Journals
A case of Zinner’s syndrome (seminal vesicle cyst with ipsilateral renal agenesis) presenting antenatally
A B S T R A C T
We present a case of a male infant with right renal agenesis associated with an ipsilateral cystic abnormality of the seminal vesicle, also known as Zinner’s syndrome. The infant presented with renal agenesis antenatally at the 20-week gestation anomaly scan, with the cystic seminal vesicle being identified postnatally. We suggest, therefore, that the absent kidney in Zinner’s syndrome is a true congenital abnormality rather than a postnatal involution of a dysplastic kidney as has been previously argued by some [1].
The cystic seminal vesicle in our case was successfully treated with minimally invasive surgery in infancy, thus preventing the various morbidities with which this syndrome more usually presents in adulthood.
K E Y W O R D S
Renal agenesis, seminal vesicle cyst, Zinner’s syndrome
Case
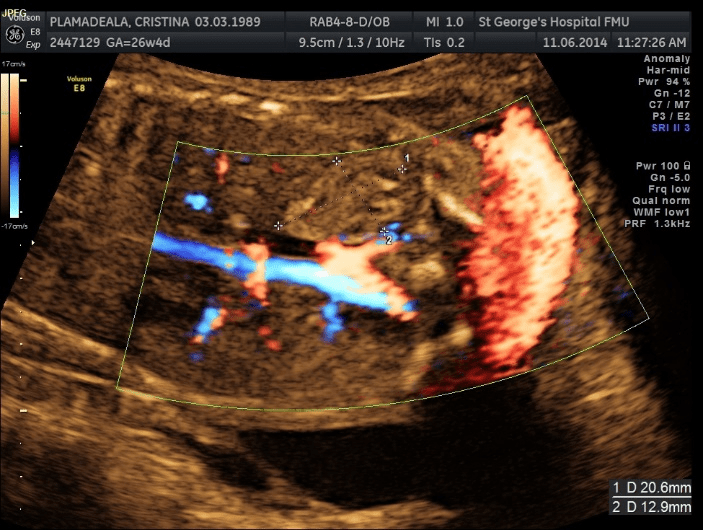
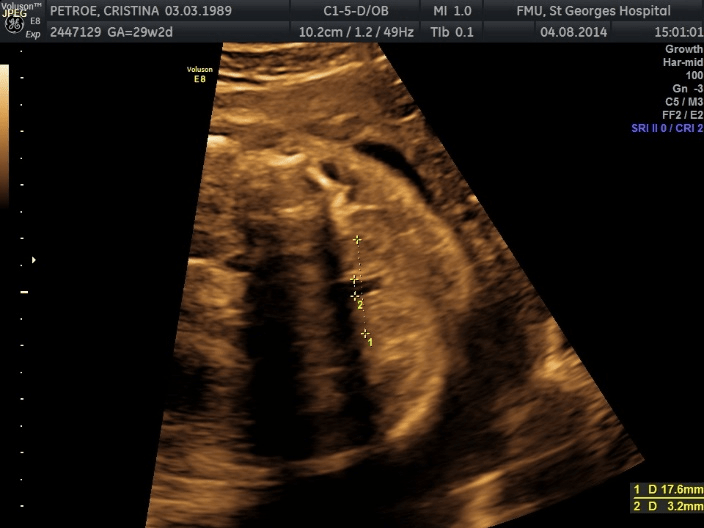
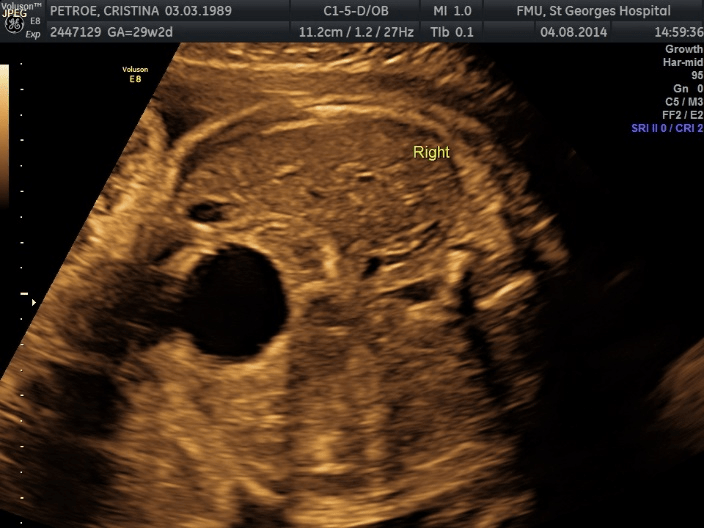
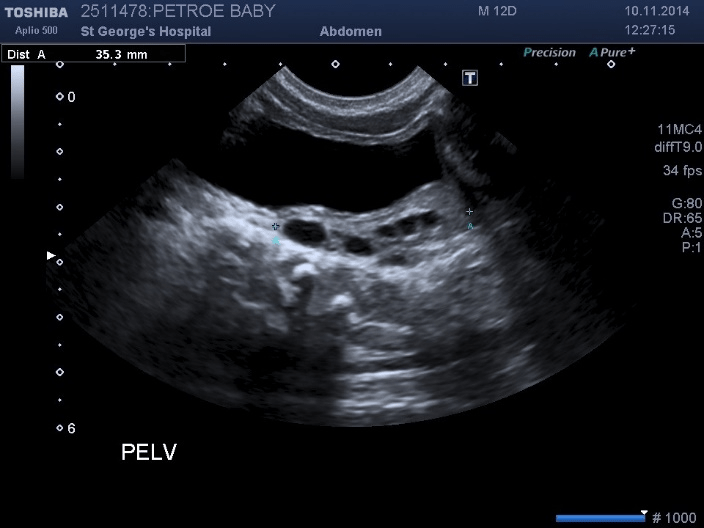
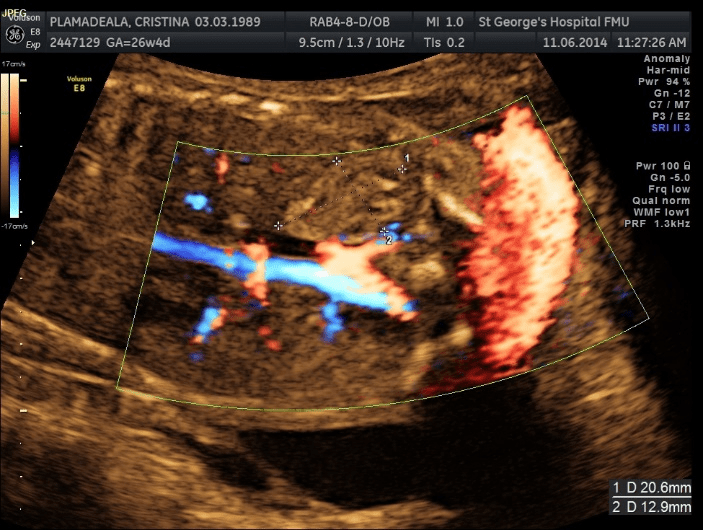
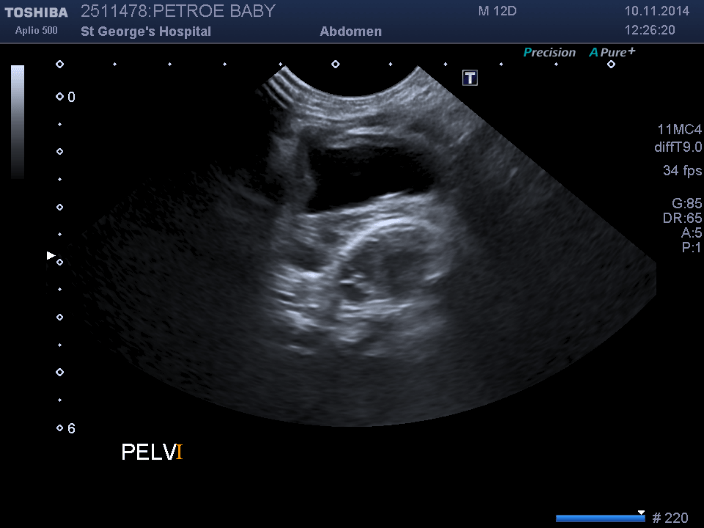
A male infant was referred to us antenatally, with findings at the 20-week gestation anomaly scan of right renal agenesis and a normal solitary left kidney (figures 1, 2, 3). No other abnormalities were identified antenatally. There was a family history of congenital renal abnormalities with the father having a duplex kidney unilaterally. The pregnancy otherwise proceeded uneventfully, and the baby was born at term by forceps delivery.
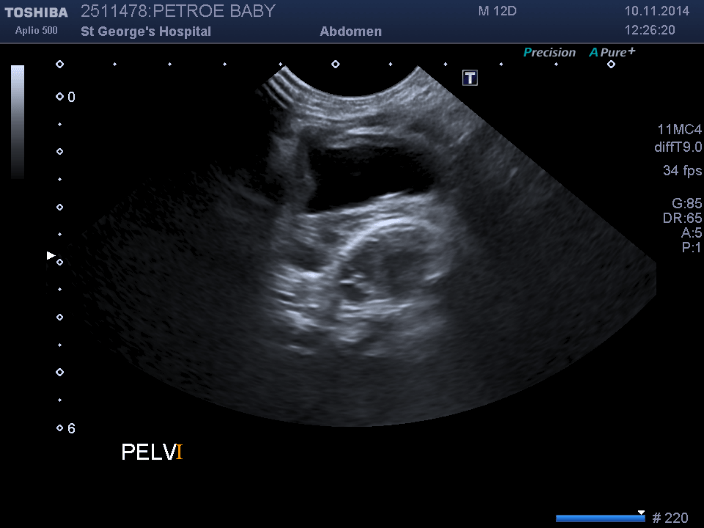
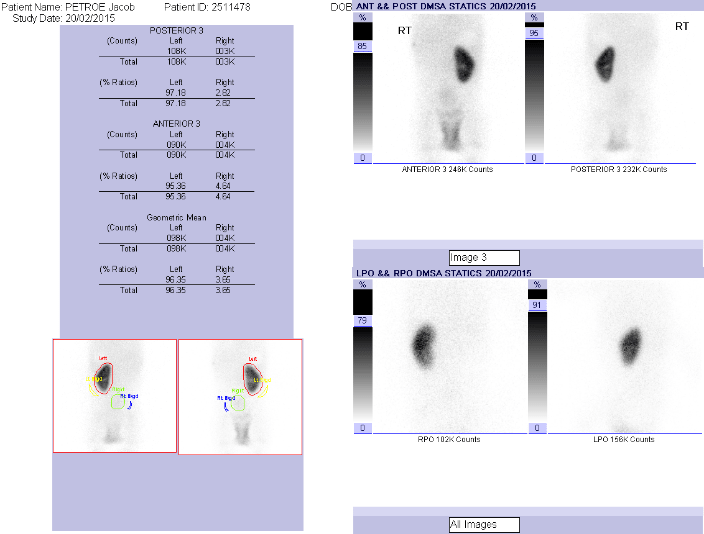
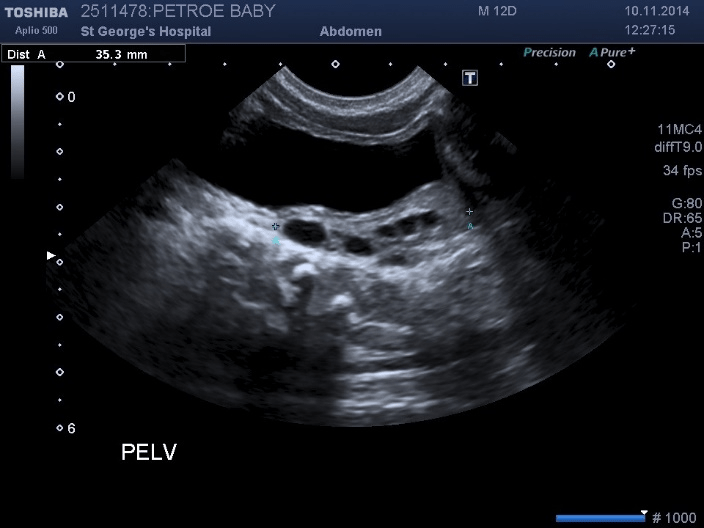
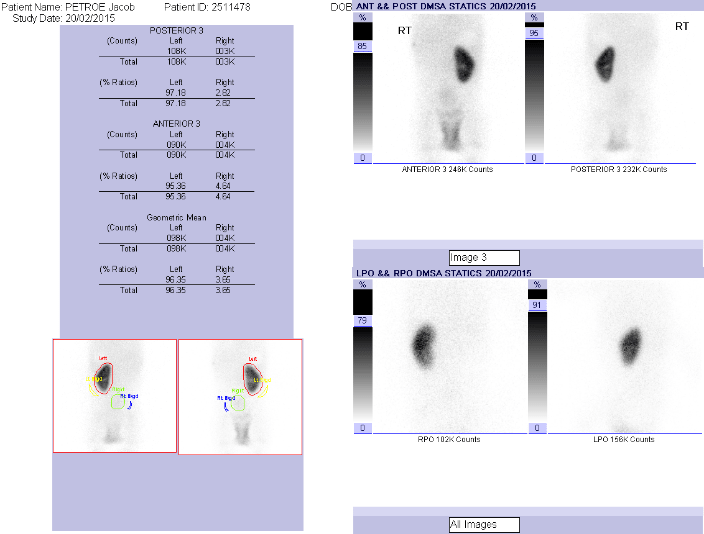
Postnatal scan performed at 11 days of age revealed a normal left kidney, empty right renal bed and a 2.3cm cystic structure in the pelvis posterior to the bladder. [figures 4,5]. This was reported as a possible rudimentary, cystic dysplastic, pelvic right kidney. A DMSA scan performed at 3 months of age confirmed a solitary functioning left kidney (figure 6).
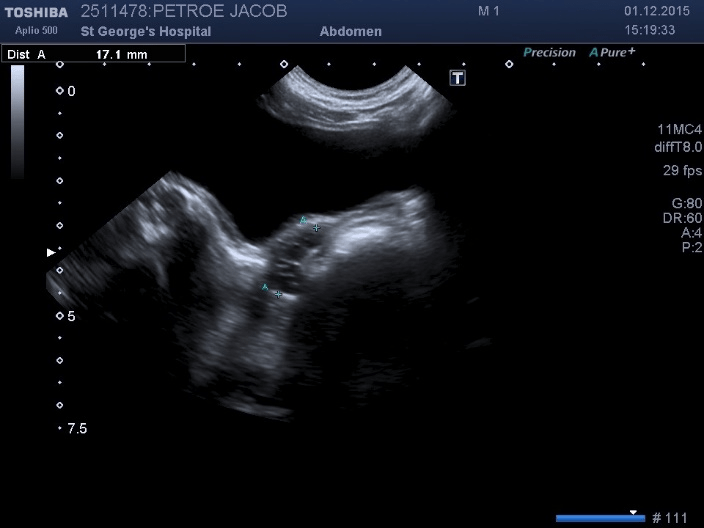
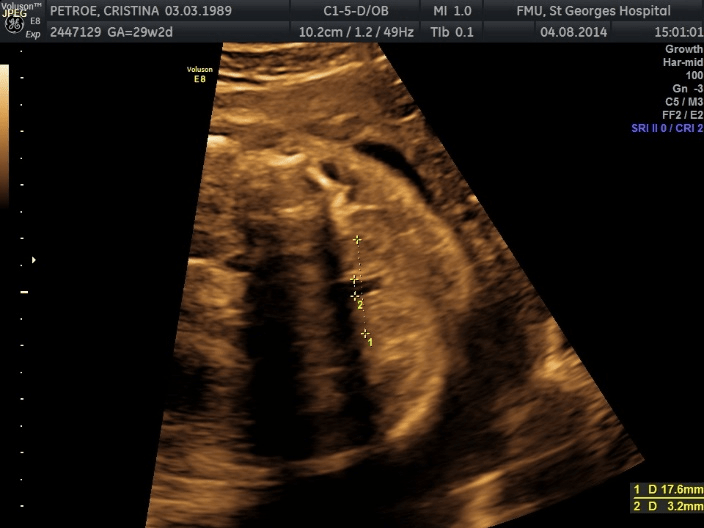
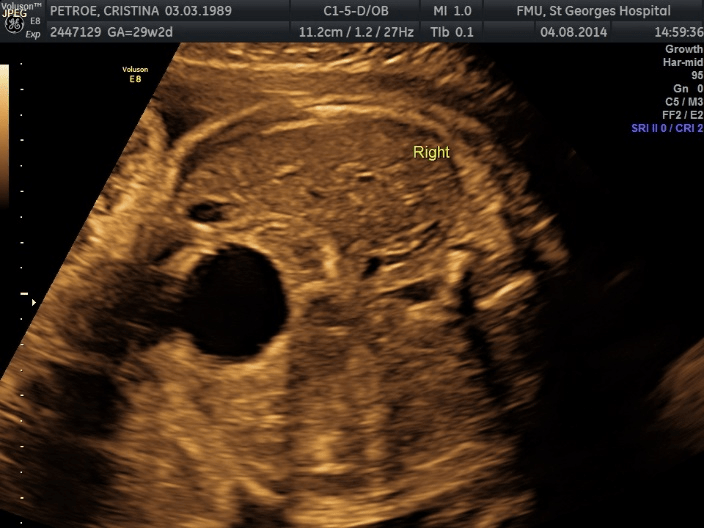
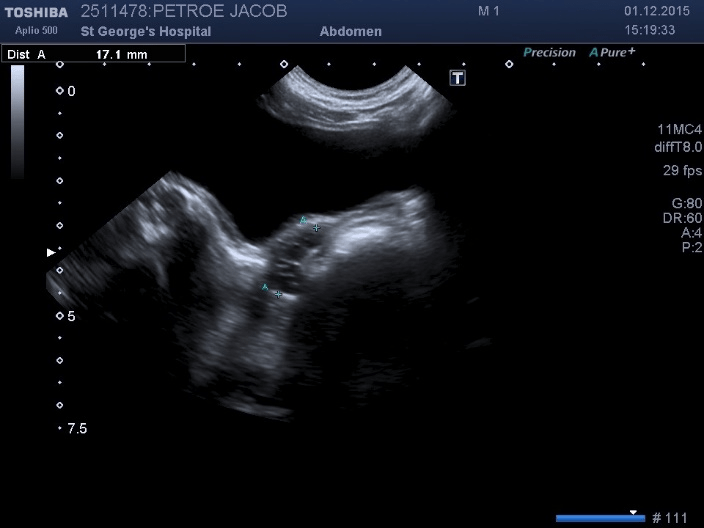
As the infant was asymptomatic, and in accordance with the parents’ wishes, he was initially treated conservatively with ultrasound surveillance. A follow up ultrasound scan at a year of age showed that the cystic structure had decreased in size to 17mm and contained multiple small cysts, with the largest being 3mm. This cystic structure was situated posteriorly to the bladder, on the right side (figure 7). The left kidney showed appropriate compensatory hypertrophy. The child remained asymptomatic The imaging was still thought to represent a dysplastic right pelvic kidney and laparoscopic excision was planned.
Surgery was performed at 18 months of age. A 5mm 30-degree scope and two 5mm instrument ports were used. At laparoscopy, the right vas was found to be abnormally tortuous, ending in a cystic structure which lay posteriorly and to the right of the bladder. There was an atretic ureteric remnant seen to be entering the cystic mass. The proximal end of this was blind ending. The right internal ring was closed. The right kidney was completely absent. The right testis on palpation was descended but with a palpably separate epididymis. There was a normal left vas and closed left internal ring. The pelvic cystic structure was excised, along with the abnormal appearing vas, which was not possible to preserve as it was entering the cystic structure. Excision was with hook diathermy and removal via the umbilical port.
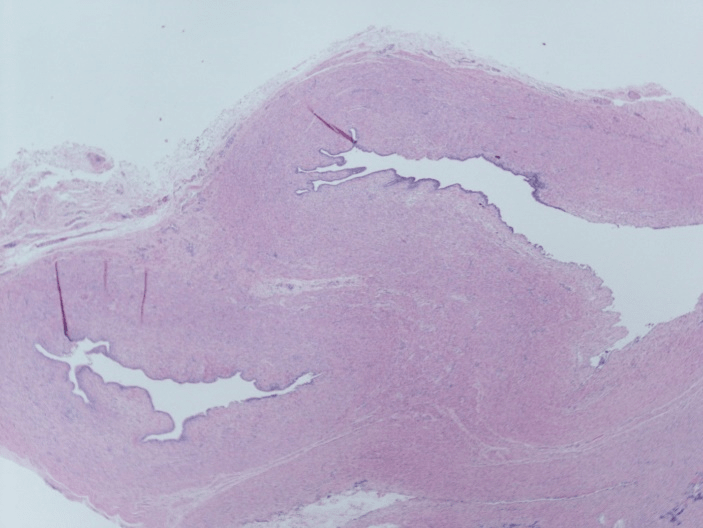
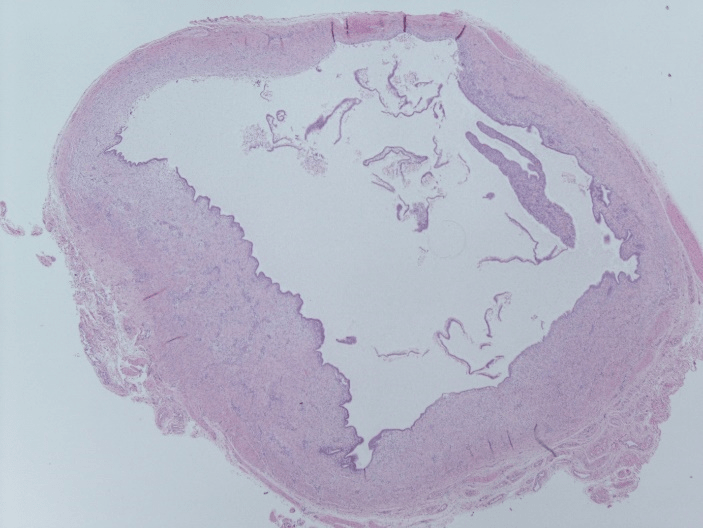
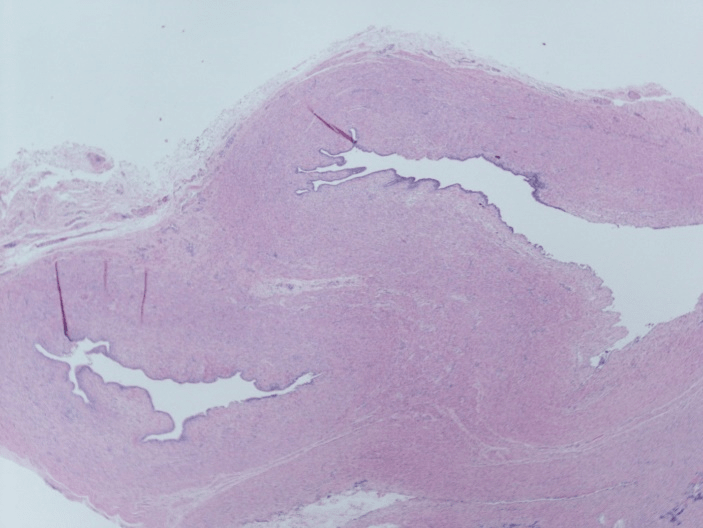
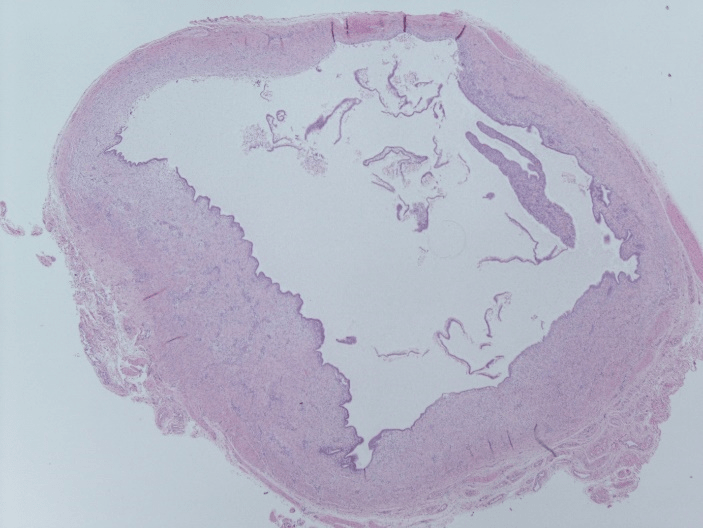
The child made an uneventful recovery and went home the following day. There were no post-operative complications. Histopathology results showed cystic dilatation of a structurally abnormal seminal vesicle, lined with columnar epithelium (figure 8). The vas also appeared dilated and tortuous (figure 9). No renal elements were identified.
There has been no recurrence of the cysts on follow up scans at 1 year post operatively. Scan of the scrotal contents showed normal testes bilaterally.
Discussion
Seminal vesicle cysts are incredibly rare with an incidence of 0.0005% of the population, of which around two thirds are associated with ipsilateral renal agenesis. Contralateral renal agenesis has also been reported as has renal dysplasia rather than agenesis [2-4].
The first description of seminal vesicle cysts is generally accredited to Smith in 1872, with Zinner first describing the association with ipsilateral renal agenesis, resulting in the eponym of Zinner’s syndrome [5, 6]. Both left and right sides are equally affected by this syndrome, and whilst most reports concern white men it has also been reported in Afro-caribbean men [7].
There are now over 200 cases reported in the literature, with the majority of these presenting in adults. Our case represents one of very few reports of this abnormality being discovered antenatally and so treated in infancy before symptom onset.
The association between renal and seminal vesical congenital abnormalities can be explained embryologically by the relative proximity of the origin of the ureter and seminal vesicle during fetal development. Zinner’s syndrome probably results from an abnormality in the relative position of the ureteric bud and the mesonephric duct during the 4th week of gestation. The seminal vesicle buds off the mesonephric duct in the 13th week of gestation. If the ureteric bud develops too cranially to the mesonephric duct it may develop an opening into the seminal vesicle instead of the bladder. This impairs the normal development of the ureter which in turn prevents the stimulation of the development of the metanephros and hence kidney on that side. Our findings at laparoscopy of an absent kidney and remnant atretic ureter entering the cystic seminal vesicle support this hypothesis.
There are reports of seminal vesicle cysts in infancy being associated with dysplastic kidneys rather than renal agenesis [1, 4]. Indeed Shukfeh, who reported 9 paediatric cases of seminal vesicle cysts associated with renal dysplasia, postulated that the renal agenesis of Zinner’s syndrome described in adults represented an involuted dysplastic kidney [1]. However, our findings of renal agenesis being detected antenatally would support the hypothesis that the absent ipsilateral kidney of Zinner’s syndrome is a true congenital event.
Symptomatic presentation of seminal vesicle cysts is usually in the second to third decade of life, thought to be related to the time of maximal sexual activity. Symptoms reported vary between pain (buttock, inguino-scrotal, low abdominal, perineal, testicular or ejaculatory pain, or dysuria or pain on defecation), blood (haematuria, haemospermia), frequency, urgency, obstructive symptoms (straining, urinary retention, difficulty defecating), recurrent epididymitis, UTIs, chronic prostatitis, a palpable mass or infertility.
The cysts are usually 5cm or less in diameter, but giant cysts of greater than 12cm in diameter have been described. These can cause symptoms of bladder or rectal obstruction [2 8, 9]. Infertility is one of the presenting symptoms of Zinners syndrome in adulthood. Zinners syndrome has been found to be associated with a decreased sperm count, asthenospermia, reduced semen volume and reduced seminal fructose level [10]. As this syndrome is unilateral, and therefore there should be a normally functioning contralateral seminal vesicle, the exact reasons for the reduced fertility are unclear. Some reports have shown that infertility was due to the seminal vesicle cysts obstructing both seminal ducts, whilst others report partial obstruction causing subfertility [11, 12].
There are reports of an improvement in fertility following surgical resection of the seminal vesicle cysts, with Pace reporting 1 out of 7 of their cases of Zinners achieving paternity without aid following cyst resection [12]. Others, however have reported no improvement in semen analysis following resection [10]. Although usually asymptomatic in childhood, seminal vesicle cysts can present in infancy and childhood with recurrent, recalcitrant epididymo-orchitis [13-15].
In the light of this catalogue of morbidities, prophylactic excision of antenatally diagnosed seminal vesicle cysts would seem prudent once the child is big enough for easy laparoscopic excision.
There are a few reports of seminal vesicle cysts being diagnosed and treated in infancy, but few reports describe antenatal detection of seminal vesicle cysts, with or without renal agenesis [1, 4, 16, 17]. Steffans reports a case of a 10-month-old in whom a 20mm cyst detected antenatally was, as in our case, thought to represent an MCDK [4]. Postnatally this was found to be a seminal vesicle cyst connected to an ectopic ureter draining a non-functioning dysplastic kidney. Valla et al is the only other report of antenatal detection of a pelvic cystic mass with ipsilateral renal agenesis as described in Zinner’s syndrome [17]. Similarly, to our case, this was initially managed conservatively, then removed laparoscopically at the age of 15 months as the cyst was found to be increasing in size, although in this case 4 rather than 3 ports were used for the surgery.
Our case was detected on antenatal then postnatal ultrasound scanning, with the final diagnosis only being made on histology following surgical excision. More usually, with symptomatic presentation in the adult period, other modalities are used. In adults, excretory urography, abdominal or transrectal ultrasound (TRUS), cross-sectional imaging and vasography have all been used. TRUS appears to be a reliable method of diagnosis in adults [18, 19]. At cystoscopy an absent hemi-trigone is seen and sometimes the indentation of the cyst into the bladder. In adults, cross-sectional imaging has increased the detection of this abnormality. With the steady improvement in antenatal scanning, it is likely that more cases will be detected antenatally giving the opportunity to intervene before the cysts become symptomatic.
Asymptomatic cases in adulthood have been managed conservatively [20]. When symptomatic, cysts have been treated either by aspiration, deroofing, or excision. Aspiration of the cyst by various approaches (tranurethrally, transabdominally, transrectally) has been described but recurrence is most commonly reported following this approach, although it has been used successfully as the sole treatment [18, 19, 21, 22]. Success with transurethral deroofing of the cyst has also been reported [21].
In the past the majority were treated with open surgical excision. A broad mix of approaches including transperitoneal, transvesical, retroperitoneal and posterior transcoccygeal have been described. Whichever the approach, open surgery was a major undertaking, associated with high morbidity [23]. The advent of laparoscopy was a turning point in the management of seminal vesicle cysts, although the first reports of this method used 5 ports and had an operative time of around 3 hours, reducing to 4 ports in 2002 [7, 24-26].
Laparoscopic removal of these cysts is now the treatment modality of choice, including in childhood and infancy, still with 4 ports [13, 16, 17, 22, 27].
More recently, robotic-assisted removal has been reported, in a 16-year-old boy, with operative time and hospital stay comparable to the laparoscopic method with described advantages being the greater precision and better view of the anatomy afforded by the 3D view and magnification [28, 29].
Valla et al removed the cyst whilst leaving the ipsilateral vas deferential intact, achieved by leaving a thin strip of the cyst on the vas. This was not possible in our case as the vas was also tortuous and abnormal [16]. Basillote described a technique of filling the cyst with indigo carmine, by cannulating the ejaculatory duct cystoscopically just before excision, to aid the identification of the cyst and thus speed and ease of cyst removal [13]. Vasoligation alone has been successful in treating the seminal vesicle cyst of an infant of 4 months with presenting with recurrent epididymo-orchitis [15].
As typified in our case, histologically the cysts are usually found to be lined with columnar epithelium, typical of seminal vesicles. There have been reports in adults of primary seminal vesicle adenocarcinoma in the abnormally formed seminal vesicles found in Zinner’s syndrome [30, 31]. There is also a report of Zinner’s syndrome in conjunction with papillary carcinoma of the bladder in a 37-year-old with no risk factors for bladder cancer, and it was postulated that irritation of the bladder by the cyst could be a contributory factor in the pathogenesis of the papillary tumour [32].
In one case in a 6-month-old the cyst was found to contain squamous metaplasia in the cyst epithelium, although in this case the cyst was not associated with renal agenesis [15]. Although in our case no concerning histological features were found, the above reports strengthen the case for prophylactic laparoscopic excision.
Conclusion
Zinner’s syndrome appears to be a true congenital abnormality, which can be detected antenatally. It is then feasible and relatively simple to excise the abnormal cystic seminal vesicle minimally invasively, using 3 ports, in infancy or early childhood, without a lengthy hospital stay. In the light of the multiple morbidities that this condition can cause in early adulthood or earlier, along with the risk of metaplasia and carcinoma, we would advocate prophylactic excision.
Article Info
Article Type
Case ReportArticle History
Received 18 July, 2018Accepted 9 August, 2018
Published 28 August 2018
Copyright
© 2018 F. Murphy. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.10.31487/j.SCR.2018.02.008
Author Info
Corresponding author
F. Murphy2 St.George’s Hospital, London, UK
Figures & Tables
References
1. Schukfeh N, Kuebler JF, Schirg E, Petersen C, Ure BM, et al. (2009) Dysplastic kidney and not renal agenesis is the commonly associated anomaly in infants with seminal vesicle cyst. BJU Int 103: 816-819. [Crossref]
2. El-Assmy A, Abou-El-Ghar ME (2012) Giant Seminal Vesicle Cyst Causing Ipsilatera Hydronephrosis with Contralateral Renal Agenesis. Urology 79: e17-e18. [Crossref]
3. Kosan M1, Tul M, Inal G, Ugurlu O, Adsan O (2006) A large seminal vesicle cyst with contralateral renal agenesis. Int Urol Nephrol 38: 591-592. [Crossref]
4. Steffens J, Oberschulte-Beckmann D, Siller V, Röttger P, Polsky MS (2000) Ectopic refluxing ureter entering a seminal vesicle cyst associated with ipsilateral renal dysplasia. World J Urol 18: 232-234. [Crossref]
5. Smith NR (1872) Hydrocele of the seminal vesicle. Lancet 2: 558.
6. Zinner A (1914) Ein Fall von intravesikaler Samenblasezyste. Wien Med Wochenschr 64: 605.
7. Cherullo EE, Meraney AM, Bernstein LH, Einstein DM, Thomas AJ, et al. (2002) Laparoscopic Management of Congenital Seminal Vesicle Cysts
Associated with Ipsilateral Renal Agenesis. J Urol 167: 1263-1267. [Crossref]
8. Zaontz M, Kass E (1987) Ectopic Ureter opening into seminal vesicle cyst associated with ipsilateral renal agenesis. Urology 29: 523-525. [Crossref]
9. Kao CC, Wu CJ, Sun GH, Yu DS, Chen HI, et al. (2010) Congenital Seminal Vesicle Cyst Associated with Ipsilateral Renal Agenesis Mimicking Bladder Outlet Obstruction: A Case Report and Review of the Literature. Kaohsiung J Med Sci 26: 30-34. [Crossref]
10. Manousakas T, Kyriakou G, Serafetinides E, Giannopoulou M, Kyroudi A, et al. (2002) Partial vesiculectomy in and infertile man with seminal vesicle cyst, ipsilateral renal agensis and cryptorchidism. Urology 59: 602. [Crossref]
11. Carbone A1, Palleschi G, Tomiselli G, Inghilleri M, Rago R, et al. (2007) Renal Aplastic Dysplasia and Ipsilateral Ectopic Ureter Obstructin the Seminal Via: A Possible Cause of Male Infertility. Eur Urol 52: 268-272. [Crossref]
12. Pace G, Galatioto GP, Gualà L, Ranieri G, Vicentini C (2008) Ejaculatory duct obstruction caused by a right giant seminal vesicle with an ipsilateral upper urinary tract agenesia: an embryologic malformation. Fertil Steril 89: 390-393. [Crossref]
13. Basillote JB, Shanberg AM, Woo D, Perer E, Rajpoot D, et al. (2004) Laparoscopic excision of a seminla vesicle cyst in a child. J Urol 369-371. [Crossref]
14. Pimpalwar A, Chowdhary S, Huskisson J, Corkery JJ (2002) Cysts of the Ejaculatory System - A Treatable Cause of Recurrent Epididymo-orchitis in Children. Eur J Pediatr Surg 12: 281-285. [Crossref]
15. Yanai T, Okazaki T, Yamataka A, Urao M, Kobayashi H, et al. (2005) Cysts of the ejaculatory system: a report of two cases. Pediatr Surg Int 21: 939-942. [Crossref]
16. Ikari O, Castilho R, D'Ancona C, Netto N (1999) Laparoscopic Excision of Seminal Vesicle Cysts. J Urol 162: 498-499.
17. Valla JS, Carfagna L, Tursini S, Mohaidi MA, Bosson N, et al. (2003) Congenital seminal vesicle cyst: prenatal diagnosis and postnatal laparoscopic excision with an attempt to preserve fertility. BJU Int 91: 891-892. [Crossref]
18. Adeyoju AB, Taylor P, Payne SR (2001) Congenital seminal vesicle cysts: an unusual but treatable cause of lower uriinary tract / genital symptoms. BJU Int 87: 901-902. [Crossref]
19. Narlawar R, Hanchate V, Raut A, Hira P, Nagar A, et al. (2003) Renal Agenesis and Seminal Vesicle Cyst. J Ultrasound Med 22: 225-228.
20. Cihan A, Cimen S, Secil M, Kefi A, Aslan G (2006) Congenital seminal vesicle cyst accompanying ipsilateral renal agenesis and rudimentary ureter. Int Urol Nephrol 38: 133-135. [Crossref]
21. Gözen AS, Alagöl B (2006). Endoscopic Management of Seminal-Vesical Cyst with Right Renal Agenesis Causing Acute Urinary Retention: Case Report. J Endourol 20: 919-922. [Crossref]
22. Liatsikos E, Lee B, Filos K, Barbalias G (2004) Congenital Seminal Vesicle Cyst and Coexisting Renal Agensis: Laparoscopic Approach. Urology 63: 584.e12-584.e14.
23. Denes F, Montellato N, Lopes R, Filho C, Cabral A (1986) Seminal Vesicle Cyst and Ipsilateral renal agenesis. Urology 28: 313-315.
24. Carmignani G, Gallucci M, Puppo P, De Stefani S, Simonato A, et al. (1995) Video Laparoscopic Excision of a Seminal Vesicle Cyst associated with Ipsilateral Renal Agenesis. J Urol 153: 437-439. [Crossref]
25. McDougall EM, Afane JS, Dunn MD, Shalhav AL, Clayman RV (2001) Laparoscopic Management of Retrovesical Cystic Disease: Washington University Experience and Review of the Literature. J Endourol 15: 815-819. [Crossref]
26. Buogo G, Rodrigues H, Rodrigues P (2002) Laparoscopic Removal of Seminal Vesicle Cyst with Ectopic Ureteral Insertion and Renal Remnant. International Brazilian Journal of Urology 28: 335-337.
27. Han P, Dong Q, Shi M, Yang YR, Wei Q (2007) Seminal Vesicle Cyst and Ipsilateral Renal Agenesis: Laparoscopic Approach. Arch Androl 53: 285-288. [Crossref]
28. Moore CD, Erhard MJ, Dahm P (2007) Robot-Assisted Excision of Seminal Vesicle Cyst Associated with Ipsilateral Renal Agenesis. J Endourol 21: 776-779. [Crossref]
29. Selli C, Cavalleri S, De Maria M, Iafrate M, Giannarini G (2008) Robot-Assisted Removal of a Large Seminal Vesicle Cyst with Ipslateral Renal Agenesis Associated with an Ectopic Ureter and a Mullerian Cyst of the Vas Deferens. Urology 71: 1226.e5-1226.e7. [Crossref]
30. Lee BH, Seo JW, Han YH, Kim YH, Cha SJ (2007) Primary Mucinous Adenocarcinoma of a Seminal Vesicle Cyst Associated with Ectopic Ureter and Ipsilateral Renal Agenesis: a Case Report. Korean J Radiol 8: 258-261. [Crossref]
31. Okada Y, Tanaka H, Takeuchi H, Yoshida O (1992) Papillary adenocarcinoma in a seminal vesicle cyst associated with ipsilateral renal agenesis: a case report. J Urol 148: 1543-1545. [Crossref]
32. Gorrea M, Lorente R, Roel J (2001) Seminal vesicle cyst associated with ipsilateral renal agenesis and papillary carcinoma of the bladder. Eur Radiol 11: 2500-2503. [Crossref]
