What is the Obstetric Outcome with a Large Loop Excision of the Transformation Zone (LLETZ) for Cervical Intraepithelial Neoplasia?
A B S T R A C T
Objective: To find out the association of large loop excision of the transformation zone (LLETZ) at or less than 36 weeks of gestation, extreme preterm delivery at or less than 28 weeks gestation and perinatal mortality with premature birth.
Design: Data was collected from euroking, ‘joe’ and e-searcher systems of 407 retrospective cases. The data were analysed pre and post cervical histology between 20-43 weeks of pregnancy to identify live births.
Setting: East Sussex Healthcare Trust
Population: The selected population were women who became pregnant after LLETZ treatment at the East Sussex hospital. Their case notes and histology reports were taken into account. The women who were not included in this study were those in age group greater than 42 years, previous premature labour or twin pregnancies.
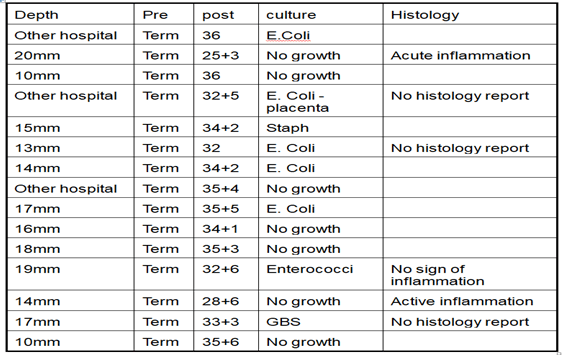
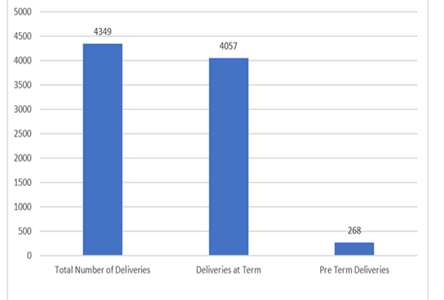
Result: Total number of deliveries in East Sussex hospital in a year were 4349 and the deliveries at term gestation (37 +) were 4057. The total number of all preterm deliveries were 268 (6.16 %), 34 to 36+6 weeks were 198 (4.55 %) and less than 34 weeks were 70 (1.6 %). In 24 cases gestation was unknown.
The total data collected were of 407 LLETZ treatment cases. The number of premature deliveries were 45 (11 %) as against background risk of 6.16%. Those who had term pregnancy prior to LLETZ were 15 out of these 45 cases, and the remaining had their first pregnancy after having LLETZ.
Conclusion: LLETZ increases the chances of premature births.
Keywords
Large loop excision of the transformation zone (LLETZ), preterm, premature parturition
Introduction
The aim of screening is to detect precancerous changes in the cervix and treat before they become malignant. Cartier et al. was the first one to relate large loop excision of the transformation zone (LLETZ) for CIN in 1981 [1]. The mortality from cancer of cervix has fallen dramatically since then. The cone biopsy related morbidity has reduced but there remained a question about the effect of LLETZ on pregnancy outcome. In England women with abnormal cervical samples at screening are sent for colposcopy for further management. The women referred to colposcopy clinic may not have any procedure or may have biopsy to detect presence or absence of abnormality. Women with results of high-grade abnormalities of cervical cytology at their first visit have the excisional treatment, such women are frequently treated by LLETZ [2]. Since the introduction of LLETZ different studies has been published with slightly different results, but the unanimous conclusion is that LLETZ is associated with increase in the rate of preterm birth. There has been no randomized controlled trials to evaluate the relationship between the LLETZ and preterm birth though association has been reported in multiple retrospective cohort studies [3]. Families and the community are affected with emotional and economic costs of the preterm infants, which has an impact on health services.
This study attempts to address the risk of severe preterm (< 34 weeks) delivery, extreme preterm < 28 weeks delivery, perinatal mortality, and low birth weight associated with previous LLETZ to cervix. The main focus of the study was on the relationship between preterm parturition and the treatment.
Methods
The data was collected from clinical records in East Sussex hospital as having had a cervical histology sample taken by LLETZ. We obtained information from the hospital record on the month and year of delivery, gestational age, birth weight, onset of delivery, mode of delivery, and number of previous pregnancies. The study design was observational, and the sampling technique was purposive. The data was collected respectively from electronic source euroking, ‘joe’ and e-searcher systems respectively, with permission and supervision of audit department. The cases considered were between 20 to 43 weeks of gestation. We considered only births with a known gestational age and that were between 20 and 43 weeks. The exclusion criteria were age greater than 42 years, previous premature labour, antepartum stillbirths and multiple births (twins and triplets). The total number of cases who had LLETZ were 407.
Statistical Analysis
Figure 1:
Results
Total number of deliveries East Sussex hospital in a year were 4349 and deliveries at term gestation (37 +) were 4057. Total number of all preterm deliveries 268 (6.16 %), 34 to 36+6 weeks were 198 (4.55 %) and less than 34 weeks were 70 (1.6 %). In 24 cases gestation was unknown.
Figure 2:
Figure 3:
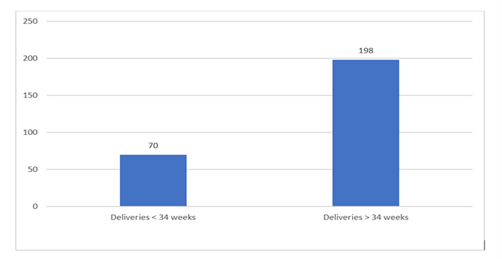
The total number of data collected were of 407 LLETZ treatment cases. Total numbers of preterm deliveries less than 37 weeks were 45 (11 %) as against background risk of 6.16%. Out of 45 women, 15 had term pregnancies prior to LLETZ, whereas the remaining were pregnant for the first time beyond after having LLETZ. We considered women with treatment and compared births after treatment with before treatment.
There were 11 cases who delivered less than 34 weeks. The incidence rate was 2.7 % as against background risk of 1.6% (70 % increase). Total number of preterm deliveries between 28 and 34 weeks gestation were eight. The total number of preterm deliveries under 28 weeks gestation were three. In three cases under 28 weeks the depth of tissue removed were 20 mm, 14 mm and one case had it done in another hospital. All three cases had signs of inflammation reported from histology, on infection screening. In eight cases of 28 to 34 weeks the depth of tissue removed in three cases were 10-14 mm and in four cases it was more than 15 mm and one case was done in different hospital. Out of 8 cases 5 had evidence of infection or inflammation. In one case there was no evidence of inflammation on histology though no swab result was available. In 2 cases there was no swab/histology result available. Women who had preterm delivery before 34 weeks gestation, eight out of eleven of them showed evidence of infection or inflammation on the high vaginal swab culture, mid specimen urine culture, placental swab culture or placental histology report.
Pregnancy Outcome - Pre and Post Lletz
Discussion
The study disclosed that after LLETZ treatment, the risk of premature parturition increases in all categories. Though the aim of study was to look at the risk of preterm parturition after LLETZ, we did not adjust for possible confounding factors such as racial, culture, social class and smoking, which may incline the woman to abnormal cervical cytology and preterm parturition. There is a possibility that in high grade abnormality women may have preterm delivery due to disease itself rather than treatment.
The exact mechanism of preterm labour after LLETZ is uncertain. Many studies supports that there was greater risk of morphological and functional damage to the cervix when greater amount of tissue was removed. It is obvious that cervix function would be compromised on taking away or injuring a large volume of cervical tissue. There are number of factors responsible for functional damage, which might include the diathermy for haemostasis when volume of tissue is taken off and injury is inflicted after LLETZ and the area of involvement of endocervical canal epithelium [3-5].
Comparison with Other Studies
Study done by Khalid et al., reveals that chances of preterm labour increases with the bulk and the total volume of tissue removed of the cervix [3]. The small amount of tissue removed has less comorbidity compared to deeper excisions of 1.2 cm and larger than 6 cm3 which have a risk of preterm labour of three times. In most of our cases the depth of tissue removed was more than recommended in this study. In a retrospective cohort study done by Jakobsson M et.al. the risk for preterm delivery < 37 weeks was increased almost three times and in cases with repeat LLETZ the risk increased to more than five times, compared with the background risk [6]. The preterm parturition rate before and after the procedure, was 6.5% before and 12% respectively, which is similar to our study 11 % as against background risk of 6.16%. This is comparable to a norwegian record linkage study which is the largest study to date.
In this study births before treatment were 57136 and 15108 after the treatment, the percentage of preterm parturition 6.7% and 17.2% in each group, respectively [7]. Arbyn M et.al. result showed LLETZ had no relation with a greater occurrence of low birth weight, severe, extreme preterm delivery and perinatal death [8]. They also concluded LLETZ cannot be considered as completely safe and free of any harmful effect. In a systemic review and meta-analysis by Dan of NA et al., they compared women before or during pregnancy with untreated CIN, revealed a higher chance of preterm birth of < 37 weeks [9]. A largely mentioned meta-analysis in 2006 of twenty seven studies revealed relation of low birth weight, preterm premature rupture of membranes, premature parturition with large loop excision of the transformation zone [10]. Kyrgiou et al. reported in a meta analytic study that the risks for preterm birth was 1.7 times greater among women treated with large loop excision of the transformation zone compared to those with no treatment [10].
In a dutch cohort study with 45,259 it was observed that women had a 1.51 times increased likelihood of preterm birth opposed to untreated CIN [11]. It was also observed that the likelihood of preterm birth was increased by 2.20 times when the bulk of cervix removed was of 0.5 to 0.9 cc. The women with cervical removed volume of 4 to 8.9 cc had risk of preterm further increased to 3.13 times and 5.93 respectively. In a meta analytic study of sixty nine studies the relative risk of prematurity with LLETZ were 1.58 [12]. In a large sample retrospective study of ten years with LLETZ treatment, CIN 1, 2, 3 had mean extent of surgical removal of 9.9 mm, 11.4 mm and 8.5 mm respectively. The difference in depth between excisions with CIN 2 and 3 were significant (p = 0.019). Women with CIN 2 had the deepest excision, but women with CIN 3 had more of preterm deliveries. This retrospective analysis suggested factors other than mechanical weakness may be responsible for preterm delivery with LLETZ [13]. The bulk of cervical tissue removed was linked with preterm delivery in another systematic review and meta-analysis of seventy one studies with sixty five thousand and eighty two treated cases. The risk ratio was 1.56 for preterm delivery with LLETZ. In excision less than 10 mm depth the risks were present, and it was two times greater for excisions larger than 10 mm. It was increased to three times when surgical removal was greater than 15-17 mm, and almost increased to five times when removal exceeded 20 mm in depth [14].
The general rate of preterm delivery in England is 6.7% [4]. The women having abnormal cytology attending colposcopy have more likelihood of preterm parturition than the general population of England [4]. The risk of preterm birth in England in women treated with colposcopy were less in many studies from Scandinavian countries [15]. There are few studies from the United Kingdom confirming the strong association between LLETZ and subsequent preterm birth but generally those studies are small [16-18]. Many studies have recommended that it is the proportion of tissue excised from the cervix rather than the procedure itself which causes excessive risk [19-21].
On the other hand, there are other studies which suggest that treatment does not increase the probability of unfavourable pregnancy outcomes, it may be an effect of confounding [15, 16]. The ascending infection from the vagina to the fetus and placenta and coincident inflammation are associated with preterm labour. Our study showed increased risk in severe, extreme preterm category were associated with infection as shown in swab culture and histology report.
Conclusion
Our data support the conclusion that women who previously had LLETZ have an increased likelihood of preterm parturition as observed in many other studies [22-24]. This suggests to limit the use of LLETZ to high-grade lesions of cervical intraepithelial neoplasia (CIN2+), and to avoid surgery for CIN1 lesions. The excision with depth greater than 10 mm is linked with a higher risk of unfavourable obstetrical consequences and to be avoided where possible. There is need to be cautious when treating women of reproductive age with CIN especially when treatment can be delayed or can be offered to high-risk cases.
LLETZ has significant risk of preterm parturition especially in the early gestation. LLETZ has higher chance of preterm parturition in all categories. According to our study extreme preterm delivery is associated with infection as shown in swab culture and histology report. LLETZ increases preterm delivery rate even in those with previous term delivery. The greater the depth of tissue excised at LLETZ, greater is the chance of preterm parturition. All those who had LLETZ should be offered to have cervical length measurement and high vaginal swabs in mid trimester. All placentas from preterm delivery should be swabbed and sent for histology.
Conclusions were difficult in previous studies concerning the relation between LLETZ and preterm birth due to many methodological issues e.g. case controlled plans, small study sizes, right control group, bad standard for confounding factors. In order to determine statistical importance larger studies with significance on the pathophysiology of preterm birth are required. We consider that all child bearing age women should be counselled about the possible consequences on subsequent pregnancies. While managing women of child bearing age the aim should be to minimize possible poor obstetric effect and concomitantly minimizing the left over disease rates. The human papillomavirus vaccination programmers significantly diminish the prevalence of cervical precancerous changes and prevent morbidity associated with the treatment.
Limitation
We have failed to investigate properly in more than fifty percent of women to find out probable cause of preterm delivery. We did not modify for possible confounding factors such as smoking, race, culture and customs that might put a woman at risk to abnormal cervical cytopathology resulting in preterm parturition. We also did not compare treated with untreated women.
Author Contributions
Shabnum Sibtain: Conceived the idea, authored the study, literature review, data analysis, reviewed the study. Ashok Mohanty: Conceived the idea, authored the study, literature review, data analysis, reviewed the study. Prabha Sinha: Conceived the idea and reviewed the study. J Zaidi: Conceived the idea and reviewed the study.
Conflicts of Interest
None.
Ethics Approval
Not required.
Funding
None.
Article Info
Article Type
Research ArticlePublication history
Received: Fri 01, Sep 2023Accepted: Wed 20, Sep 2023
Published: Mon 09, Oct 2023
Copyright
© 2023 Shabnum Sibtain. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2023.03.01
Author Info
Shabnum Sibtain Ashok Mohanty Prabha Sinha J Zaidi
Corresponding Author
Shabnum SibtainDepartment of Obstetrics and Gynecology, Azra Naheed Medical College, Lahore, Pakistan
Figures & Tables

References
1.
Gazvani MR, ÖZTÜRK O (2001) Large Loop Excision of the
Transformation Zone: An Outpatient Procedure. Turk J Med Sci 31:
435-438.
2.
(2006) Cervical screening programme, England: 2005-06.
NHS Information Centre.
3.
Khalid S, Dimitriou E, Conroy R, Paraskevaidis E,
Kyrgiou M et al. (2012) The thickness and volume of LLETZ specimens can predict
the relative risk of pregnancy-related morbidity. BJOG 119: 685-691. [Crossref]
4.
Castanon A, Landy R, Brocklehurst P, Evans H, Peebles D
et al. (2014) Risk of preterm delivery with increasing depth of excision for
cervical intraepithelial neoplasia in England: nested case-control study. BMJ
349: g6223. [Crossref]
5.
Bruinsma FJ, Quinn MA (2011) The risk of preterm birth
following treatment for precancerous changes in the cervix: a systematic review
and meta-analysis. BJOG 118: 1031-1041. [Crossref]
6.
Jakobsson M, Gissler M, Paavonen J, Tapper AM (2009)
Loop electrosurgical excision procedure and the risk for preterm birth. Obstet
Gynecol 114: 504-510. [Crossref]
7.
Albrechtsen S, Rasmussen S, Thoresen S, Irgens LM,
Iversen OE (2008) Pregnancy outcome in women before and after cervical
conisation: population based cohort study. BMJ 337: a1343. [Crossref]
8.
Arbyn M, Kyrgiou M, Simoens C, Raifu AO, Koliopoulos G
et al. (2008) Perinatal mortality and other severe adverse pregnancy outcomes
associated with treatment of cervical intraepithelial neoplasia: meta-analysis.
BMJ 337: a1284. [Crossref]
9.
Danhof NA, Kamphuis EI, Limpens J, van Lonkhuijzen LR,
Pajkrt E et al. (2015) The risk of preterm birth of treated versus untreated
cervical intraepithelial neoplasia (CIN): a systematic review and
meta-analysis. Eur J Obstet Gynecol Reprod Biol 188: 24-33. [Crossref]
10. Kyrgiou
M, Koliopoulos G, Martin Hirsch PL, Arbyn M, Prendiville W et al. (2006)
Obstetric outcome after conservative treatment for intraepithelial or early invasive
cervical lesions: systematic review and meta-analysis. Lancet 367:
489-498. [Crossref]
11. Loopik
DL, van Drongelen J, Bekkers RLM, Voorham QJM, Melchers WJG et al. (2021)
Cervical intraepithelial neoplasia and the risk of spontaneous preterm birth: A
Dutch population-based cohort study with 45,259 pregnancy outcomes. PLoS Med
18: e1003665. [Crossref]
12. Kyrgiou
M, Athanasiou A, Kalliala IEJ, Paraskevaidi M, Mitra A et al. (2017) Obstetric
outcomes after conservative treatment for cervical intraepithelial lesions and
early invasive disease. Cochrane Database Syst Rev 11:CD012847. [Crossref]
13. Maguire
PJ, McCarthy CM, Molony P, O’Donovan E, Walsh T (2019) Large loop excision of
the transformation zone and preterm delivery over a decade in a major women’s
hospital. Ir J Med Sci 188: 579-581. [Crossref]
14. Kyrgiou
M, Athanasiou A, Paraskevaidi M, Mitra A, Kalliala I et al. (2016) Adverse
obstetric outcomes after local treatment for cervical preinvasive and early
invasive disease according to cone depth: systematic review and meta-analysis BMJ
354: i3633. [Crossref]
15. Castanon
A, Brocklehurst P, Evans H, Peebles D, Singh N et al. (2012) Risk of preterm
birth after treatment for cervical intraepithelial neoplasia among women
attending colposcopy in England: retrospective-prospective cohort study. BMJ
345: e5174. [Crossref]
16. Reilly
R, Paranjothy S, Beer H, Brooks CJ, Fielder H et al. (2012) Birth outcomes
following treatment for precancerous changes to the cervix: a population-based
record linkage study. BJOG 119: 236-244. [Crossref]
17. Shanbhag
S, Clark H, Timmaraju V, Bhattacharya S, Cruickshank M (2009) Pregnancy outcome
after treatment for cervical intraepithelial neoplasia. Obstet Gynecol
114: 727-735. [Crossref]
18. Tan
L, Pepera E, Haloob RK. (2004) The outcome of pregnancy after large loop
excision of the transformation zone of the cervix. J Obstet Gynaecol 24:
25-27. [Crossref]
19. Noehr
B, Jensen A, Frederiksen K, Tabor A, Kjaer SK (2009) Loop electrosurgical
excision of the cervix and subsequent risk for spontaneous preterm delivery: a
population-based study of singleton deliveries during a 9-year period. Am J
Obstet Gynecol 201: 33,e1-e6. [Crossref]
20. Acharya
G, Kjeldberg I, Hansen SM, Sorheim N, Jacobsen BK et al. (2005) Pregnancy outcome
after loop electrosurgical excision procedure for the management of cervical
intraepithelial neoplasia. Arch Gynecol Obstet 272: 109-112. [Crossref]
21. Sadler
L, Saftlas A, Wang W, Exeter M, Whittaker J et al. (2004) Treatment for
cervical intraepithelial neoplasia and risk of preterm delivery. JAMA
291: 2100-2106. [Crossref]
22. Zhuang
H, Hong S, Zheng L, Zhang L, Zhuang X et al. (2019) Effects of cervical
conisation on pregnancy outcome: a meta-analysis. J Obstet Gynaecol 39:
74-81. [Crossref]
23. Jin G, LanLan Z, Li C, Dan Z (2014) Pregnancy outcome following loop electrosurgical excision procedure (LEEP) a systematic review and meta-analysis. Arch Gynecol Obstet 289: 85-99. [Crossref]
24. Jančar N, Ponikvar BM, Tomšič S (2016) Cold-knife conisation and large loop excision of transformation zone significantly increase the risk for spontaneous preterm birth: a population-based cohort study. Eur J Obstet Gynecol Reprod Biol 203: 245-249. [Crossref]
