Use of Virtual Reality as a Distraction Technique to Limit Opiate Use in Traumatic and Surgical Wound Dressing Management
A B S T R A C T
Background: Chronic opiate use in traumatic and surgical wound management has become an increasingly controversial topic nationally. Here we present a case of a large surgical wound previously managed with operative dressing changes with significant opiate use for pain control with the use of virtual reality at the time of dressing changes to decrease opiate use as well as operative need; and therefore, overall cost.
Case Presentation: The patient is a 57-year-old female with morbid obesity and poorly controlled diabetes mellitus who presented with a necrotizing soft tissue infection of the left thigh. She was admitted to the intensive care unit, initiated on broad spectrum antibiotics, and taken to the operating room for excisional debridement. After stabilization and source control, the patient continued to require operative incisional wound vac changes every other day despite maximal multimodal pain therapy. After discussion with the patient regarding her continued ongoing operative wound vac changes and her desire to progress care, the team attempted a bedside dressing change utilizing the Facebook Oculus Quest Virtual Reality device application “Nature Treks VR”. The patient endorsed reduced pain scores during the dressing change and endorsed emersion into the virtual world throughout the dressing change.
Conclusion: To the best of our knowledge this is the first reported incidence of using a virtual reality platform to reduce opiate use, operative need, progression of care, and overall cost in a patient with a large, debilitating operative wound outside of the burn population. Advances in virtual reality hardware including tether less systems like Oculus Quest, non-controller hand tracking and headset sanitation devices have reduced barriers to introducing virtual reality therapy into the clinic and ICU. A prospective study is needed to validate the use of virtual reality as a distraction therapy at the time of dressing changes. Future use of virtual reality may involve reducing ICU delirium, targeted pain management, post trauma recovery exercises and enhanced rehabilitation of amputees with prosthetic devices.
Keywords
Virtual reality, dressing changes, pain management, conscious sedation
Background
According to the Centers for Disease Control (CDC), opiate abuse has become a health emergency in the United States [1]. Practitioners as well as hospital systems are increasingly under pressure to maximize patient satisfaction while minimizing the use of potentially harmful and addicting pain medications. Opiate use has an important role to play in managing pain during the treatment of traumatic or surgical wounds; however, opiate use leads to many unwanted side effects including nausea, constipation, diminishing effect requiring increasing dosing, and, eventually, physical dependence. The advent of virtual reality has been a proven distraction therapy in reducing opiate needs as well as anxiety at the time of dressing changes in the burn injury population [2-4]. To date, there has not been a study examining the use of virtual reality as a distraction technique in patients with more common traumatic and surgical wounds that frequently require numerous operative dressing changes outside of the burn population. As virtual reality continues to improve, becomes more accessible, and more immersive, there is an opportunity to utilize its technology broadly to decrease opiate use, decrease anxiety, improve functional status sooner, increase patient satisfaction, decrease cost, and improve overall outcomes.
Case Report
The patient is a 57 year-old female with a past medical history significant for morbid obesity (BMI 40 kg/m2), poorly controlled type 2 diabetes mellitus (HgbA1c 11.4), hypertension, as well as a failed left ankle arthrodesis status post left below the knee amputation (1998) complicated by phantom limb pain (on Duloxetine and diclofenac) who presented with a necrotizing soft tissue infection of the left thigh, perineum, and left labia. On presentation, the patient was tachycardic (112 bpm), normotensive (129/88), and afebrile (36.7o C) with a lactic acidosis (3.3), hyponatremia (128), and profound hyperglycemia (471). Resuscitation was initiated, she was placed on broad spectrum antibiotics, and the patient was taken to the operating room emergently for incision, drainage, and debridement. Post-operatively, the patient was brought to the surgical intensive care unit for ongoing resuscitation, glycemic control, and monitoring.
The patient returned to the operating room for source control twice with final wound dimensions measuring 28 x 37 x 5 cm. Wound cultures ultimately grew Group B Streptococcus Agalactiae and the patient completed a course of antibiotics. The patient was placed on a multimodal pain regimen including scheduled Tylenol, lidocaine patches, Ibuprofen, Pregabalin, as needed intravenous Dilaudid, and as needed oral Dilaudid/Oxycodone. Despite maximizing pain control measures, the patient required 120 mg of morphine equivalent opiate dosing per day. Unfortunately, despite these pain control measures, the patient would not tolerate a bedside wound vac dressing change and required the operating theater for dressing changes an additional eight instances. In addition, the patient underwent a diverting colostomy to divert stool from the wound. The patient’s last operative need was on hospital day 29.
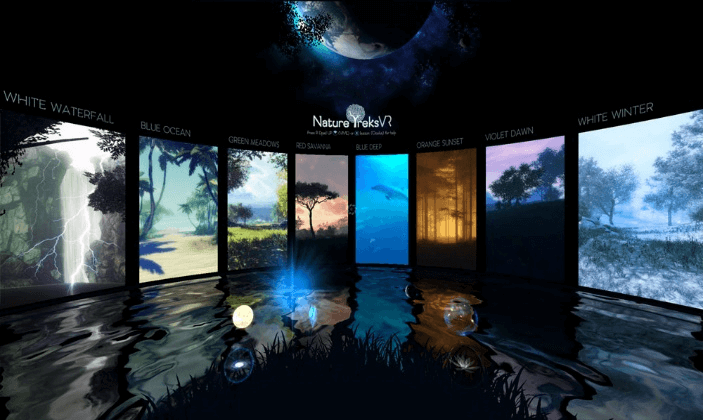
After discussion with the patient, the patient decided to use a virtual reality headset as a tool to initiate bedside dressing changes in an effort to transition to the next level of care. After discussing the risks and benefits of bedside dressing changes with the patient and allowing her time to trial the virtual reality headset, the patient consented to a bedside dressing change. On the day of the dressing change, the patient was premedicated with 5 mg oral oxycodone and 0.5 mg oral Lorazepam approximately 45 minutes prior to the dressing change. The virtual reality headset was then placed onto the patient (Figure 1). The team chose the application “Nature Treks VR” on the Facebook Oculus Quest device (Figure 2). The application placed the patient on a tropical beach overlooking the ocean and palm trees. The patient then underwent the bedside wound vac exchange over the next 20 minutes. After the dressing change was complete, the patient was asked a series of questions to examine her immersion in the virtual reality world as well as her perceived pain during the dressing change.
Figure 1: Oculus Quest- All-in-One VR headset.
Figure 2: Nature Treks Environment- offers 9 breathtaking VR environments with VR choices ranging from tropical beaches, nature, underwater oceans, exploring the stars and more.
The following questions along a scale from 1-10 were assessed:
i. How much fun did you have during VR therapy? (3/10 – Mildly fun (1-4)).
ii. To what extent at all did you feel “nausea” during VR therapy? (1/10 – Mild nausea (1-4)).
iii. While experiencing the virtual world, to what extent did you feel like you “went inside” the computer-generated world? (6/10 – Moderate sense of going inside (5-6)).
iv. How much time did you spending thinking about your pain? (5/10 – Half of the time (5)).
v. Rate your worst pain during the dressing change (7/10 – Severe pain (7-9)).
vi. How “unpleasant” was your pain during VR therapy? (4/10 – Mildly unpleasant (1-4)).
The patient continued with bedside dressing changes and was eventually discharged to a skilled nursing facility on hospital day 43.
Discussion
The patient described in the above case is not unlike the patients that many Acute Care surgeons encounter. Given the paucity of operating room space for Acute Care surgeons, an increasing necessity for rapid turnover of operative rooms, and an expansion of elective surgical practice, many institutions are unable to accommodate operative dressing changes during the day. As such, our patients often spend the entirety of their day NPO on call to the operating room only for their case to be cancelled by more emergent surgeries. Since nutrition is an enormous component to wound healing, offering early bedside dressing changes without the need for compromising nutritional status is paramount.
In addition to potentially improving nutrition status and, thereby, wound healing, there is a cost savings for the patient when performing bedside dressing changes. In our institution alone, a 45-minute operative wound vac dressing change bills approximately 6500 dollars compared with just 300 dollars for wound vac supplies if the dressing is changed at the bedside. The use of virtual reality at the time of dressing changes as a distraction therapy also provides the advantage of decreased opiate use prior to, during, and after the dressing change. In the patient described above, her total opiate need decreased from 120 mg of morphine equivalent to 5 mg Oxycodone and 0.5 mg Ativan given prior to the dressing change. The reduction of opiate use at the time of the dressing change as well as the perceived reduction of pain scores during virtual reality therapy are promising. It is well documented in the literature that large traumatic wounds requiring months of opiate therapy lead to a significantly increased risk of opiate dependence, addiction, and tolerance.
Furthermore, with hospitals under increasing pressure to maintain occupancy and limited rehabilitation centers across the country, it is paramount to facilitate the progression of care from the acute phase to the rehabilitation phase in an expedited fashion. With the need for operative dressing changes, the patient’s hospital course can often be weeks, if not, months long. The early implementation of virtual reality therapy leading to an earlier transition to bedside dressing changes can be a tool to progress care, decrease hospital length of stay, and further complications. Opportunity exists to develop virtual reality environments better suited to the clinic. Gaze based controls offer interactivity and additional immersion for users unable to manipulate handheld controllers. Advances in pupillary tracking offer additional opportunity for virtual reality interactivity to patients. Virtual environments should also be designed to accommodate patient placement (e.g. Reclining, seated, laying on side).
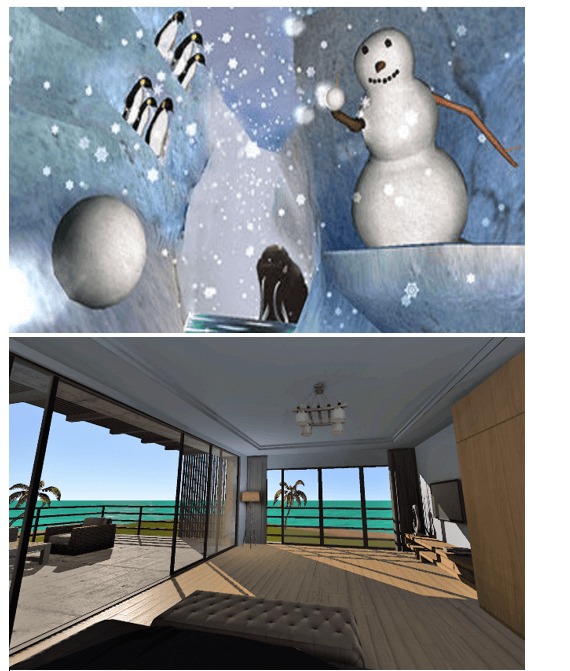
Additionally, attention should be given to high quality virtual environments (Figure 3). Virtual reality therapies are most effective when they incorporate game-like elements to promote engagement and immersion, and less likely to produce side effects like dizziness or nausea when they include game industry standard frame rates, high quality environments, textures and lighting [5]. To the best of our knowledge this is the first use of virtual reality platforms as a method of distraction in order to progress patient care, decrease operative need, opiate use, and overall patient cost in large surgical wound care patients outside of the burn population. A prospective study is needed to validate the use of virtual reality as a distraction therapy at the time of dressing changes. Future use of virtual reality may involve reducing ICU delirium, targeted pain management, post trauma recovery exercises and enhanced rehabilitation of amputees with prosthetic devices.
Figure 3: Screenshots from existing clinical virtual reality environments: Snow World (left), an environment designed for burn wound care, and an unreleased ICU and inpatient environment (right) developed by SuperGenix featuring gaze-based interactions, high quality graphics, lighting effects and day/night cycles.
Article Info
Article Type
Case ReportPublication history
Received: Sat 30, May 2020Accepted: Thu 11, Jun 2020
Published: Wed 24, Jun 2020
Copyright
© 2023 Albert Chi. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2020.02.12
Author Info
Albert Chi Julius Jockusch Michael Long Peter Lund Scott Sherry
Corresponding Author
Albert ChiDivision of Trauma, Critical Care & Acute Care Surgery Department of Surgery, Oregon Health and Science University Portland, Oregon, USA
Figures & Tables

References
- Centers for Disease Control and Prevention (2018) 2018 Annual Surveillance Report of Drug-Related Risks and Outcomes-United States. Surveillance Special Report 2pdf icon. Centers for Disease Control and Prevention, U.S. Depart Health Human Ser.
- Maani CV, Hoffman HG, Morrow M, Maiers A, Gaylord K et al. (2011) Virtual Reality Pain Control During Wound Debridement of Combat-Related Burn Injuries Using Robot-like Arm Mounted VR Goggles. J Trauma 71: S125-S130. [Crossref]
- Sharar SR, Miller W, Teeley A, Soltani M, Hoffman HG et al. (2008) Applications of Virtual Reality for Pain Management in Burn-Injured Patients. Expert Rev Neurother 8: 1667-1674. [Crossref]
- Morris LD, Louw QA, Grimmer Somers K (2009) The Effectiveness of Virtual Reality on Reducing Pain and Anxiety in Burn Injury Patients: A Systematic Review. Clin J Pain 25: 815-826. [Crossref]
- Karamians R, Proffitt R, Kline D, Gauthier LV (2017) Effectiveness of Virtual Reality- and Gaming-Based Interventions for Upper Extremity Rehabilitation Poststroke: A Meta-analysis. Arch Phys Med Rehabil 101: 885-896. [Crossref]
