Journals
A case series of penetrating laryngeal trauma managed without tracheotomy
A B S T R A C T
Background: This study is a case series that involves two patients with penetrating laryngeal trauma managed without tracheotomy. Laryngeal trauma is a rare but potentially life-threatening injury. Injuries involving Zone II of the neck are classically managed with a tracheotomy. Our aim is to illustrate that in select cases Zone II laryngeal trauma can be surgically managed conservatively without tracheotomy or stenting.
Case Presentation: The two patients presented in this study both had penetrating trauma to the anterior neck in zone 2. While they were not in distress, both had subcutaneous air, loss of laryngeal prominence on exam, and fracture of the thyroid cartilage. In both cases the airway was secured via awake fiberoptic intubation, neck exploration and fracture fixation performed using sutures and microplates via a single incision through an extension of the original traumatic wound. Esophagoscopy was performed at the time of exploration and a brief period of endotracheal intubation was used to manage the airway, avoiding the use of laryngeal stenting.
Conclusion: In select cases zone II/Schaefer-Fuhrman group 3 laryngeal trauma can be surgically managed without tracheotomy or stenting, without compromising the basic tenets of airway management and patient safety. The above management led to a shorter hospital stay than advocated for in the literature and improved cosmetic outcome without any adverse voice or swallowing outcomes.
K E Y W O R D S
Larynx, neck injuries, fracture fixation, wounds, penetrating, laryngeal cartilage
Background
While variability exists in the management of laryngeal trauma likely due to the heterogeneous manner in which it presents, the first priority in all management pathways is to first secure the airway and address the injuries to the larynx and associated structures.
The management of penetrating injuries to the neck has traditionally been taught according to anatomically defined zones. Zone I involve the region between the clavicles and the cricoid cartilage, zone II from the cricoid cartilage to the angle of the mandible, and zone III from the angle of the mandible to the skull base [1]. Given the unique anatomical structures within each zone, the management algorithm for penetrating neck trauma is largely dictated based on the zone of injury. Classically, penetrating injuries in Zone II that violate the platysma require neck exploration in the operating room [1]. Other indications for surgical exploration include expanding hematoma, bruit, subcutaneous emphysema, and stridor [2]. Another framework for laryngeal injuries is the Schaefer-Fuhrman classification system [3], which divides laryngeal injuries into 5 categories, outlined in Table 1. Group 1 are generally managed medically, while group 2 may be managed conservatively with serial examinations, although some require tracheotomy. Group 3-5 are generally managed surgically; group 4 typically require stent placement, and Group 5 injuries are often fatal and those patients who survive require complex surgical repairs [3].
|
Severity of Injury |
|
|
Group 1 |
Minor endolaryngeal hematomas or lacerations without detectable fractures |
|
Group 2 |
More severe edema, hematoma, minor mucosal disruption without exposed cartilage, or nondisplaced fractures |
|
Group 3 |
Massive edema, large mucosal lacerations, exposed cartilage, displaced fractures, or vocal cord immobility |
|
Group 4 |
Same as group 3, but more severe, with disruption of anterior larynx, unstable fractures, two or more fracture lines, or severe mucosal injuries |
|
Group 5 |
Complete laryngotracheal separation |
|
|
|
Table 1: Schaefer Classification System [3]
The objective of this case report is to present two cases of penetrating laryngeal trauma involving zone II/Schaefer-Fuhrman group 3 that were managed by a conservative surgical approach without tracheotomy. Injuries involving this zone are classically managed with a tracheotomy, and the nature of the fractures usually requires laryngeal stenting [4]. We aim to illustrate, in select cases, how zone II/Schaefer-Fuhrman group 3 laryngeal trauma can be surgically managed without tracheotomy or stenting, without compromising the basic tenets of airway management and patient safety.
Case Report
Patient #1
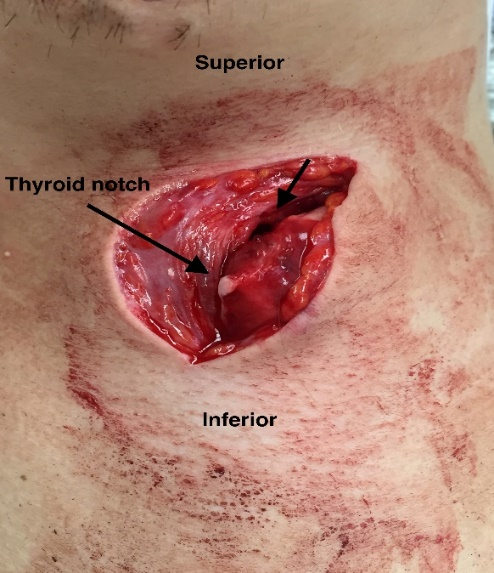
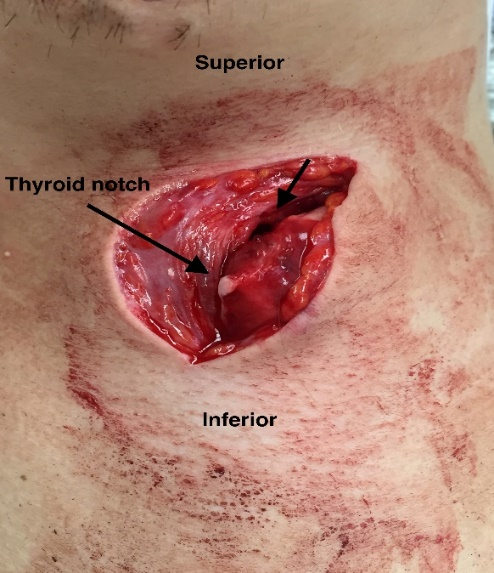
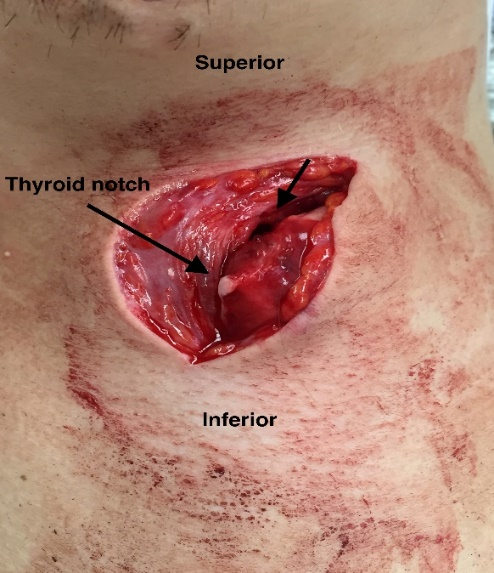
A 17-year-old intoxicated male presented to the Emergency Department with a neck laceration; he reported that he had collapsed on a ceramic mug while seated at his desk at home. He complained of hoarseness but denied any other symptoms. His vital signs were within normal limits and he was in no acute respiratory distress. On exam, he had an inverted L-shaped wound on his anterior neck in zone II that was transversely disrupting the thyrohyoid membrane and the upper half of his thyroid cartilage in the right paramedian area (Figure 1). Flexible laryngoscopy was performed in the emergency department demonstrating mild right vocal cord edema but no mucosal lacerations or exposed cartilage.
Given the extent of his injury, he was brought to the operating room on an emergent basis with no prior imaging and an awake fiberoptic intubation was performed by an experienced anaesthesia team using a size 6.5 endotracheal tube with the otolaryngology team on standby for possible awake tracheostomy. Direct laryngoscopy was unremarkable with intact laryngeal mucosa. There were no mucosal injuries to the glottis or supraglottic. Rigid Esophagoscopy was normal. Examination of the neck wound under anaesthesia revealed a penetrating injury with a large laceration of the thyrohyoid membrane as well as a displaced fracture of the right thyroid ala just lateral to midline.
Open reduction and internal fixation of the thyroid cartilage fracture was performed. The pre-existing wound was utilized to access the right paramedian fracture site. A titanium microplate was initially fashioned, but the thyroid cartilage was not yet ossified, and the self-drilling screws did not anchor tightly, even using “emergency” screws as described by Thor and Linder in 2007 [4]. Two 2-0 PDS interrupted sutures were therefore used to approximate the fracture sites. Repeat laryngoscopy confirmed proper alignment. The thyrohyoid membrane was repaired with absorbable sutures and the wound was closed in layers over a Penrose drain to prevent subcutaneous emphysema. The patient was kept intubated in the ICU post-operatively and was treated with antibiotics. On post-operative day 3, he was successfully extubated without complication. Flexible nasolaryngoscopy was done post extubation showing normal glottic mucosa. An NG tube was kept in place for feeding until a gastrograffin esophagram was performed on post-operative day 4, which showed no evidence of penetration or aspiration. He was then transitioned to an oral diet and was sent home six days after surgery. His voice was still slightly hoarse, but he had no difficulty breathing or dysphagia. Unfortunately, no long-term follow was completed as the patient failed to show up for his follow up appointments.
Patient #2
A 24-year-old male suffered a stab wound to his anterior neck in zone II. He presented to the emergency department by ambulance. On arrival, he was intoxicated but awake and alert with stable vital signs and in no acute respiratory distress. He had no recollection of his injury. He was able to speak in full sentences but was noted to be dysphonic despite having no complaints of difficulty breathing. He did however complain of a crackling sensation and pain in his neck after an episode of coughing.
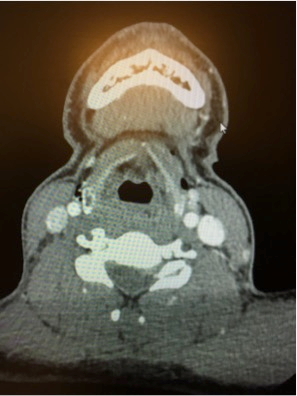
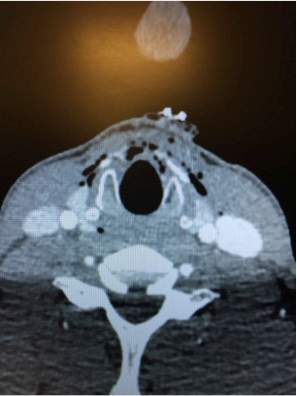
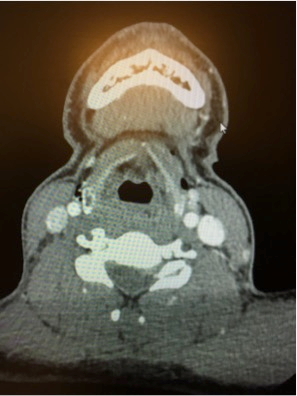
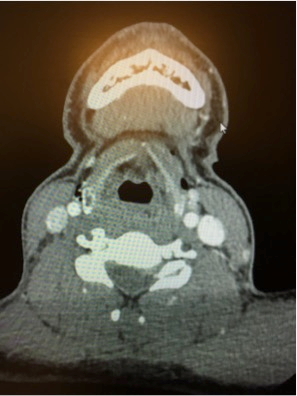
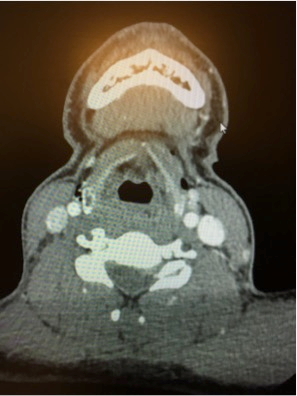
On examination, there was a small open wound violating the platysma at the level of the thyroid cartilage (Figure 2). Subcutaneous air was noted in the mid neck down to the clavicles and he had loss of the laryngeal prominence. Flexible laryngoscopy at the bedside showed a left vocal cord hematoma with no associated misalignment or vocal cord paresis. A contrast-enhanced CT scan of the neck from arch to vertex showed subcutaneous emphysema and a displaced fracture of the thyroid lamina (Figure 3 & 4).

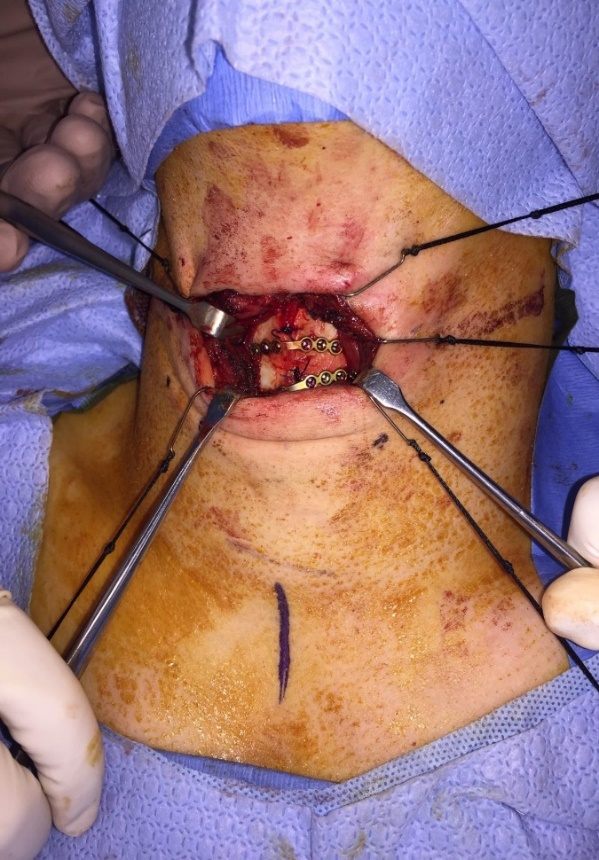
The patient was brought to the operating room and the airway was secured by an experienced anaesthesiology team via awake fiberoptic intubation using a size 7.5 endotracheal tube, with the otolaryngology team on standby for possible awake tracheostomy. Direct laryngoscopy and rigid esophagoscopy revealed a small mucosal laceration at the level of the anterior commissure and a left vocal cord haemorrhage but was otherwise unremarkable. Open reduction and internal fixation of the thyroid cartilage fracture was performed utilizing the original wound with a slight extension to provide access. The injury had resulted in a complete thyrotomy, just to the left of midline, with displacement and telescoping of the fractured cartilages explaining the loss of laryngeal prominence. The fracture edges were reduced and re-approximated using two simple interrupted 2-0 PDS sutures. Titanium microplates with self-drilling screws of 3 mm depth were then used to stabilize the reduction with two point fixation. (Figure 5) shows an intra-operative image of the thyroid cartilage fixation. The wound was closed in layers over a penrose drain to prevent further subcutaneous emphysema. The patient was transferred to the intensive care unit intubated and was treated post operatively with IV antibiotics and a proton pump inhibitor. He was extubated in the operating room on post-operative day 4 after ensuring a spontaneous leak on the ventilator. Direct laryngoscopy at the time of extubation revealed a healed mucosal tear at the anterior commissure and normal laryngeal anatomy with a partially resolving left vocal cord haemorrhage. He was discharged home in stable condition and was tolerating a full diet on post-operative day 7. He was last seen in follow up 11 months post-operatively and was doing well with no dysphagia or dysphonia. Examination of the neck revealed good laryngeal contour without noticeable step off or loose hardware (Figure 6 & 7). Flexible fiberoptic laryngoscopy was within normal limits and the patient felt his voice was completely back to baseline; his voice handicap index score was excellent (4/120).


Discussion and Conclusions
This paper illustrated two cases of penetrating laryngeal trauma to zone II that were successfully managed by a conservative surgical approach without tracheotomy. In both cases the airway was managed by awake fiberoptic intubation with the otolaryngology service on standby for possible awake tracheostomy. Rigid esophagoscopy was performed after securing the airway. Neither patient had any evidence of cricotracheal separation. Neck exploration and fracture fixation was performed via extension of the original traumatic wound in both cases. A brief period of endotracheal intubation was used to secure and stent the airway, but no laryngeal keels or formal stents were required.
Using the Schaefer classification, both of these patients fall into the group 3 category and classic management recommendations favour tracheotomy and neck exploration. According to Schaefer’s algorithm published in 1992, awake tracheotomy was recommended unless there was a normal appearing endolarynx with the patient undergoing general anaesthesia for another indication, or the laryngeal injury was occult and not noted until after initial airway management [3]. The concern for avoiding intubation was related to the possibility of avulsion of the endolaryngeal mucosal membrane, creation of a false passage, or disruption of a tenuous airway [5]. However, proponents of intubation such as Gussack et al. believe that emergency tracheotomy may be dangerous as it has the potential to create further damage to surrounding structures [6]. Contemporary reviews of laryngeal trauma management also discuss endotracheal intubation as a viable option when highly experienced personnel are involved [5]. In both of the cases outlined above, awake fiberoptic intubation by an experienced anesthesia team in a controlled environment such as the operating room was successful. This was the preferred route of airway management for these patients after initial clinical assessment and flexible endoscopy seemed favourable for a trial of awake fiberoptic intubation.
Another similarity between the two cases presented is the brief period of endotracheal intubation in the ICU setting used to secure the healing airway. For severe endolaryngeal disruption, unstable fractures, or when a thyrotomy was performed, Schaefer recommended at least ten to fourteen days of formal stenting while Bent et al. recommended at least two to six weeks of formal stenting [3,7]. We found that while the injury essentially caused a paramedian thyrotomy in both cases, the nature of the thyroid cartilage fracture was straightforward, enabling us to use sutures and plates to keep it stabilized. There was also no concern with regards to the patency of the laryngeal lumen. This is in keeping with Leopold et al and Schaefer’s most recent statement with regards to using stents where, “if the laryngeal fractures can be stabilized without an internal lumen keeper, and the endolaryngeal mucosa injuries are minimal, stenting should be avoided” [5,8].
It is important to underline the necessity of assessing concurrent alimentary tract injuries in penetrating laryngeal trauma cases. While the frequency of esophageal injuries with laryngeal trauma is low with studies citing a 4% to 6.3% incidence, the potential consequences of a missed esophageal injury can be catastrophic [9,10]. A 2014 review of aerodigestive tract endoscopy by Soliman and colleagues advocated for rigid endoscopic evaluation of the larynx, hypopharynx, and esophagus in symptomatic patients, when patients are undergoing neck exploration for other injuries, and asymptomatic patients with CT evidence of occult injury [11]. Rigid esophagoscopy was performed in the presented cases to rule out esophageal injury.
In summary, the above highlights two cases of zone II/Schaefer-Fuhrman group 3 penetrating neck trauma using a more conservative surgical approach without tracheotomy or laryngeal stenting. In both cases the airway was secured with awake flexible laryngoscopy followed by a brief period of post-operative intubation in the ICU. Both were managed using a single incision approach, by extending the pre-existing neck wound, and performing an open reduction and fixation of the laryngeal fracture. We were able to achieve favourable voice outcomes and return to normal diet. The above management led to a shorter hospital stay than advocated for in the literature and improved cosmetic outcome without any adverse voice or swallowing outcomes. Given that this is a case series of 2 patients, a major limitation of this study is its generalizability. Caution regarding the findings of the study is warranted, and management of injuries should be tailored depending on the context of each case.
We have reviewed the classic management of penetrating laryngeal trauma as described in the 1990’s and updated in recent years. Essential aspects include expeditious control of the airway, management of laryngeal injuries within 24 hours, evaluation for occult alimentary tract injuries, and maintenance of airway patency in the post-operative period [1-3, 5, 9-11]. However, the method of airway control and stenting remain controversial and can therefore be determined on a case-by-case basis. In these two cases it was possible to avoid multiple incisions and tracheotomy with good voice and swallowing outcomes.
Declarations
Ethics approval and consent to participate
An ethics application and approval were waived by the Providence Health Care/University of British Columbia Research Ethics Board as per the following:
Case Reports
Individual case reports do not meet the definition of research, they are considered to be a medical/educational activity. UBC’s REBs expect that patients will be made aware that the author/investigator plans to create a report about their case which may be published. Case reports for REB purposes are a retrospective analysis of one or two clinical cases. If more than two cases are involved in the analytical activity, the activity will normally constitute “research” and be subject to review. Both patients we contacted by the research coordinator via telephone. A letter was mailed to patient #1 informing them their case will be used for this project. PHC/UBC REB has confirmed if the patient cannot be contacted, a letter may be sent to the home address with the information above. The research coordinator was able to speak to patient #2 and the protocol of the case series was explained in detail. Patient #2 verbally consented they were aware that the information from their case will be included in the case review. A verbal consent form was completed which serves as documentation that the required elements of informed consent had been presented orally to the patient.
Consent for publication
The BioMed Central Consent Form has been signed by the patient.
Availability of data and materials
All data generated or analysed during this study are included in this published article (and its supplementary information files).
Competing interests
The authors declare that they have no competing interests.
Funding
The authors declare that there were no sources of funding for this case series.
Authors’ contributions
DV: Data collection, manuscript writing, revisions to final manuscript
JG: Data collection, manuscript writing, revisions to final manuscript
JL: Data collection, revisions and approval of the final manuscript
Acknowledgements
The authors would like to thank Rochelle Galleto who provided research support and assistance to the project.
Article Info
Article Type
Case ReportArticle History
Received 28 September 2018Accepted 15 October 2018
Published 30 October 2018
Copyright
© 2018 The Authors. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.03.009
Author Info
Corresponding author
Dr. Jane LeaSt. Paul’s Hospital - B.C. Rotary Hearing & Balance Centre, 1081 Burrard St., Providence 2 ENT Clinic, Vancouver, BC, V6Z 1Y6 Canada
Figures & Tables
|
Severity of Injury |
|
|
Group 1 |
Minor endolaryngeal hematomas or lacerations without detectable fractures |
|
Group 2 |
More severe edema, hematoma, minor mucosal disruption without exposed cartilage, or nondisplaced fractures |
|
Group 3 |
Massive edema, large mucosal lacerations, exposed cartilage, displaced fractures, or vocal cord immobility |
|
Group 4 |
Same as group 3, but more severe, with disruption of anterior larynx, unstable fractures, two or more fracture lines, or severe mucosal injuries |
|
Group 5 |
Complete laryngotracheal separation |
|
|
|
Table 1: Schaefer Classification System [3]


References
1. Roon AJ, Christensen N (1979) Evaluation and treatment of penetrating cervical injuries. J Trauma 19: 391-397. [Crossref]
2. Tisherman SA, Bokhari F, Collier B, Cumming J, Ebert J, et al. (2008) Penetrating zone II neck trauma. J Trauma 64: 1392-1405. [Crossref]
3. Schaefer SD (1992) The acute management of external laryngeal trauma: a 27-year experience. Arch Otolaryngol Head Neck Surg 118: 598-604. [Crossref]
4. Thor A, Linder A (2007) Repair of a laryngeal fracture using miniplates. Int J Oral Maxillofac Surg 36: 748-750. [Crossref]
5. Schaefer Sd (2014) Management of acute blunt and penetrating external laryngeal trauma. Laryngoscope 124: 233-44. [Crossref]
6. Gussack GS, Jurkovich J (1988) Treatment dilemmas in laryngotracheal trauma. J Trauma 28: 1439-1444. [Crossref]
7. Bent JP, Silver JR, Porubsky ES (1993) Acute laryngeal trauma: a review of 77 patients. Otolaryngol Head Neck Surg 109: 441-449. [Crossref]
8. Leopold DA (1983) Laryngeal trauma: a historical comparison of treatment methods. Arch Otolaryngol 109: 106-111. [Crossref]
9. Grewal H, Prakashchandra MR, Mukerji S, Ivatury RR (1995) Management of penetrating laryngotracheal injuries. Head Neck 17: 494-502. [Crossref]
10. Demetriades D, Velmahos GG, Asensio JA (2001) Cervical pharyngoesophageal and laryngotracheal injuries. World J Surg 25: 1044-1048. [Crossref]
11. Soliman AM, Ahmad SM, Roy D (2014) The role of aerodigestive tract endoscopy in penetrating neck trauma. Laryngoscope 7: 1-9. [Crossref]
