A Case of Scheuermann’s Disease Co-Occurrence with Idiopathic Scoliosis and Intradural-Extramedullary Epidermoid Cyst: The First Case Report in Literature
A B S T R A C T
Background and importance: Scheuermann’s disease (SD), intradural-extramedullary epidermoid cysts and idiopathic scoliosis (IS) are all rare conditions. The co-occurrence of the three condition on one case has not been reported in literature before. We describe an extremely rare case of SD co-occurrence with IS and intradural-extramedullary epidermoid cyst, which is the first in the literature.
Clinical presentation: A 13-year old boy and his parents presented at Honghui Hospital complaining of progressive hyperkyphosis for 5 years and back pain for 2 months. Thorough medical examination and radiology confirmed the diagnosis of SD kyphosis, IS, and intradural-extramedullary epidermoid cyst. Medical panel with spine surgeons, oncologists, neurosurgeons, histopathologists and radiologists were consulted. Tumor excise, kyphosis recorrection and spine reconstruction surgery was conducted. Postoperative histological examination detected desquamation of keratin from the epithelial lining and stratified squamous epithelium without skin adnexa. The boy was ambulant 2 days postoperative with walking aids.
Conclusion: This is the first case report of Scheuermann’s disease (SD) co-occurrence with idiopathic scoliosis (IS) and intradural-extramedullary epidermoid cyst. The co-occurrence of intradural epidermoid cyst, SD and IS might not be a coincidence, indicating a kind of genetic etiology need to be illuminated.
Keywords
Scheuermann’s disease (SD), epidermoid cysts, idiopathic scoliosis (IS), extramedullary, intradural
Background and Importance
Scheuermann’s disease (SD) or juvenile kyphosis itself is a rare situation with a prevalence of 0.4%-8.0% [1]. It is characterized with progressive, structural thoracic or thoracolumbar hyperkyphosis associated with back pain in adolescents. The typical radiology performance is vertebral body wedging, vertebral endplate irregularity, diminished anterior vertebral growth, Schmorl’s nodes, narrowing of the intervertebral disk spaces, and premature disk degeneration. It’s co-occurrence with IS is seldom reported previously [2]. Epidermoid cysts of the spinal cord are also unusual lesions which represent less than 1% of all intraspinal tumors [3-5]. The co-occurrence of the three rare conditions, Scheuermann’s disease (SD), idiopathic scoliosis (IS), and intradural-extramedullary epidermoid cyst, has not been reported in literature before. We describe an extremely rare case of SD co-occurrence with IS and intradural-extramedullary epidermoid cyst, which is the first in the literature.
Clinical Presentation
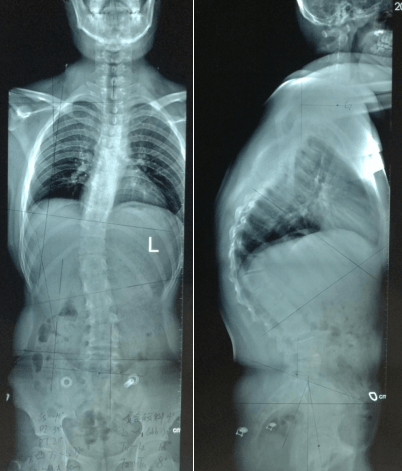
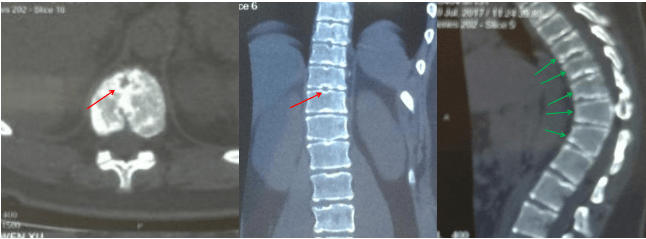
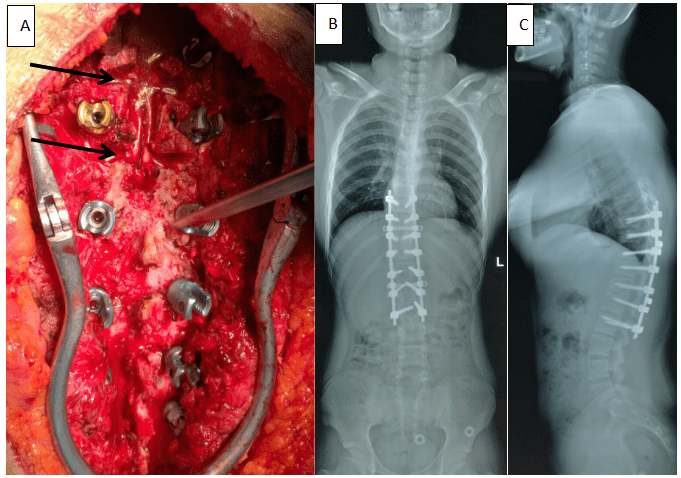
A 13-year old boy and his parents presented at the authors’ hospital complaining of progressive hyperkyphosis for 5 years and back pain for 2 months. He had no complain of symptoms such as muscle weakness, abnormal sensation, bowel or urinary retention. He had no history of relevant trauma or intradural puncture. His physical examination was negative, with normal sensation and motor. Normal muscle tone and reflexes. Hematological and serum chemistry tests were negative. Routine lateral and A-P X-ray (with the whole spine included) (Figure 1) showed diminished anterior vertebral growth from T9 to L1, hyperkyphosis (C7-SVA 6cm, T7/L2 73o) and scoliosis (C7-CSVL 1.8cm. Cobb’s angle: T2/T11 8o, T11/L2 18o, L2/S1 30o) and Risser’s Sign 4. CT scans showed vertebral endplate irregularity and sclerosis, diminished anterior vertebral growth, Schmorl’s nodes, narrowing of the intervertebral disk spaces (Figure 2). Whole spine MRI was examined to illustrate any neuromuscular abnormalities. And a 6cm long T1WI hypointense, T2WI hyperintense signal was found intradural-extramedullary, just below the conus medullaris, at T12/L1 level (Figure 3). Before surgery, a medical panel with spine surgeons, oncologists, neurosurgeons, histopathologists and radiologists were consulted. Tumor excise and kyphosis recorrection surgery was arranged. T8~L2 pedical screws placed after bony structures exposed. Total microsurgical excision of the lesion achieved with the help of neuromonitoring. T12/L1 laminotomies performed using a piezoelectric ultrasonic osteotome. After dural opening, the whitish cyst capsule came into sight and opened, the dense pearly content curetted out (Figure 4). And then, with meticulous protection of the cauda equina fibers and conus medullaris, the cyst capsule was excised completely. Watertight closure of dura mater with dura gel. Several continuous Ponte Osteotomy was performed to correct the hyperkyphosis, allograft and rod-screws fixed for spine reconstruction (Figure 5). Postoperative histological examination detected desquamation of keratin from the epithelial lining and stratified squamous epithelium without skin adnexa (Figure 6). The boy was ambulant 2 days postoperative with walking aids. He was discharged 1 week later.
Figure 1: Routine lateral and A-P X-ray showed diminished anterior vertebral growth from T9 to L1. Hyperkyphosis (C7-SVA 6cm, T7/L2 73o) and scoliosis (C7-CSVL 1.8cm, Cobb’s angle: T2/T11 8o, T11/L2 18o, L2/S1 30o) .
Figure 2: CT scans showed vertebral endplate irregularity and sclerosis, diminished anterior vertebral growth (green arrows), Schmorl’s nodes (red arrows), narrowing of the intervertebral disk spaces .
Figure 3: A 6cm long intradural-extramedullary lesion was detected just below the conus medullaris, at T12/L1 level. T1WI hypointense (A), T2WI hyperintense (B) signal. Cervical and thoracic MRI (C & D) exclude other abnormalities.
Figure 4: The dense pearly content of the tumor.
Figure 5: Continuous Ponte Osteotomy (black arrows) was performed to correct hyperkyphosis, pedicle screws placed for spine reconstruction (A). Postoperative A-P and lateral X-ray show hyperkyphosis corrected (T7/L2 kyphosis angle dropped to 25o from 73o) (B,C).
Figure 6: Postoperative histological examination detected desquamation of keratin from the epithelial lining and stratified squamous epithelium without skin adnexa.
Discussion
Epidermoid cysts of the spinal cord are rare benign tumours which may be congenital or acquired. Malignant progression is extremely rare. Because of its typically slow grown character, the symptoms are usually occult and progressively, especially in young children.The most frequent symptoms first presented at a clinic is progressing deteriorating sensation, paraparesis,even urinary retention. The situation in this boy mainly complaining of hyperkyphosis and sometimes back pain without nerve symptoms is are. Routine X-ray of epidermoid cysts are usually normal if not co-occurrence with IS, SD, et al., both of which are of rare condition [6]. This is the first case report of Scheuermann’s disease (SD) co-occurrence with idiopathic scoliosis (IS) and intradural-extramedullary epidermoid cyst. In consensus, MRI is considered the best investigation tool to diagnose spinal epidermoid cysts, with T1-WI usually show hypointensity or isointensity signal, and T2-WI show hyperintensity signal [7]. MRI diffusion-weighted imaging (DWI) and fluid attenuated inversion recovery (FLAIR) sequence are also very help in the diagnosis of epidermoid cysts. DWI clearly shows homogeneous hyperintensity in epidermoid cysts. Because the epidermoid cysts do not contain free water,slower diffusion of cysts leads to hyperintensity on DWI7 . However, the intensity of DWI in neurinomas, meningiomas, and arachnoid cysts is not as high as that in epidermoid cysts [8]. Spinal arachnoid cysts do not show restriction on DWI, and their signal is often suppressed by fluid attenuated inversion recovery; spinal dermoid cysts usually contain fatty elements [9, 10]. Whole spine MRI should be done to rule out syringohydromyelia and other abnormalities, which is negative in this case except the epidermoid cyst (Figure 2). CT scans showed vertebral endplate irregularity and sclerosis, diminished anterior vertebral growth, Schmorl’s nodes, narrowing of the intervertebral disk spaces confirmed the diagnosis of SD (Figure 3) can be done after MRI at suspicious sites to rule out spina bifida and other bony abnormalities.
Surgical resection is the preferred treatment for epidermoid cysts. Gross total resection is preferred. However, when total resection is not possible in caution of neuro protection, partial debulking resections have demonstrated satisfactory long-term outcomes, only sometimes recurrence is quite annoying. One case had been reported 8 interventions in 30 years and finally successfully treated with radiotherapy [11]. In this case, total resection including the content and cyst are excised. And several continuous Ponte Osteotomy was performed to correct the SD hyperkyphosis. The extremely rare co-occurrenced IS is not treated surgically. Neither of the three conditions’ own etiology is not clear. The cause of epidermoid cysts is believed to be the introduction of ectoderm cells arising in early fetal life between 3 and 5 weeks [12]. In 2017, Dai et al. reported a series cases of familial lumbar scheuermann disease with idiopathic scoliosis in China, which might indicate the genetic etiology of Scheuermann disease with IS.2 In this case, the co-occurrence of intradural epidermoid cyst, SD and IS might not be a coincidence, indicating a kind of genetic etiology need to be illuminated.
Conclusion
This is the first case report of Scheuermann’s disease (SD) co-occurrence with idiopathic scoliosis (IS) and intradural-extramedullary epidermoid cyst. Gross total resection of the epidermoid cyst is advised if possible. Whether the co-occurrenced SD and IS needs surgical treatment should be decided by a medical panel with at least one senior spine surgeon, one senior oncologist, and one senior neurosurgeon. The co-occurrence of intradural epidermoid cyst, SD and IS might not be a coincidence, indicating a kind of genetic etiology need to be illuminated.
Consent
Informed consent was obtained from the parents and patient to publication of this study and the accompanying images.
Conflicts of Interest
None.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 21, Aug 2019Accepted: Mon 09, Sep 2019
Published: Tue 17, Sep 2019
Copyright
© 2023 Jinwen Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2019.04.12
Author Info
Dingjun Hao Jinwen Zhu Xiaodong Wang Zhen Chang
Corresponding Author
Jinwen ZhuHonghui Hospital, Xi'an Jiaotong University College of Medicine, Xi'an, China,710054
Figures & Tables



References
- Damborg F, Engell V, Andersen M, Kyvik KO, Thomsen K (2006) Prevalence, concordance, and heritability of Scheuermann kyphosis based on a study of twins. J Bone Joint Surg Am 88: 2133-2136. [Crossref]
- Dai Y, Li Y, Li P, Li L, Tu Z et al. (2017) Familial lumbar Scheuermann disease with idiopathic scoliosis in China. Medicine (Baltimore) 96: e7100. [Crossref]
- Deogaonkar M, Goel A, Pandya SK (1995) Thoracic intradural anterior epidermoid manifesting as sudden onset of paraplegia-case report. Neurol Med Chir 35: 678-679. [Crossref]
- Scarrow AM, Levy EI, Gerszten PC, Kulich SM, Chu CT et al. (2001) Epidermoid cyst of the thoracic spine: case history. Clin Neurol Neurosurg 103: 220-222. [Crossref]
- Barbagallo GMV, Maione M, Raudino G, Certo F (2017) Thoracic intradural-extramedullary epidermoid tumor: the relevance for resection of classic subarachnoid space microsurgical anatomy in modern spinal surgery. Technical note and review of the literature. World Neurosurg 108: 54-61. [Crossref]
- Yin H, Zhang D, Wu Z, Zhou W, Xiao J (2014) Surgery and outcomes of six patients with intradural epidermoid cysts in the lumbar spine. World J Surg Oncol 12: 50. [Crossref]
- Fazio MG, Kil AM, Rooks VJ, Biega TJ (2013) Diffusion-weighted magnetic resonance imaging of an intramedullary epidermoid cyst with dorsal dermal sinus tract in a toddler. Case Rep Radiol 2013: 878713. [Crossref]
- Kukreja K, Manzano G, Ragheb J, Medina LS (2007) Differentiation between pediatric spinal arachnoid and epidermoid-dermoid cysts: is diffusion-weighted MRI useful? Pediatr Radiol 37: 556-560. [Crossref]
- Dutt SN, Mirza S, Chavda SV, Irving RM (2002) Radiologic differentiation of intracranial epidermoids from arachnoid cysts. Otol Neurotol 23: 84-92. [Crossref]
- Barbagallo GMV, Maione M, Raudino G, Certo F (2017) Thoracic Intradural-Extramedullary Epidermoid Tumor: The Relevance for Resection of Classic Subarachnoid Space Microsurgical Anatomy in Modern Spinal Surgery.Technical Note and Review of the Literature. World Neurosurg 108: 54-61. [Crossref]
- Bretz A, Van den Berge D, Storme G (2003) Intraspinal epidermoid cyst successfully treated with radiotherapy: case report. Neurosurgery 53: 1429-1431. [Crossref]
- Cincu R, Lázaro JF, Liesa JL, Callizo JR (2007) Dorsal intramedullary spinal epidermoid cysts: report of two cases and review of literature. Indian J Orthop 41: 395-397. [Crossref]
