A Bullet Injury to the Liver Complicated by Biliary Broncho Pleural Fistula and IVC Thrombosis: Case Presentation and Review for Management Guidelines
A B S T R A C T
This is a case report of a 20-year-old male who presented to our hospital after sustaining a gunshot to the left upper abdominal quadrant with an exit right below the right scapula. On investigation, he was found to have a large right sided hemothorax and an extensive laceration in the liver. A right chest tube drain was inserted, initially drained blood and days later started draining bile. Consequently, the patient started coughing up bile and diagnosis of a biliary-broncho-pleural fistula was made. ERCP with sphincterotomy and stenting of a left hepatic duct injury was subsequently performed. The patient also developed an IVC thrombus that was discovered incidentally on follow up imaging and was treated with anticoagulation.
Keywords
Trauma, IVC, liver, biliary-bronchopleural fistula
Introduction
A bilio-pleural fistula and formation of bilio-pleural effusion is a rare but serious complication of thoraco-abdominal trauma. Moreover, review of the literature showed that the occurrence of inferior vena cava thrombosis post penetrating abdominal wall injury is rare and has not been well described in the literature. So far most of the reported cases were secondary to blunt abdominal trauma [1].
We report the case of a 20-year-old male who presented to our hospital after sustaining a gunshot to the left upper abdominal quadrant with an exit right below the right scapula. On investigation, he was found to have a large right sided hemothorax and an extensive laceration in the liver. A right chest tube drain was inserted, initially drained blood and days later started draining bile. Consequently, the patient started coughing up bile and diagnosis of a biliary-broncho-pleural fistula was made ERCP with sphincterotomy and stenting of a left hepatic duct injury was subsequently performed. The patient also developed an IVC thrombus that was discovered incidentally on follow up imaging and was treated with anticoagulation.
Case Presentation
This is a case report of a 20-year-old male previously healthy who presented to our emergency department at the American University of Beirut Medical Center (AUBMC) after having sustained a close-range gunshot injury to the abdomen. On presentation he was hemodynamically stable, awake and alert. The bullet entry site was in the left upper quadrant and the exit site was in the right subscapular region. The abdominal exam was positive for tenderness and voluntary guarding with a positive FAST (Focused Assessment with Sonography for Trauma) examination. The patient was resuscitated based on the ATLS protocol with two large bore IV cannulas and massive transfusion protocol (MTP) was activated based on injury mechanism. A right chest tube was inserted, and it drained 500 ml of blood on insertion. A CXR was done afterwards as part of the primary survey.
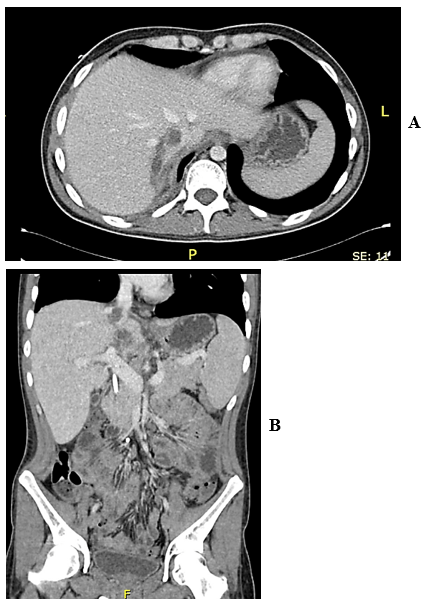
The patient underwent a CT scan on the way to the operating room in view of the patient’s hemodynamic stability and bullet trajectory in order to evaluate for combined chest and abdominal injuries. CT scan of the chest showed a right lung contusion and hemopneumothorax but no signs of active bleeding. CT of the abdomen showed an extensive liver laceration extending from segment II-VII and VIII (Figure 1) with no blush indicating active bleeding (Grade IV injury) as well as poor enhancement of IVC at the level of hiatus with associated hemoperitoneum.
In the operating room a midline laparotomy was done, the hemoperitoneum was evacuated and temporary control of bleeding was done with packing of the liver. Exploration of the four quadrants revealed a small serosal tear of the anterior wall of the stomach which was repaired. No small or large bowel injury was identified. The liver laceration was sutured primarily, and inspection of the retroperitoneum revealed no evidence of expanding hematoma. The chest tube output was monitored throughout the procedure and was noted to be less than 100ml/hr. so the decision was made to treat the lung injury conservatively.
Figure 1: CT image showing grade IV liver injury.
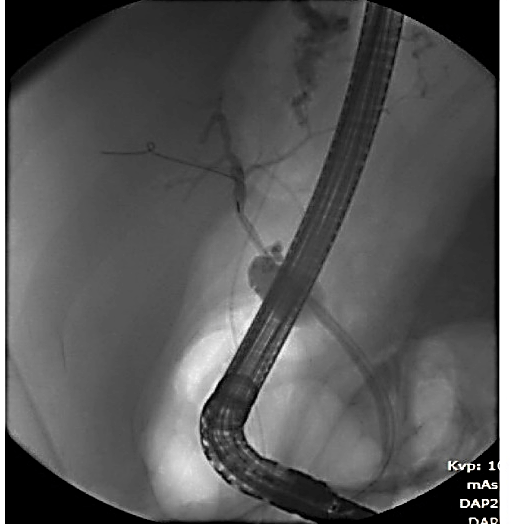
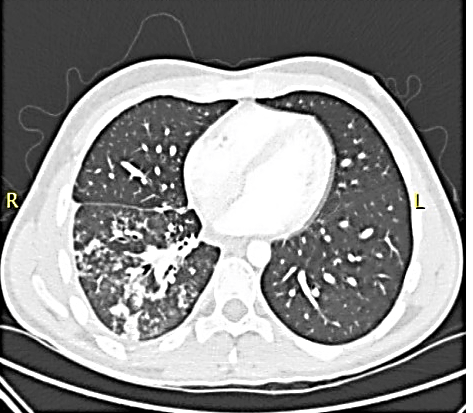
The patient was observed in the surgical intensive care unit (SICU) postoperatively for 24 hours and then transferred to the floor. On postoperative day 3 (POD#3) the chest tube output was noted to be bile tinged with a bilirubin level of 50 so we proceeded with ERCP which showed a left hepatic duct distal injury (Figure 2). A sphincterotomy and CBD stent was placed. Afterwards the chest tube output decreased but on POD#7 a loculated collection in the supra-diaphragmatic region was identified and treated with percutaneous drainage. Two days later the patient started coughing up bilious material and was diagnosed with a biliary-bronchopleural fistula with an output of around 100ml/24 hrs. The patient was started on Octreotide and antitussives with significant decrease in the output of the fistula. However, after one week of conservative management the patient developed high grade fever, atrial flutter and a picture of severe pneumonitis on imaging (Figure 3). He was transferred SICU again for optimization with antibiotics and pulmonary rehabilitation. The output of the biliary-bronchopleural fistula significantly decreased, and the sputum cleared up after two weeks of conservative management and the patient was discharged home after a total of 27 days, with a normal CXR.
Figure 2: ERCP showing extravasation of contrast from a branch of left hepatic duct.
Figure 3: CT image showing a right lower lobe consolidation with a tree-in-bud pattern.
The patient presented 3 days later with a picture of small bowel obstruction that failed to resolve on conservative management. He underwent a laparotomy with release of a single adhesive band. The patient did well thereafter and was discharged home after tolerating regular diet. The patient presented at POD#8, 3 days after he was discharged, with fever and supraventricular tachycardia. A CT scan was done which showed an IVC thrombus with a rim-enhancing collection that is contiguous with the thrombus suggestive of thrombophlebitis (Figure 4). The patient was started on therapeutic anticoagulation and IV antibiotics. He was discharged on prolonged, 6 months period, of anticoagulation. A follow up CT scan of abdomen showed near complete resolution of the IVC thrombus.
Figure 4: A)Axial CT scan cut showing the IVC thrombus. B) Coronal CT scan cut showing the IVC thrombus.
Discussion
Biliopleural fistula (BPF), first described by Graham back in 1987, is one of the dilemmas that patients with thoraco-abdominal penetrating traumas can present with [2]. BPF is an uncommon condition that, when discussed in previous case reports, was most frequently the consequence of hepatobiliary intervention or as a complication of many liver diseases, most commonly inflammatory, infectious or malignant [3]. When due to trauma, it can develop either secondary to injury to the diaphragm and adjacent liver or via diffusion of subdiaphragmatic fluid collection to the pleural cavity via diaphragmatic pores or by lymphatic [4]. In our case, the cause of biliary effusion was not clear initially as the diaphragm was found to be intact during exploratory laparotomy. However, Bamberger et al. hypothesizes that the injury might have been present but missed during the laparotomy as it could be very posterior. Even an iatrogenic injury that occurred during the exploration has been reported [5]. It is crucial to obtain an early diagnosis of BPF, whenever it is suspected, as an early management would reduce complications caused by the caustic action of bile on the pleura and lung. A BPF eventually leads to the development of a pleural effusion which predisposes to pneumonia with rapid progression to bilious empyema. Due to the excessive thickness of empyema, the lung will be entrapped, and its functions therefore compromised [6].
Such patients present with shortness of breath that may be accompanied by fever especially when an empyema forms, and by bilioptysis, a pathognomonic sign for BPF. Two other pathognomonic signs of BPF are the presence of bile on thoracentesis and a total bilirubin level higher than in the serum [7]. While there are multiple imaging modalities that help confirm the diagnosis of biliopleural fistula, endoscopic retrograde cholangiopancreatography remains the imaging modality of choice. It also provides the advantage of therapeutic intervention as it did in our case [8]. When performed on our patient, it revealed contrast extravasation from a branch of the left hepatic duct. Hence, a sphincterotomy was performed followed by the placement of a plastic stent into the bifurcation towards the left hepatic duct. The stent was removed 2 months later after confirming absence of contrast extravasation on ERCP.
Initial management of BPF is non-surgical. It is often successful as it was in our case and includes drainage via a chest tube, antibiotics, sphincterotomy and stenting with removal of the stents once healing occurs [9]. Indications for surgical intervention include but are not limited to respiratory compromise, presence of a large fistula and presence of tissue that needs debridement. Surgery involves fistula tract excision and destruction of the lung tissue by necrotizing bronchopneumonia [7].
With respect to thrombosis, different mechanisms reported in the literature dwell on the physiopathology of post traumatic IVC thrombosis. However, the exact mechanism if thrombosis in association with trauma is unclear. Virchow’s triad implies to IVC thrombosis in addition to other risk factor [1].
i. Lacerations from crush injury cause intimal tear with endothelial injury leading to IVC thrombus.
ii. Hepatic parenchymal injury and subsequent subcapsular hematoma, retroperitoneal hematoma or intra hepatic infections from bullet injury causing thrombophlebitis in the hepatic vein then anterograde to caval thrombosis.
iii. Hypercoagulability associated with suppression of fibrinolysis is a normal physiologic response after trauma.
The clinical manifestations of post traumatic IVC thrombosis are unclear and involve nonspecific signs as abdominal or back pain. It can also involve ascites, bilateral leg edema, phlebitis of lower limb, pulmonary embolism and Budd-Chiari syndrome [1]. However, in the case described above the thrombus was found incidentally on CT scan and fever could have represented the only clinical manifestation.
The delay of diagnosis varies through the literature from 3 days to 4 years [1]. So, a normal initial CT scan does not exclude the possibility of a thrombus formation later. In fact, IVC thrombosis is usually found 2-7 weeks after injury in the reported cases, indicating slow progression in formation. MRI imaging or cavography is required to delineate IVC anatomy and ascertain the distal extent of the thrombus [1, 10].
The management of post traumatic IVC thrombosis is not well described and remains a therapeutic challenge in traumatic context [1]. Pulmonary embolism is the most serious complication. However, early anticoagulation should be discussed on a case-by-case basis for fear of bleeding risk initially from hepatic laceration and other active bleeding lesions. Unfractionated heparin is the mainstay of treatment for patients with IVC thrombosis targeting an activated partial thromboplastin time twice the normal value [1]. Other alternative such IVC filter or surgical thrombectomy may be used when the bleeding risk is increased [1]. Outcome can be favorable even with non-surgical approaches. Interventional vascular techniques have become an important alternative approach for the treatment of many vessel lesions.
Conclusion
Though atypical, a BPF is a complication of thoracoabdominal traumas that should not be missed. It is often suspected following a bilious pleural effusion. That would warrant an ERCP to confirm as well as treat the defect. It is usually managed non-operatively and surgery should be reserved to those who fail to respond to non-surgical treatment. Moreover, a normal CT at the initial presentation does not exclude the possibility for development of IVC thrombosis later on. Nonspecific symptoms should warrant investigations to rule out IVC thrombosis. Management should be addressed case by case outweighing the risks and benefits.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Sat 20, Jun 2020Accepted: Thu 02, Jul 2020
Published: Fri 10, Jul 2020
Copyright
© 2023 Arwa El Rifai. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.SCR.2020.07.07
Author Info
Arwa El Rifai M. Zorkot S. Emsieh G. Abi Saad
Corresponding Author
Arwa El RifaiDepartment of Surgery, American University of Beirut Medical Center, Beirut, Lebanon
Figures & Tables

References
- Amine Chakroun, Mohamed Said Nakhli, Mohamed Kahloul, Mohamed Amine Harrathi et al. (2017) Post traumatic inferior vena cava thrombosis: A case report and review of literature. Int J Surg Case Rep 36: 59-63. [Crossref]
- J E Graham (1897) Observations on Broncho-Biliary Fistula: (With the Reports of Two Cases). Br Med J 1: 1397-1400 [Crossref]
- G N Ramesh, A Duggal, J C Vij (1991) Successful treatment of post-operative pleurobiliary fistula by endoscopic technique. Gastrointest Endosc 37: 574-576. [Crossref]
- Ghritlaharey R. K (2008) Posttraumatic bilothorax in a child: a case report. J Clin Diagnost Res 2: 760-763.
- P K Bamberger, A Stojadinovic, G Shaked, M Golocovsky (1997) Biliary-pleural fistula presenting as a massive pleural effusion after thoracoabdominal penetrating trauma. J Trauma 43: 162-163. [Crossref]
- Margaret M. Johnson, Jr R. Chin, Edward F. Haponik (1996) Thoracobiliary fistula. South Med Jl 89: 335-339.
- Divya Dahiya, Lileswar Kaman, Arunanshu Behera (2015) Biliopleural fistula following gunshot injury in right axilla. BMJ Case Rep 2015: bcr2014207454. [Crossref]
- S G Thrumurthy, A H Anuruddha, M I De Zoysa, D N Samarasekera (2011) ERCP for the treatment of traumatic biliobronchial and biliocutaneous fistulas. Endoscopy 43: E42. [Crossref]
- Avraham Z Cooper, Alok Gupta, Stephen R Odom (2012) Conservative management of a bilothorax resulting from blunt hepatic trauma. Ann Thorac Surg 93: 2043-2044. [Crossref]
- Masaki Hamamoto, Taira Kobayashi, Hiroshi Kodama, Atsushi Nakamitsu, Masaru Sasaki et al. (2013) Thrombectomy under cardiopulmonary bypass for inferior vena cava thrombosis induced by liver injury. Ann Vasc Dis 6: 751-755. [Crossref]
