headache Society Evidence-Based Guidelines. Headache 56: 1093-1106. [Crossref]
- Seshadri Raju, Peter Neglén (2009) Clinical practice. Chronic venous insufficiency and varicose veins. N Engl J Med 360: 2319-2327. [Crossref]
- Xu R (1990) The application of bloodletting in acupuncture therapy. J Trad Chin Med 10: 274-275.
- L Fofi, G Allais, P E Quirico, S Rolando, P Borgogno et al. (2014) Acupuncture in cluster headache: four cases and review of the literature. Neurol Sci 35: 195-198. [Crossref]
- Simon Hayhoe (2016) Acupuncture for episodic cluster headache: a trigeminal approach. Acupunct Med 34: 55-58. [Crossref]
- C J Chen, W C Tsai, J H Yen, J J Tsai, T T Ou et al. (2001) Bloodletting acupuncture of the engorged vein around Bl-40 (Wei-Chung) for acute lumbar sprain. Am J Chin Med 29: 387-391. [Crossref]
- Klaus Linde, Gianni Allais, Benno Brinkhaus, Yutong Fei, Michael Mehring et al. (2016) Acupuncture for the prevention of tension-type headache. Cochrane Database Syst Rev 4: Cd007587. [Crossref]
- J E Hardebo, R Ekman, M Eriksson (1989) Low CSF met-enkephalin levels in cluster headache are elevated by acupuncture. Headache 29: 494-497. [Crossref]
- Mann F (1973) Acupuncture: the ancient Chinese art of healing and how it works scientifically. Vintage.
- Rachel A McBain, Janet L Taylor, Robert B Gorman, Simon C Gandevia, Jane E Butler (2016) Human intersegmental reflexes from intercostal afferents to scalene muscles. Exp Physiol 101: 1301-1308. [Crossref]
