Journals
A Clinical Case Study and Review of the Literature on Stercoral Ulcer Perforation: An Uncommon but Deadly Culprit
A B S T R A C T
Stercoral ulcer perforation (SUP) was first described in 1894. Fewer than 150 cases have been reported in the literature. Historically, stercoral ulcers (SU) are mostly seen in older patients. However, in recent years younger patients have presented with this condition. Stercoral ulcers are caused by impacted feces, which result in loss of bowel wall integrity due to chronic pressure necrosis. This can lead to perforation and fecal peritonitis. It is a deadly but rare complication of chronic constipation.
The case of a 78-year-old woman with a history of chronic constipation who presented to the emergency department (ED) with diffuse abdominal pain is described. Initial imaging studies revealed severe fecal impaction, most significant in the sigmoid and rectum. The patient was admitted for observation with serial abdominal exams, however, during the hospital course her clinical status deteriorated over a 12-hour period. Abdominal x-ray demonstrated free air under the diaphragm, and the patient was taken to the operating room (OR) for emergency exploratory laparotomy. Colorectal perforation was discovered and repaired. The patient tolerated the surgical intervention, but unfortunately died during the post-operative period. The patient’s history of chronic constipation, immobility, and opioid use for pain management after knee surgery most likely precipitated the stercoral ulceration and colonic perforation.
In this study, a systematic review was conducted to assess the epidemiology, presentation, diagnosis, management, complications, and clinical implications associated with stercoral ulcers.
Introduction
Stercoral ulcer perforation (SUP) was first described by Berry in 1894 [1]. Fewer than 150 cases have been reported across the literature. Stercoral ulcer (SU) is defined as a colonic perforation secondary to pressure necrosis from a fecal mass [2]. History of chronic constipation and fecal impaction allows for fecalomas to form. Stercoral ulcers measure 1-10 cm and multiple ulcers are found in approximately 27% of cases [3]. The most common location for ulcer formation is at the rectosigmoid junction, particularly along the antimesenteric border and the anterior wall of the rectum proximal to the peritoneal reflection [2]. Perforation is most common in the sigmoid colon, accounting for 77% of cases [4]. While considered a rare entity, SUP accounts for approximately 3.2 of colonic perforations [5].
Pathophysiologically, stercoral ulcers are thought to be caused by increased intraluminal pressure and pressure necrosis of the intestinal wall caused by impacted “hard rock” stools. The pressure created causes compression of capillary flow along the antimesenteric border of the bowel, where blood flow from the vasa recta is easily compromised, resulting in progressive ischemia and necrosis [2, 6]. In rare occasions, the impacted stools can calcify into scybalas which have a very high likelihood of progressing to perforation [2].
In this study a review of the literature was conducted to assess the epidemiology, presentation, diagnosis, management, complications, and clinical implications associated with stercoral ulcer perforation. A PubMed search was performed using the phrases “stercoral ulcer perforation” and “stercoral ulceration”. A total of 98 articles were found, and 38 were included (Table 1). Criteria for inclusion consisted of articles written in English from 1998 to 2015, stercoral ulcer perforation not associated with other colonic pathology (e.g., diverticulitis, neoplasia), and chief complaint of abdominal pain and/or distention.
Table 1: Studies included and relevant findings.
|
Study |
Year |
No. of patients |
Mean age(years) |
Chronic constipation |
Surgery |
Hartmann’s procedure |
Resection and Primary anastomosis |
Mortality |
|
Brunkar |
2015 |
1 |
45 |
1 |
1 |
No |
1 |
0 |
|
Davis |
2015 |
1 |
67 |
1 |
1 |
NR |
NR |
1 |
|
Baltazar |
2015 |
1 |
87 |
1 |
1 |
1 |
0 |
0 |
|
Saksonov |
2014 |
13 |
66 |
13 |
9 |
3 total colectomy 2 L. and 1 R.hemicolectomy 1 anterior resection 2 sigmoidectomy |
NR |
6 |
|
Bhatt |
2014 |
1 |
55 |
1 |
1 |
1 |
0 |
0 |
|
Habeeb |
2014 |
1 |
73 |
1 |
1 |
1 |
0 |
0 |
|
Kim |
2013 |
2 |
70.5 |
2 |
2 |
2 |
0 |
0 |
|
Okullo |
2013 |
1 |
77 |
1 |
1 |
0 |
1 |
0 |
|
Kwag |
2013 |
1 |
83 |
1 |
1 |
1 |
0 |
0 |
|
Sakharpe |
2012 |
1 |
41 |
NR |
1 |
1 |
0 |
0 |
|
Kang |
2012 |
1 |
69 |
1 |
1 |
1 |
0 |
0 |
|
Baltazar |
2013 |
2 |
87.5 |
2 |
2 |
2 |
0 |
0 |
|
Falidas |
2011 |
1 |
82 |
1 |
1 |
1 |
0 |
0 |
|
Wu |
2011 |
10 |
77.1 |
8 |
10 |
NR |
NR |
7 |
|
Kumar |
2010 |
2 |
NR |
NR |
NR |
NR |
NR |
NR |
|
Nam |
2010 |
8 |
74 |
8 |
8 |
7 |
1 |
2 |
|
Haung |
2006 |
5 |
60.2 |
5 |
3 |
3 |
2 |
1 |
|
Heffernana |
2005 |
4 |
70 |
4 |
4 |
4 |
0 |
4 |
|
Haddad |
2005 |
3 |
61 |
3 |
3 |
3 |
0 |
0 |
|
Matsuo |
2002 |
2 |
45.5 |
1 |
2 |
2 |
0 |
0 |
|
Maurer |
2000 |
7 |
59 |
5 |
0 |
7 |
0 |
0 |
|
Oakeful |
2011 |
1 |
79 |
1 |
1 |
1 |
0 |
0 |
|
McHugh |
2011 |
1 |
17 |
1 |
1 |
1 |
0 |
0 |
|
Matsushita |
2011 |
1 |
39 |
1 |
1 |
1 |
0 |
0 |
|
Lin |
2011 |
1 |
76 |
1 |
Not operated |
Not operated |
Not operated |
1 |
|
Craft |
2011 |
1 |
70 |
1 |
Not operated |
Not operated |
Not operated |
1 |
|
Park |
2010 |
1 |
80 |
1 |
1 |
1 |
0 |
0 |
|
Sharma |
2010 |
1 |
67 |
0 |
1 |
1 |
0 |
0 |
|
Hsiao |
2010 |
1 |
75 |
0 |
1 |
1 |
0 |
0 |
|
Ucel |
2009 |
1 |
106 |
1 |
1 |
1 |
0 |
0 |
|
YaNo |
2008 |
1 |
77 |
1 |
1 |
1 |
0 |
1 |
|
Tsai |
2008 |
1 |
81 |
1 |
1 |
1 |
0 |
0 |
|
Arana |
2007 |
1 |
75 |
1 |
1 |
1 |
0 |
1 |
|
Lundy |
2006 |
1 |
25 |
1 |
1 |
1 |
0 |
0 |
|
Tessier |
2002 |
1 |
67 |
1 |
1 |
1 |
0 |
0 |
|
Patel |
2002 |
1 |
45 |
0 |
1 |
1 |
0 |
0 |
|
Exadactylos |
2001 |
1 |
62 |
1 |
Not operated |
Not operated |
Not operated |
1 |
|
Tokonuga |
1998 |
1 |
60 |
0 |
1 |
0 |
1 |
0 |
|
* NR: Not reported |
||||||||
Case Report
A 78-year old female presented to the emergency department (ED) complaining of diffuse abdominal pain. On physical exam, her abdomen was soft, distended and tender to palpation, especially in the right lower quadrant. Medical history was significant for 10 years of chronic constipation, hypertension, diabetes mellitus, peripheral neuropathy, and Charcot joints. Surgical history included a recent knee surgery for which she was on opiates for pain control. Family history was noncontributory.
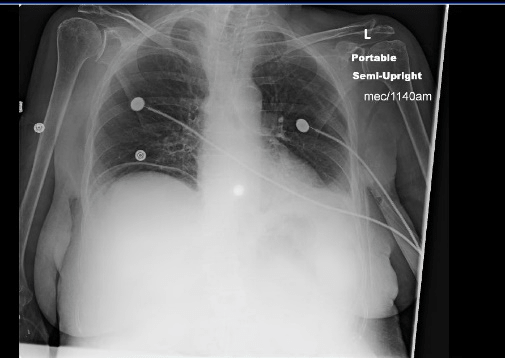
X-ray and computed tomography (CT) scan of the abdomen revealed severe fecal impaction, particularly in the sigmoid colon and rectum. There was no radiographic evidence of perforation, free peritoneal air, fecal spillage, or any other acute process. The patient was admitted for observation, and managed conservatively, with fluid resuscitation, fecal disimpaction, and serial abdominal x-rays. Over subsequent hours, the patient’s abdominal exam worsened; she developed peritoneal signs, tachycardia, hypotension, and shock. A repeat x-ray was obtained, significant for free peritoneal air under the diaphragm. Due to an INR of 14, the patient could not be taken to the operating room for emergency laparotomy, thus, she was transferred to the intensive care unit (ICU) for medical optimization.


After successful reversal of anticoagulation, the patient was taken for exploratory laparotomy. Perforation of the proximal rectum with gross ischemia and fecal spillage above the peritoneal reflection was diagnosed intraoperatively. The resection area included necrotic bowel extending from the sigmoid colon apex to the proximal rectum. After copious peritoneal irrigation, a wound VAC was placed in anticipation of a second look surgery.
The patient returned to the ICU, with unstable vital signs. She received several blood transfusions and required vasopressors for blood pressure support. Despite aggressive medical and surgical management, the patient developed pulseless electrical activity and died soon after. Pathologic results of the surgical specimen revealed perforation, inflamed mucosa, and ischemic necrosis of the intestinal wall.
Epidemiology
The incidence of stercoral ulcer perforation is most commonly seen in patients who are frail, bed-bound, narcotic dependent, chronically dehydrated, and challenged. Interestingly, being, in a long-term care facility resident is a predisposing factor [7]. The greatest single risk factor across the literature is chronic constipation, present in 81% of patients [1, 7, 8]. Previous post-mortem autopsies have revealed 1.3% to 5.7% of older patients have evidence of possible stercoral ulcer perforation [9]. Age at presentation ranges from 22 to 85 years old, with a mean of 59 years. The incidence is equal both for men and women [10]. The most common drugs prescribed in patients with SUP include opioids, tricyclic antidepressants, and anticholinergics [11]. Non-steroidal anti-inflammatory drugs have also been associated with stercoral ulcer perforation due to decreased protection of the mucosal lumen [12].
Clinical presentation
Non-perforated stercoral ulcers are usually silent. When symptoms develop it presents with altered mental status, and symptoms associated with fecal impaction including diffuse or localized abdominal pain, nausea, vomiting, rectal discomfort, fecal incontinence, and constipation [13, 14]. However, diagnosis is usually made during exploratory laparotomy [11]. In a survey of 38 cases of SUP only 8% of cases were diagnosed preoperatively [15]. The most common association across the literature is chronic constipation. Less commonly, fever, nausea, vomiting, and sepsis can also occur [16]. In many cases, an abdominal mass can be palpated during physical examination. In patients with perforated stercoral ulcers, gross rectal bleeding, or bloody stools is often accompanied by rapidly progressing signs of peritoneal inflammation [7]. Timely diagnosis is important due to the high risk of mortality, reported to range from 32% to 60% [5].
Diagnosis and Imaging studies
SUP can be diagnosed with the criteria proposed by Maurer et al in 1999 (Table 2) [1]. He conducted a study that evaluated 1295 patients who underwent colorectal surgery from 1993 to 1998, of which 566 (44%) were emergencies, 220 (17%) were caused by colonic perforation, and 7 perforations were due to SUP (3.1%) [1]. CT scan is the imaging modality of choice to accurately identify and diagnose SUP. CT scan findings include focal areas of fecal accumulation within the colon, mural enhancement, and thickening of the bowel wall due to associated mucosal inflammation [17]. Protrusion of a fecaloma through a perforated ulcer is diagnostic [1, 11]. Non-specific findings include pericolic stranding, and perfusion defects. It is important to distinguish imaging findings of SUP and non-perforated fecal impaction. In cases of non-perforated fecalomas, initial CT scan reveals increased thickness of the colonic wall secondary to inflammation and edema. When perforation occurs, CT scan findings consist of a markedly thin bowel wall from distention caused by the fecal mass. Moreover, perforation can be suspected when there is discontinuity of the colonic wall, with or without fecal spillage in the peritoneal cavity. In most cases of perforation, CT scans show intraperitoneal feces, extra-luminal gas, and free-air under the diaphragm, in 13%, 61%, and 90% of cases respectively [18]. Across the literature, authors agree that diagnosis of SUP can be made via CT scan, based on the presence of discontinuity of the bowel wall, focal colonic distention, and surrounding identifiable fecaloma [17]. Plain abdominal x-ray is commonly obtained and can demonstrate pneumomediastinum, evidence of fecal impaction, and calcified fecaloma. Pneumoperitoneum is seen in 70% of patients with SUP [1, 19].
Table 2: Proposed Maurer’s criteria for diagnosis of SUP*
|
Maurer et al suggested criteria for the diagnosis of SUP* |
|
|
|
|
|
* SUP: Stercoral ulcer perforation. |
Management
The appropriate management of stercoral ulcers has been widely debated across the literature. When perforation is not present, fecal impaction can be managed conservatively to reduce the risk of SUP in the future. Studies have shown that gastrograffin enemas can be both diagnostic and therapeutic for disimpaction of the fecal mass [17]. Surgical management consists of resection of the perforated bowel segment along with extensive peritoneal irrigation. It is considered the standard of care. SUP is associated with nearly 100% mortality when nonoperative treatment is sought, compared to 35% to 40% with surgery [12, 20, 21]. Surgical intervention with Hartmann’s closure is associated with a mortality rate of 32%, while colostomy only, and proximal colostomy have mortality rates of 43%, and 57% respectively [22].
Conclusion
SUP is a rare complication of chronic constipation that is not well understood. However, mortality rates are high, and awareness of this entity is important as it may allow timelier recognition. Clinicians should be aware and pay close attention to older patients with chronic constipation, optimize treatment for bowel evacuation in a timely manner, and prevent catastrophic complications which can result in death.
Article Info
Article Type
Case Report and Review of the LiteratureArticle History
Received Date: 29 November, 2018Accepted Date: 8 December, 2018
Published Date: 29 April, 2019
Copyright
© 2018 Vanita Ahuja. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2018.03.024
Author Info
Corresponding author
Vanita AhujaMD, MPH, MBA, FACS, Department of Surgery, Sinai Hospital, Hoffberger Building, 2401 W Belvedere Ave, Baltimore, MD 21215, USA.
Figures & Tables


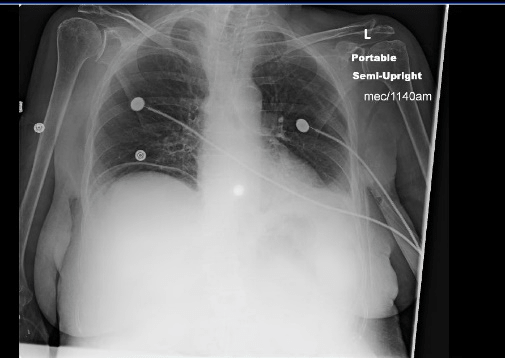
Table 1: Studies included and relevant findings.
|
Study |
Year |
No. of patients |
Mean age(years) |
Chronic constipation |
Surgery |
Hartmann’s procedure |
Resection and Primary anastomosis |
Mortality |
|
Brunkar |
2015 |
1 |
45 |
1 |
1 |
No |
1 |
0 |
|
Davis |
2015 |
1 |
67 |
1 |
1 |
NR |
NR |
1 |
|
Baltazar |
2015 |
1 |
87 |
1 |
1 |
1 |
0 |
0 |
|
Saksonov |
2014 |
13 |
66 |
13 |
9 |
3 total colectomy 2 L. and 1 R.hemicolectomy 1 anterior resection 2 sigmoidectomy |
NR |
6 |
|
Bhatt |
2014 |
1 |
55 |
1 |
1 |
1 |
0 |
0 |
|
Habeeb |
2014 |
1 |
73 |
1 |
1 |
1 |
0 |
0 |
|
Kim |
2013 |
2 |
70.5 |
2 |
2 |
2 |
0 |
0 |
|
Okullo |
2013 |
1 |
77 |
1 |
1 |
0 |
1 |
0 |
|
Kwag |
2013 |
1 |
83 |
1 |
1 |
1 |
0 |
0 |
|
Sakharpe |
2012 |
1 |
41 |
NR |
1 |
1 |
0 |
0 |
|
Kang |
2012 |
1 |
69 |
1 |
1 |
1 |
0 |
0 |
|
Baltazar |
2013 |
2 |
87.5 |
2 |
2 |
2 |
0 |
0 |
|
Falidas |
2011 |
1 |
82 |
1 |
1 |
1 |
0 |
0 |
|
Wu |
2011 |
10 |
77.1 |
8 |
10 |
NR |
NR |
7 |
|
Kumar |
2010 |
2 |
NR |
NR |
NR |
NR |
NR |
NR |
|
Nam |
2010 |
8 |
74 |
8 |
8 |
7 |
1 |
2 |
|
Haung |
2006 |
5 |
60.2 |
5 |
3 |
3 |
2 |
1 |
|
Heffernana |
2005 |
4 |
70 |
4 |
4 |
4 |
0 |
4 |
|
Haddad |
2005 |
3 |
61 |
3 |
3 |
3 |
0 |
0 |
|
Matsuo |
2002 |
2 |
45.5 |
1 |
2 |
2 |
0 |
0 |
|
Maurer |
2000 |
7 |
59 |
5 |
0 |
7 |
0 |
0 |
|
Oakeful |
2011 |
1 |
79 |
1 |
1 |
1 |
0 |
0 |
|
McHugh |
2011 |
1 |
17 |
1 |
1 |
1 |
0 |
0 |
|
Matsushita |
2011 |
1 |
39 |
1 |
1 |
1 |
0 |
0 |
|
Lin |
2011 |
1 |
76 |
1 |
Not operated |
Not operated |
Not operated |
1 |
|
Craft |
2011 |
1 |
70 |
1 |
Not operated |
Not operated |
Not operated |
1 |
|
Park |
2010 |
1 |
80 |
1 |
1 |
1 |
0 |
0 |
|
Sharma |
2010 |
1 |
67 |
0 |
1 |
1 |
0 |
0 |
|
Hsiao |
2010 |
1 |
75 |
0 |
1 |
1 |
0 |
0 |
|
Ucel |
2009 |
1 |
106 |
1 |
1 |
1 |
0 |
0 |
|
YaNo |
2008 |
1 |
77 |
1 |
1 |
1 |
0 |
1 |
|
Tsai |
2008 |
1 |
81 |
1 |
1 |
1 |
0 |
0 |
|
Arana |
2007 |
1 |
75 |
1 |
1 |
1 |
0 |
1 |
|
Lundy |
2006 |
1 |
25 |
1 |
1 |
1 |
0 |
0 |
|
Tessier |
2002 |
1 |
67 |
1 |
1 |
1 |
0 |
0 |
|
Patel |
2002 |
1 |
45 |
0 |
1 |
1 |
0 |
0 |
|
Exadactylos |
2001 |
1 |
62 |
1 |
Not operated |
Not operated |
Not operated |
1 |
|
Tokonuga |
1998 |
1 |
60 |
0 |
1 |
0 |
1 |
0 |
|
* NR: Not reported |
||||||||
Table 2: Proposed Maurer’s criteria for diagnosis of SUP*
|
Maurer et al suggested criteria for the diagnosis of SUP* |
|
|
|
|
|
* SUP: Stercoral ulcer perforation. |
References
1. Maurer CA, Renzulli P, Mazzucchelli L, Egger B, Seiler CA, et al. (2000) Use of accurate diagnostic criteria may increase incidence of spectral perforation of the colon. Dis Colon Rectum 43: 991-998. [Crossref]
2. Chung CH, Huang CC, Chiu HH, Huang CC, Chen JS (2011) Endoscopic evolution of rectal stercoral ulcer presenting with a large bleeding pseudodiverticulum in a patient with chronic constipation. Endoscopy 77-78. [Crossref]
3. Lundy JB, Gadacz TR (2006) Massive fecal impaction presenting with megarectum and perforation of a stercoral ulcer at the rectosigmoid junction. South Med J 99: 525-527. [Crossref]
4. Grinvalsky HT, Bowerman CI (1959) Stercoraceous ulcers of the colon: Relatively neglected medical and surgical problem. J Am Med Assoc 171: 1941-1946. [Crossref]
5. Serpell JW, Nicholls RJ (1990) Stercoral perforation of the colon. Br J Surg 77: 1325-1329. [Crossref]
6. Knigge KL, Katon RM (1997) Massive hematochezia from a visible vessel within a stercoral ulcer: effective endoscopic therapy. Gastrointest Endosc 46: 369-370. [Crossref]
7. Brombacher GD, Murray WR (1998) Emergency subtotal colectomy for chronic constipation. Scott Med J 43: 21-22. [Crossref]
8. Huang WS, Wang CS, Hsieh CC, Lin PY, Chin CC, et al. (2006) Management of patients with stercoral perforation of the sigmoid colon: report of five cases. World J Gastroenterol 12: 500-503. [Crossref]
9. Madan P, Bhayana S, Chandra P, Hughes JI (2008) Lower gastrointestinal bleeding: associated with Sevelamer use. World J Gastroenterol 14: 2615-2616. [Crossref]
10. Monika Sharma, Anjali Agrawal (2010) Case report: Stercoral sigmoid colonic perforation with faecal peritonitis. Indian J Radiol Imaging 20: 126-128. [Crossref]
11. Canders CP, Shing R, Rouhani A (2015) Stercoral colitis in two young psychiatric patients presenting with abdominal pain. J Emerg Med 49: 99-103. [Crossref]
12. Hollingworth J, Alexander Williams J (1991) Non-steroidal antiinflammatory drugs and stercoral perforation of the colon. Ann R Coll Surg Engl 73: 337-340. [Crossref]
13. Kumar P, Pearce O, Higginson A (2011) Imaging manifestations of faecal impaction and stercoral perforation. Clin Radiol 66: 83-88. [Crossref]
14. Gough AE, Donovan MN, Grotts J, Greaney GC (2016) Perforated stercoral ulcer: A 10-year experience. J Am Geriatr Soc 64: 912-914. [Crossref]
15. Hatzaras IS, Armen S, Dudrick SJ (2008) Perforated stercoral ulcer of the sigmoid colon. South Med J 101: 1072-1073. [Crossref]
16. Saksonov M, Bachar GN, Morgenstern S, Zeina AR, Vasserman M, et al. (2014) Stercoral colitis: a lethal disease computed Tomographic findings and clinical characteristic. J Comput Assist Tomogr 38: 721-726. [Crossref]
17. Baltazar G, Sahinoglu S, Betler M, Huynh M, Chendrasekhar A (2012) Rectal stercoral ulcer perforation. Am Surg 78: 515-516. [Crossref]
18. Chakravartty S, Chang A, Nunoo-Mensah J (2013) A systematic review of stercoral perforation. Colorectal Dis 15: 930-935. [Crossref]
19. Cheng-Hsien Wu, Li Jen Wang, Yon-Cheong Wong, Chen Chih Huang, Chien Cheng Chen, et al. (2011) Necrotic stercoral colitis: importance of computed tomography findings. World J Gastroenterol 17: 379-384. [Crossref]
20. Rozenblit AM, Cohen-Schwartz D, Wolf EL, Foxx MJ, Brenner S (2000) Case Reports: Stercoral perforation of the sigmoid colon: computed tomography findings. Clin Radiol 55: 727-729. [Crossref]
21. Bhatt VR, Murukutla S, DiPoce J, Gustafson S, Sarkany D, et al. (2014) Perforation in a patient with stercoral colitis and diverticulosis: who did it? J Community Hosp Intern Med Perspect 17: 4. [Crossref]
22. Celayir MF, Köksal HM, Uludag M (2017) Stercoral perforation of the rectosigmoid colon due to chronic constipation: A case report. Int J Surg Case Rep 40: 39-42. [Crossref]
