Wellbeing in UK Frontline Healthcare Workers During Peaks One and Three of the COVID-19 Pandemic: A Retrospective Cross-Sectional Analysis
A B S T R A C T
Background: COVID-19 had a huge impact on the wellbeing of healthcare workers (HCWs). This is well documented during the first peak of the pandemic. With cases in the UK rising for a third peak, hospitalisations and deaths surpassing the first, there is very little known about the mental health of HCWs during this time.
Methods: Using a questionnaire, data was collected from patient-facing staff at Barking, Havering, and Redbridge University Trust to quantify and compare the period prevalence of symptoms of depression, anxiety, and PTSD during the first peak (P1: March-May 2020) and third peak (P3: December 2020-Feburary 2021) of the COVID-19 pandemic as well as wellbeing service use, demographics of responders and what they found most difficult during the peaks.
Results: Of 158 responders, only 22·4% felt they had enough access to wellbeing services during P1 and 21·5% in P3. Of those who used wellbeing services 34·4% found them useful in P1 and 34·6% in P3. 70·3% of responders felt that not enough was done for staff wellbeing. The median anxiety score decreased from P1 (10(range 5-17)) to P3 (8(range 4-16)) p=0·031. Under 30-year-olds’ depression and PTSD scores increased from P1 to P3 (depression: P1 7(1-11), P3 8(3-14), p=0·048, PTSD: P1 4(0-7) peak 3 5(2-9), p=0·037). Several groups showed a decrease in anxiety scores from P1 to P3 including; over 30-year-olds (P1 10(5-17), P3 7(3-15) p=0·002), BME responders (P1 8(3·75-15) P3 6·5(1-12) p=0·006), AHP (P1 14(7-19), P3 11(5-19) p=0·005), ITU workers (P1 15(8-18·25) P3 12(5·75-18·25) p=0·004), and those who were redeployed (P1 8(5-18·25), P3 5(2-14·75), p=0·032).
Conclusion: We have observed changes in mental health symptoms within the study population as the peaks of the pandemic continue. With the majority of responders reporting they felt not enough had been done for their wellbeing support - and of those who used the wellbeing services only around 1/3 felt they were useful - we hope that this paper can help inform wellbeing provision and identify groups at higher risk of developing mental health symptoms.
Keywords
COVID-19, COVID-19 and mental health, wellbeing in healthcare, mental health in healthcare professionals, depression, anxiety, PTSD
Introduction
Since the start of the COVID-19 pandemic, the UK has experienced vast numbers of COVID-19 cases. The first peak (P1) of the pandemic from March to May 2020 required mass restructuring of the National Health Service (NHS) and daily deaths reached a height of 1,075 [1]. Cases rose again from September to November 2020, before the third peak of cases was seen from December 2020 [2]. This third peak (P3) of COVID-19 in the UK superseded the hospitalisations and deaths seen in P1, with 80% greater hospital bed occupancy and greater total mortality than P1 [1, 3].
The pandemic has provoked an enormous body of literature globally, with many studies suggesting a high prevalence of anxiety, depression, post-traumatic stress disorder (PTSD), stress and sleep disturbance in healthcare workers (HCWs) during the first months of the pandemic. Though individual study designs and results were variable, systematic reviews and meta-analyses indicate that the strain on the wellbeing in HCWs at this time may have been extensive [4, 5]. Protective factors against poor mental health in the first peaks of COVID-19 have been identified, such as access to personal protective equipment (PPE), and access to wellbeing services [6, 7]. Negative factors include female gender, clinical inexperience, redeployment, moral injury, and high levels of exposure [5-11]. Comparatively, little is known regarding the progression of HCW wellbeing with time and evolution of the pandemic. Some studies have found the mental health of HCWs to recover with time as case numbers ease whereas others have seen high levels of poor mental health remain static or even worsen [12-18]. Even fewer studies compare how HCW wellbeing changes when further peaks of the pandemic are encountered. A Japanese longitudinal survey examining the mental health of HCWs over 8 months of outbreaks indicates that mental health may deteriorate as further peaks are encountered [19]. Despite the enormity of P3 of COVID-19 cases in the UK, there is minimal published literature regarding the impact of the largest peak yet on the wellbeing of HCWs, or how this impact might differ from that of the first. Only McFadden et al. 2021 have probed this question, finding that wellbeing and quality of life deteriorated between the first and largest peaks of cases [20]. However, 75% of the HCWs in the study were social workers, so these results may not be reflected in frontline healthcare workers.
Through a single-site retrospective cross-sectional study design, a questionnaire was used to compare the wellbeing of patient-facing HCWs (nurses, doctors, healthcare assistants (HCA), and therapists) within Barking, Havering, and Redbridge University Trust (BHRUT) during P1 and P3. This aimed to assess the period-prevalence of symptoms of depression, anxiety, and PTSD, compare any difference between the peaks and determine if these differences were associated with any protective or risk factors related to demographics, workplace environment, or uptake of wellbeing provisions.
Methods
I Participants and Procedures
An anonymised questionnaire was designed to assess staff experience of working during the COVID-19 pandemic UK peaks. The questionnaire collected information regarding P1, defined as 1/3/20-31/5/20 and P3, defined as 1/12/20-28/2/21. P1 and P3 were selected for this data set as they represent the largest COVID-19 patient burden in the UK and therefore should demonstrate the greatest impact on staff wellbeing. P3 was analysed individually as this peak has been less frequently investigated in the literature, before comparing the two peaks to identify any change in symptom prevalence between the peaks.
The questionnaire collected data on demographics (gender, ethnicity, age, role, specialty area), access to and uptake of wellbeing services, factors that staff found most difficult during the COVID-19 peaks, whether they were redeployed and whether they had opportunities to debrief following difficult events. Using the validated self-reporting questionnaires for depression (PHQ-9), anxiety (GAD-7), and PTSD (TSQ) we measured the period-prevalence of symptoms of depression, anxiety, and PTSD respectfully. Questions were modified to use only lay terms and repeated question lines were removed for brevity.
Responders were recruited by disseminating the questionnaire to all patient-facing staff working in BHRUT via a hyperlink in an email. The hyperlink included instructions for the questionnaire and a statement explaining that by submitting the questionnaire, participants were consenting to their responses being used in this study. No identifiable data was collected or stored.
II Inclusion/Exclusion Criteria
Participants were required to have a patient-facing role including doctors of all grades, nurses, advanced nurse practitioners, HCA, therapists including physiotherapists, occupational therapists, and speech and language therapists. Participants were required to work at BHRUT at the time of data collection and at any NHS trust during P1. Exclusion criteria included any non-patient facing roles and staff who did not work at all during P1 or P3.
III Statistical Analysis
For each responder, a score was produced which represented the frequency of symptoms of depression, anxiety, and PTSD experienced during P1 and P3. The maximum potential score for depression was 21, anxiety was 21 and PTSD was 10. Data produced did not follow a gaussian distribution, therefore Mann-Whitney and Wilcoxon signed-ranks tests were used as appropriate to measure differences between groups. A p<0·05 was used to signify statistical significance. Data is shown as median and IQR or as percentages. Box plots produced show median, upper and lower quartiles and range of scores. Asterix represents significant differences between the groups analysed.
Questionnaires with discrete incomplete sections were not included in the relevant section’s analysis. Responders with variation between the two peaks (i.e., area worked, redeployment status, use of wellbeing services) were not included in the overall analysis for that variable.
Age range was grouped into <30-year-olds and >30-year-olds to reflect responders who were recently out of training compared to those who had been established in their careers prior to the pandemic. Job role was also grouped into doctors (foundation trainees to consultants) and allied health professionals (AHP - nurses, HCA (healthcare assistants), therapists), the latter having more close contact with patients. Intensive therapy unit (ITU) staff were also grouped separately to all other areas of the hospital.
Changes in symptom prevalence for depression, anxiety, and PTSD in P1 were compared to P3. For baseline responder descriptors (e.g., age, gender, role) the prevalence of reported symptoms for P3 and a difference between the two peaks were calculated and compared between groups.
Questionnaires that reached the clinically significant diagnostic threshold for GAD-9, and TSQ-9 were displayed as a percentage for P1 and P3. This was not done for PHQ-9 as some of the questions were edited or removed for brevity. The factors that staff reported as finding most difficult for each peak were represented by a percentage.
Results
158 questionnaires were completed. Seven questionnaires had incomplete fields; these missing fields were excluded during the relevant analysis. A summary of responder demographics is shown in (Table 1).
Table 1: Summary of responder demographics.
|
Demographic
|
|
n |
% |
|
Gender |
Female |
111 |
70·3 |
|
|
Male |
47 |
29·7 |
|
Age (y) |
≤30 |
41 |
25·9 |
|
|
31-40 |
45 |
28·5 |
|
|
41-50 |
38 |
24·1 |
|
|
51-60 |
26 |
16·5 |
|
|
≥61 |
8 |
5·1 |
|
Ethnicity |
BME |
79 |
50·0 |
|
|
White |
76 |
48·1 |
|
|
Prefer not to say |
3 |
1·9 |
|
Subgroups of BME |
Arab |
1 |
12·7 |
|
|
Asian or Asian British |
48 |
60·8 |
|
|
Black or Black British |
12 |
15·2 |
|
|
Mixed |
6 |
7·6 |
|
|
Other |
12 |
15·2 |
|
Job role |
Allied health professional |
104 |
65·8 |
|
|
Doctor |
54 |
34·2 |
|
Subgroups of AHP |
Nurse/ANP |
83 |
79·8 |
|
|
Therapist (OT/PT/SALT) |
10 |
9·6 |
|
|
HCA |
11 |
10·6 |
|
Subgroups of doctors |
Consultant |
9 |
16·7 |
|
|
Registrar |
13 |
24·1 |
|
|
Specialty training (pre-registrar) |
14 |
25·9 |
|
|
Foundation |
18 |
33·3 |
|
Area worked |
ITU both peaks |
58 |
36·7 |
|
|
Other area both peaks |
87 |
55·1 |
|
|
Mixed areas |
13 |
8·2 |
|
Redeployed |
Both peaks |
20 |
12·7 |
|
|
Neither peak |
102 |
64·6 |
|
|
Mixed redeployment |
36 |
22·8 |
AHP:
Allied Health Professional, BME: Black Minority Ethnicities, ANP: Advanced
Nurse Practitioner, OT: Occupational Therapist, PT: Physiotherapist, SALT:
Speech and Language Therapist, ITU: Intensive Therapy Unit.
Table 2: Summary of opinion regarding wellbeing services.
|
|
|
P1 |
P3 |
||
|
|
|
n |
% |
n |
% |
|
Staff opinion regarding access to wellbeing
services |
Sufficient |
34 |
22·4 |
34 |
21·5 |
|
Insufficient |
82 |
53·9 |
80 |
50·6 |
|
|
No difference |
36 |
23·7 |
44 |
27·8 |
|
|
Did staff use wellbeing services |
Yes |
35 |
22·2 |
26 |
16·5 |
|
No |
123 |
77·8 |
132 |
83·5 |
|
|
Of those who used wellbeing services,
staff opinion regarding whether they found this service useful |
Yes |
12 |
34·3 |
9 |
34·6 |
|
No |
12 |
34·3 |
9 |
34·6 |
|
|
No difference |
11 |
31·4 |
8 |
30·8 |
|
I Wellbeing Provision
A summary of wellbeing service use in P1 and P3 is shown in (Table 2). During P1, 53·9% of responders felt that they did not have adequate access to wellbeing services, and only 22·4% felt that they did, compared with 50·6% and 21·5% respectively in peak 3.
22·2% of responders reported using wellbeing services in P1; 34·3% of which felt they were unhelpful, 34·3% felt that they were helpful and 31·4% felt they made no difference. 16·5% of responders used wellbeing services in P3; 34·6% felt these were unhelpful, 34·6% found them helpful and 30·8% felt they made no difference.
During P1, 41·1% of responders reported having the opportunity to debrief with their team following difficult events. This dropped to 39·2% in P3. When comparing the two peaks, 56·3% of responders felt that morale was better during P1, 15·2% felt it was better in P3 and 28·5% felt there was no difference.
43·3% of responders found P1 more difficult, 38·2% found P3 more difficult and 18·5% felt there was no difference. When asked whether the responders felt that enough was done for staff wellbeing overall 70·3% answered no and only 29·7% answered yes.
The score for symptoms of depression, anxiety, and PTSD: The median anxiety score decreased from P1 to P3 (P1 10(range 5-17), P3 8(range 4-16) p=0·031). The median depression and PTSD scores did not significantly differ between the peaks (depression: P1 7(3-13) P3 7(3-13) p=0·54, PTSD: P1 5(2-8) P3 6(2-9) p=0·24).
II Peak 3
Analysing depression, anxiety, and PTSD scores from P3 only, women had higher depression and anxiety scores than men (depression: female 9(4-13), male 3(0-9) p=0·002, anxiety: female 10(4-18), male 4(0-11·5), p<0·001, Figure 1).
Figure 1: Depression and anxiety scores for males and females during P3.
P3: Peak 3.
Black and minority ethnic (BME) responders had lower depression and anxiety scores than Caucasian responders (depression: BME 6(2-10·5), Caucasian 9(4-14) p=0·003, anxiety: BME 8(1·5-12), Caucasian 12(5-18·5) p<0·001), shown in (Figure 2).
Figure 2: Depression and anxiety scores for BME and Caucasian responders during P3.
BME: Black and Minority Ethnic, P3: Peak 3.
Allied health professionals (AHP) had higher depression, anxiety and PTSD scores compared to doctors (depression: AHP 9(4-14), doctor 4(0-8) p<0·001, anxiety: AHP 11(4·5-18·5), doctor 4·5(0-11), p<0·001, PTSD: AHP 7(3-9), doctor 3(0-8) p<0·001), shown in (Figure 3).
Figure 3: Depression, anxiety and PTSD scores for AHP and doctors during P3.
P3: Peak 3, PTSD: Post Traumatic Stress Disorder.
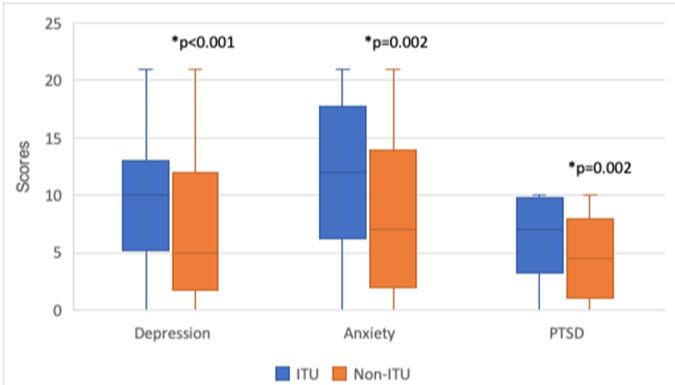
Those who worked in ITU for both peaks had higher depression, anxiety, and PTSD scores compared to those working in other areas of medicine/surgery (depression: ITU 10(6-14), non-ITU 5(2-11), p<0·001, anxiety: ITU 12(5·5-19), non-ITU 7(2-14), p=0·002, PTSD: ITU 7(3·5-10), non-ITU 5(1-8), p=0·002), as shown in (Figure 4).
Figure 4: Depression, anxiety and PTSD scores for ITU and non-ITU workers during P3.
PTSD: Post Traumatic Stress Disorder, ITU: Intensive Therapy Unit, P3: Peak 3.
There was no significant difference in anxiety, depression, and PTSD scores between those who used wellbeing services and those who didn’t, those who were redeployed and those who weren’t and those who had opportunities to debrief compared to those who didn’t.
III Comparison of Peak 1 and Peak 3
In comparing the scores from P1 to P3, the following relationships were found between groups. Under 30-year-olds’ depression and PTSD scores increased from P1 to P3 (depression: P1 7(1-11), P3 8(3-14), p=0·048, PTSD: P1 4(0-7) P3 5(2-9), p=0·037), shown in (Figure 5).
Figure 5: Responders aged less than 30-years’ depression and PTSD scores during P1 and P3.
PTSD: Post Traumatic Stress Disorder, P1: Peak 1, P3: Peak 3.
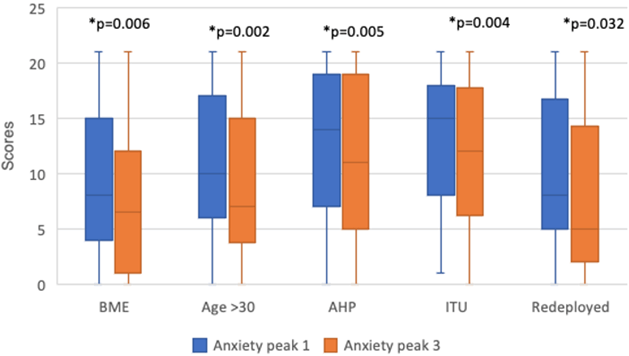
Several groups showed a decrease in anxiety scores from P1 to P3 including; over 30-years-olds (P1 10(5-17), P3 7(3-15) p=0·002), BME responders (P1 8(3·75-15) P3 6·5(1-12) p=0·006), AHP (P1 14(7-19), P3 11(5-19) p=0·005), ITU workers (P1 15(8-18·25) P3 12(5·75-18·25) p=0·004), and those who were redeployed (P1 8(5-18·25), P3 5(2-14·75), p=0·032), (Figure 6).
Figure 6: Anxiety scores in P1 and P3 for responder groups including BME, those aged over 30-years, AHP, ITU workers, those who were redeployed.
P1: Peak 1, P3: Peak 3, BME: Black and Minority Ethnic, AHP: Allied Health Professional, ITU: Intensive Therapy Unit.
IV Clinical Significance
During P1 50·3% of responders scores were clinically significant for anxiety, compared to 47·7% in P3. During P1 47.1% of responders scores were clinically significant for PTSD compared to 51·5% in P3.
V Difficult Factors
Of the factors that responders reported as finding most difficult, the factors that were most commonly reported in both peaks were as follows: poor staffing levels (49·7%), burden of work (47·8%), dealing with morally uncomfortable situations (42·7%), morale (35·7%), limited rest spaces (38·9%), care of a dying patient (31·8%), lacking senior support (30·6%).
Discussion
This retrospective cross-sectional study is the first to report mental health data focused on patient-facing HCWs in both the first and third peaks of COVID-19 in the UK. Our results showed the high burden of PTSD and depression symptoms seen in P1 (March to May 2020) to endure in P3 (December to February 2021). Anxiety symptoms, however, remained high but became less prevalent in P3, with the average level of anxiety no longer reaching clinical significance. This study indicates that the scale of the strain on the mental health of HCWs has largely continued in subsequent peaks of the pandemic, but that the pattern of impact is changeable. The scale of poor mental health in P3 demonstrates the need for additional measures to better support the wellbeing of HCWs.
In concordance with studies from P1 as well as those studying longitudinal change, women and AHPs suffered a greater burden of mental health symptoms again in P3 [14]. ITU staff were shown to be at higher risk during P3 than HCWs in other clinical areas, on average reaching clinically significant scores for depression, anxiety, and PTSD. The vulnerability of ITU staff has been demonstrated across P1, and its recurrence in P3 advocates for targeted support for ITU HCWs and risk stratification of HCW mental health by department and exposure to COVID-19 [21]. Not all previously identified risk and protective factors were demonstrated again in P3. Contrary to studies reporting on P1, redeployment had no effect on mental health in P3. As better workplace training prior to redeployment has been found to neutralise/reduce the impact on mental health in P1, perhaps the lack of negative effect of redeployment in P3 reflects that experience has been gained already through working in prior peaks of the pandemic [7]. The variable continuity of risk factors across the peaks reiterates the importance of continuing to study how and why the mental health of HCWs is impacted by subsequent COVID-19 peaks rather than relying on literature from P1 alone.
Greater improvement in mental health between P1 a was seen in our BME than the Caucasian population. Studies focused on P1 have tended to find either no effect or an increased risk of poor mental health in BME HCWs [22-24]. The greater drop in symptoms amongst BME HCWs might reflect alleviation of the stress on the BME community that resulted from disproportionate deaths of BME HCWs in P1, where initially two thirds of the HCWs who died were BME [25]. This study featured greater BME representation than most Trusts (50% in this study, 19% across NHS). The lower prevalence of mental health symptoms across both peaks in BME HCWs may also represent the protective effect of a more diverse environment, especially as greater social support has been previously identified as a strong protective factor in P1 [23, 26]. However, exploring the effect on diversity on the impact of COVID-19 on BME HCW mental health is beyond the scope of a single center study.
Further work is needed regarding the identification of HCW subsets which might be at risk for mental health to deteriorate even further in subsequent peaks of the pandemic. While anxiety symptoms were lower overall in P3, an increase was seen in under 30-year-olds. Initially, we felt this might be due to clinical inexperience, a previously identified risk factor in P1 [5, 10, 26]. However, as HCWs who had not worked in P1 were excluded from the study, the experience would have increased by P3. Further clarity regarding if this increase is more strongly associated with age or inexperience would require further studies measuring age and inexperience as separate variables. As this was the sole subset in which anxiety symptoms significantly increased with a later peak, institutions should work to implement greater workplace and wellbeing support for HCWs under 30-years-old should hospitalisations rise again moving forward.
Over half of the responders across both peaks did not feel enough was done institutionally to benefit staff wellbeing, only around 22% felt they had adequate access to services and just a third of those who did access wellbeing services found them to be beneficial. Additionally, no improvement in mental health symptoms was seen in P3 in those who did use mental wellbeing services (and the evidence that traditional wellbeing provision is a significant predictor of psychological resilience in the pandemic is uncertain). The reported feeling of insufficient provision in combination with our finding of low efficacy of existing wellbeing services indicates a need to shift the scale and form of wellbeing provisions offered, for example, providing employees with Psychological First Aid or coping strategies [20, 27]. As some literature has found resilient mental health in P1 to be associated with provision of mental health support, further studies delineating which forms of mental health services are most beneficial both in the first and subsequent peaks of the pandemic are needed [7, 26]. The consistency of the most reported difficult workplace factors across both peaks (primarily burden of work, moral injury, and poor staffing levels) suggests undertaking structural changes in addition to optimising wellbeing services would best protect the mental health of HCWs from further blows. Some factors might be more readily modifiable, such as the reduction of moral injury through access to an ethics panel [23]. This study’s demonstration of the enduring high prevalence of mental health symptoms across patient facing HCWs accompanied by inadequate institutional support should provide an impetus for healthcare institutions to bolster and adapt wellbeing support for their staff.
Strengths and Limitations
This study has many strengths. Primarily, capturing data focused on mental health symptoms in frontline HCWs during two critical points of the COVID-19 pandemic has not yet been done in Europe, making this study unique. By focusing on frontline HCWs only, the impact on those most at risk of poor mental health has been highlighted. Few studies exist looking at HCW mental health in P3 of the pandemic in the UK, and the ability of this study to then compare how P1 and P3 differed is a further asset. Assessing how HCW mental health progressed with peaks of COVID-19 informs the need for policy changes as well as for further research into subsequent peaks.
The greatest limitation of this study is the single-center design which may limit the generalisability of the study to other regions or countries, particularly the performance of wellbeing provision. Secondly, causality cannot be inferred due to the cross-sectional nature of the study. Thirdly, as data was collected for P1 and P3 but not the intervening time, we cannot be certain that P3 outcomes were associated with P3 rather than poor mental health outcomes remaining persistent throughout the pandemic.
Fourth is the potential for bias. The study’s retrospective design and survey-based approach open up the study to recall and selection bias respectively. The self-report nature of the survey also may introduce bias, though the PHQ-9, GAD-7, and TSQ are all validated as self-reporting screening tools. Fifth, by removing repetitive questions from the PHQ-9 for brevity and therefore acceptability, the ability to screen for the prevalence of clinically significant depression scores is limited, though the overall burden can still be approximated.
Conclusion
This study highlights an overall trend of a persistently high burden of mental health symptoms in frontline HCWs across two peaks of the COVID-19 pandemic in BHRUT. Working in ITU, being an AHP, and female gender were identified as risk factors for poor outcomes in P3. Younger age was a risk factor for worsening outcomes in P3 compared to P1. Wellbeing support was thought to be inadequate and was not associated with improved outcomes. These results demonstrate that poor mental health is an ongoing issue as peaks of the pandemic continue. The results could inform policy makers to make structural changes as well as further develop, expand, and target wellbeing provisions to improve the mental health of frontline HCWs during further peaks of hospitalisations. As we move forward in the pandemic, it is evident that the mental health of HCWs is at risk. We hope this data can contribute towards developing effective wellbeing services to support our workforce during this time, including who is particularly at risk and what issues are most pertinent to our staff.
Funding
None.
Ethical Approval
This project received HRA approval, REC number 21/HRA/1620.
Author Contributions
Eleanor Dorman - Conceptualisation, methodology, investigation, formal analysis, writing, review and editing; Zara Marcovic-Obiago - Conceptualisation, methodology, investigation, writing, review and editing; Julie Philips - Conceptualisation, methodology, investigation; Richard Szydlo - Formal analysis, review and editing; Darren Patten - Conceptualisation, methodology, investigation, review and editing.
Declaration
All authors declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Transparency Declaration
The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported, that no important aspects of the study have been omitted.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 02, Nov 2022Accepted: Mon 21, Nov 2022
Published: Fri 02, Dec 2022
Copyright
© 2023 Darren K. Patten. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.EJGM.2022.01.01
Author Info
Eleanor Dorman Zara Markovic-Obiago Julie Phillips Richard Szydlo Darren K. Patten
Corresponding Author
Darren K. PattenDepartment of General Surgery, Barking, Havering, and Redbridge University Trust, Queens Hospital, Rom Valley Way, Romford, UK
Figures & Tables
Table 1: Summary of responder demographics.
|
Demographic
|
|
n |
% |
|
Gender |
Female |
111 |
70·3 |
|
|
Male |
47 |
29·7 |
|
Age (y) |
≤30 |
41 |
25·9 |
|
|
31-40 |
45 |
28·5 |
|
|
41-50 |
38 |
24·1 |
|
|
51-60 |
26 |
16·5 |
|
|
≥61 |
8 |
5·1 |
|
Ethnicity |
BME |
79 |
50·0 |
|
|
White |
76 |
48·1 |
|
|
Prefer not to say |
3 |
1·9 |
|
Subgroups of BME |
Arab |
1 |
12·7 |
|
|
Asian or Asian British |
48 |
60·8 |
|
|
Black or Black British |
12 |
15·2 |
|
|
Mixed |
6 |
7·6 |
|
|
Other |
12 |
15·2 |
|
Job role |
Allied health professional |
104 |
65·8 |
|
|
Doctor |
54 |
34·2 |
|
Subgroups of AHP |
Nurse/ANP |
83 |
79·8 |
|
|
Therapist (OT/PT/SALT) |
10 |
9·6 |
|
|
HCA |
11 |
10·6 |
|
Subgroups of doctors |
Consultant |
9 |
16·7 |
|
|
Registrar |
13 |
24·1 |
|
|
Specialty training (pre-registrar) |
14 |
25·9 |
|
|
Foundation |
18 |
33·3 |
|
Area worked |
ITU both peaks |
58 |
36·7 |
|
|
Other area both peaks |
87 |
55·1 |
|
|
Mixed areas |
13 |
8·2 |
|
Redeployed |
Both peaks |
20 |
12·7 |
|
|
Neither peak |
102 |
64·6 |
|
|
Mixed redeployment |
36 |
22·8 |
AHP:
Allied Health Professional, BME: Black Minority Ethnicities, ANP: Advanced
Nurse Practitioner, OT: Occupational Therapist, PT: Physiotherapist, SALT:
Speech and Language Therapist, ITU: Intensive Therapy Unit.
Table 2: Summary of opinion regarding wellbeing services.
|
|
|
P1 |
P3 |
||
|
|
|
n |
% |
n |
% |
|
Staff opinion regarding access to wellbeing
services |
Sufficient |
34 |
22·4 |
34 |
21·5 |
|
Insufficient |
82 |
53·9 |
80 |
50·6 |
|
|
No difference |
36 |
23·7 |
44 |
27·8 |
|
|
Did staff use wellbeing services |
Yes |
35 |
22·2 |
26 |
16·5 |
|
No |
123 |
77·8 |
132 |
83·5 |
|
|
Of those who used wellbeing services,
staff opinion regarding whether they found this service useful |
Yes |
12 |
34·3 |
9 |
34·6 |
|
No |
12 |
34·3 |
9 |
34·6 |
|
|
No difference |
11 |
31·4 |
8 |
30·8 |
|

P3: Peak 3.

BME: Black and Minority Ethnic, P3: Peak 3.

P3: Peak 3, PTSD: Post Traumatic Stress Disorder.
PTSD: Post Traumatic Stress Disorder, ITU: Intensive Therapy Unit, P3: Peak 3.

PTSD: Post Traumatic Stress Disorder, P1: Peak 1, P3: Peak 3.
P1: Peak 1, P3: Peak 3, BME: Black and Minority Ethnic, AHP: Allied Health Professional, ITU: Intensive Therapy Unit.
References
1.
UK Government
Coronavirus (COVID-19) in the UK. Deaths in United Kingdom.
2.
UK Government
Coronavirus (COVID-19) in the UK. Cases in United Kingdom.
3.
UK Government
Coronavirus (COVID-19) in the UK. Healthcare in United Kingdom.
4.
Salari N, Khazaie
H, Far AH, Paveh BK, Kazeminia M et al. (2020) The prevalence of stress,
anxiety and depression within front-line healthcare workers caring for COVID-19
patients: A systematic review and meta-regression. Hum Resour Health 18:
100. [Crossref]
5.
Muller AE, Hafstad
EV, Himmels JPW, Smedslund G, Flottorp S et al. (2020) The mental health impact
of the covid-19 pandemic on healthcare workers, and interventions to help them:
A rapid systematic review. Psychiatry Res 293: 113441. [Crossref]
6.
Wanigasooriya K,
Palimar P, Naumann DN, Ismail K, Fellows JL et al. (2021) Mental health
symptoms in a cohort of hospital healthcare workers following the first peak of
the COVID-19 pandemic in the UK. BJPsych Open 7: e24. [Crossref]
7.
Khajuria A,
Tomaszewski W, Liu Z, Chen Jh, Mehdian R et al. (2021) Workplace factors
associated with mental health of healthcare workers during the COVID-19
pandemic: An international cross-sectional study. BMC Health Serv Res
21: 262.
8.
Vizheh M, Qorbani
M, Arzaghi SM, Muhidin S, Javanmard Z et al. (2020) The mental health of
healthcare workers in the COVID-19 pandemic: A systematic review. J Diabetes
Metab Disord 19: 1967-1978. [Crossref]
9.
Danet AD (2021)
Psychological impact of COVID-19 pandemic in western frontline healthcare
professionals. A systematic review. Med Clin (Barc) 156: 449-458. [Crossref]
10.
Kisely S, Warren N,
McMahon L, Dalais C, Henry I et al. (2020) Occurrence, prevention, and
management of the psychological effects of emerging virus outbreaks on
healthcare workers: Rapid review and meta-analysis. BMJ 369: m1642. [Crossref]
11.
Tuan NQ, Phuong ND,
Co DX, Son DN, Chinh LQ et al. (2021) Prevalence and Factors Associated with
Psychological Problems of Healthcare Workforce in Vietnam: Findings from
COVID-19 Hotspots in the National Second Wave. Healthcare (Basel) 9:
718. [Crossref]
12.
Dufour MM, Bergeron
N, Rabasa A, Guay S, Geoffrion S (2021) Assessment of Psychological Distress in
Health-care Workers during and after the First Wave of COVID-19: A Canadian
Longitudinal Study: Évaluation de la Détresse Psychologique Chez Les
Travailleurs de la Santé Durant et Après la Première Vague de la COVID-19: une
étude longitudinale canadienne. Can J Psychiatry 66: 807-814. [Crossref]
13.
Rossi R, Socci V,
Jannini TB, Pacitti F, Siracusano F et al. (2021) Mental Health Outcomes Among
Italian Health Care Workers During the COVID-19 Pandemic. JAMA Netw Open
4: e2136143. [Crossref]
14.
Vanhaecht K, Seys
D, Bruyneel L, Cox B, Kaesemans G et al. (2021) COVID-19 is having a
destructive impact on health-care workers' mental well-being. Int J Qual
Health Care 33: mzaa158. [Crossref]
15.
Steinmetz LCL,
Herrera CR, Fong SB, Godoy JC (2021) Changes in Healthcare Workers' Anxiety
During Two Time Points of the COVID-19 Pandemic: Evidence From a Longitudinal
Study. Int J Ment Health Addict 1-15. [Crossref]
16.
Steenkiste EV,
Schoofs J, Gilis S, Messiaen P (2021) Mental health impact of COVID-19 in
frontline healthcare workers in a belgian tertiary care hospital: A prospective
longitudinal study. Acta Clin Belg 77: 533-540. [Crossref]
17.
Zhou Y, Ding H,
Zhang Y, Zhang B, Guo Y et al. (2021) Prevalence of poor psychiatric status and
sleep quality among frontline healthcare workers during and after the COVID-19
outbreak: A longitudinal study. Transl Psychiatry 11: 223. [Crossref]
18.
Vagni M, Maiorano
T, Giostra V, Pajardi D (2021) Protective Factors against Emergency Stress and
Burnout in Healthcare and Emergency Workers during Second Wave of COVID-19. Soc
Sci 10.
19.
Sasaki N, Kuroda R,
Tsuno K, Imamura K, Kawakami N (2022) COVID-19 vaccination did not improve
employee mental health: A prospective study in an early phase of vaccination in
Japan. Neuropsychopharmacol Rep 42: 230-232. [Crossref]
20.
McFadden P, Neill
RD, Moriarty J, Gillen P, Mallett J et al. (2021) A Cross-Sectional Examination
of the Mental Wellbeing, Coping and Quality of Working Life in Health and
Social Care Workers in the UK at Two Time Points of the COVID-19 Pandemic. Epidemiologia
2: 227-242.
21.
Greenberg N, Weston
D, Hall C, Caulfield T, Williamson V et al. (2021) Mental health of staff
working in intensive care during Covid-19. Occup Med (Lond) 71: 62-67. [Crossref]
22.
Greene T, Seppänen
JH, Adeniji M, Steel C, Grey N et al. (2021) Predictors and rates of PTSD,
depression and anxiety in UK frontline health and social care workers during
COVID-19. Eur J Psychotraumatol 12: 1882781. [Crossref]
23.
Gilleen J,
Santaolalla A, Valdearenas L, Salice C, Fusté M (2021) Impact of the COVID-19
pandemic on the mental health and well-being of UK healthcare workers. BJPsych
Open 7: e88. [Crossref]
24.
Feingold JH,
Hurtado A, Feder A, Peccoralo L, Southwick SM et al. (2022) Posttraumatic
growth among health care workers on the frontlines of the COVID-19 pandemic. J
Affect Disord 296: 35-40. [Crossref]
25.
Rimmer A (2020)
Covid-19: Two thirds of healthcare workers who have died were from ethnic
minorities. BMJ 369: m1621. [Crossref]
26. Uphoff EP, Lombardo C, Johnston G, Weeks L, Rodgers M et al. (2021) Mental health among healthcare workers and other vulnerable groups during the COVID-19 pandemic and other coronavirus outbreaks: A rapid systematic review. PloS One 16: e0254821. [Crossref]
27. Asaoka H, Koido Y, Kawashima Y, Ikeda M, Miyamoto Y et al. (2021) Longitudinal Change of Psychological Distress among Healthcare Professionals with and without Psychological First Aid Training Experience during the COVID-19 Pandemic. Int J Environ Res Public Health 18: 12474. [Crossref]
