Ultrasonographic Diagnosis of Left-sided Ovarian Torsion in a Twin Pregnancy at 24 weeks: A Case-Report
A B S T R A C T
We describe a case report of ovarian torsion in a Korean-speaking woman with a 24-week twin pregnancy who attended a Spanish- and English-speaking institution. Ovarian torsion represents a diagnostic challenge for clinicians and radiologists because of its lack of pathognomonic symptoms and imaging findings. Ultrasonography may show unilateral ovarian enlargement without color Doppler flow and free fluid; however, clinical data should be mandatory for management decisions.
Keywords
Torsion, ovarian, abdominal pain, ultrasound, diagnostic imaging, pregnancies, twin
Introduction
Ovarian torsion (OT) is the fifth most common cause of gynaecological emergency surgery affecting 2.7% of women, and it is seen in 6/10,000 of pregnant women, usually at early pregnancy with a right-sided predilection [1]. Timely diagnosis is of utmost importance because it can lead to ischaemia and infertility. Imaging assessment is mandatory due to non-specific presentation. Literature reports several cases of OT during pregnancy, but there are only few reports of left-sided OT at third trimester twin pregnancy [2]. This is a case of diagnosis and management of a left OT in a twin pregnancy of a woman with a communication barrier due to different language speaking, with normal term delivery.
Case Report
A 32-year-old Korean woman, primigravida, with a twin pregnancy at 24 weeks and adequate prenatal control, admitted to the emergency department (ED) with sudden severe pain in the left renal fossa irradiated to ipsilateral iliac fossa. As an important context, the Korean-speaking patient presented to our institution in Northeastern Mexico, where the emergency and radiology staff spoke only Spanish and English, making clinical data difficult to obtain, with the use of electronic translators. Physical examination showed no palpable uterine activity, longitudinal products, normal fetal heart-beats and pain on palpation in left iliac fossa; laboratory findings revealed mild neutrophilia. Vital signs were normal.
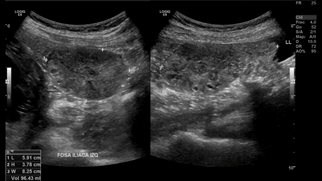
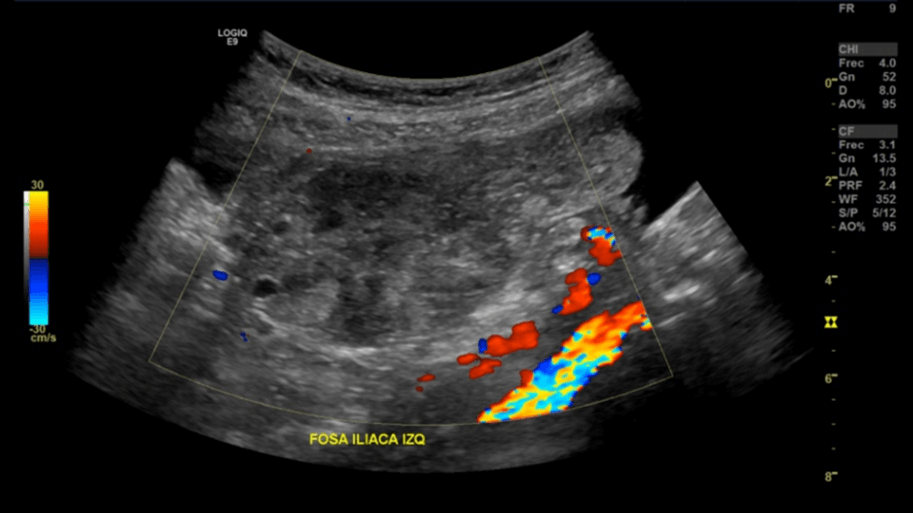
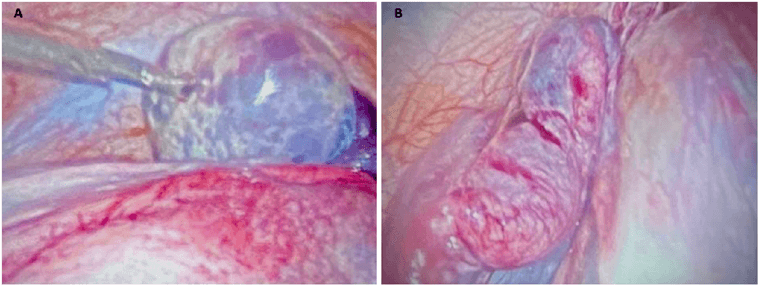
An obstetric US was requested by ED. Obstetric US was performed with 1-6 MHz convex transducer (LOGIQ E9, GE Healthcare), documenting a normal dichorionic diamniotic twin pregnancy with normal heart-beats of twin 1 and twin 2. Intentional tracking was performed at the pain site, where enlarged left ovary was identified, with heterogeneous echotexture and free fluid (Figure 1). No Doppler colour flow was documented (Figure 2). Right ovary was normal. These findings were indicators of ovarian torsion with suggestive data of ischaemia. Findings were confirmed with magnetic resonance imaging (MRI) (Optima™ MR450w GEM 1.5T, GE Healthcare) (Figure 3). Laparoscopic surgical approach was performed (Figure 4) where the left ovary was identified with congestive, edematous and violaceous salpinx, suggestive of ischaemia, with three turns on its axis in relation to the salpinx. Ovary was released from torsion and its normal position was reestablished until adnexal revascularization was observed with restoration of colour and morphology. The patient was discharged asymptomatic 60 hours later. Currently the patient is healthy, she reports having given birth to her twins without associated complications.
Figure 1: Gray scale US shows enlarged left ovary, with a volume of 96 ml and heterogenous echotexture and free fluid surrounding upper and lower poles.
Figure 2: Color Doppler assessment revealed no ovary flow. These findings were compatible with ovarian torsion and suggestive data of ischaemia.
Figure 3: Coronal MRI slices A) show both products of normal gestation. Axial fat-saturated T2-weighted slices, B) revealed enlarged left ovary with edema and free fluid. `
Figure 4: A) Edema and violaceous colouration of the left ovary, B) as well as congestive changes of the salpinx at the moment of operative laparoscopy.
Discussion
OT is an axial twist of at least one turn of the adnexa, ovary or the tube, causing compromise of lymphatic and venous outflow and arterial inflow, leading to edema, ischaemia and necrosis. 71% of cases of OT correspond to the right ovary and 21% to the left. This may be explained because the right utero-ovarian ligament is longer, and the presence of the sigmoid colon in the left pelvis leaves less space for the torsion to take place [3].
This case of abdominal pain in a pregnant woman was a clinical and radiologic challenge due to the language barrier, taking into account that correct diagnosis of OT prior to surgery has been reported only in 23-66% of cases. Upon receiving our patient in US room, obstetric complications were the first causes of pain we tried to rule out. After documenting normal pregnancy findings, left iliac fossa pain during US exploration lifted the suspicion of ovarian pathology. OT has been shown to be more common in pregnancy (28%) than in a non-pregnant patient (7%) [4]. Diagnosis requires integration of clinical and imaging findings. US is one of the most accessible and fastest modalities that provides 70% sensitivity and 87% specificity. Presence of a mass/cyst, unilateral ovarian enlargement, ovarian edema, peripheral location of the follicles, an anechoic halo around the ovary due to hemorrhage, free fluid and the use of Color Doppler can suggest OT. Persistence of adnexal vascularization does not exclude torsion, in fact, normal Doppler features are described in 60% of cases [5]. This is why surgical intervention should not be based exclusively on images [6]. In our patient, a frank increase in the dimensions and heterogeneous aspect of the left ovary, total absence of Color Doppler flow, free fluid and pain at the time of US exploration of this site were observed, so that, despite the language barrier, the integration of these findings was highly suggestive of OT with ischaemia data.
Obstetrician requested an MRI without intravenous (IV) contrast. MRI does not expose the fetus or mother to ionizing radiation, however, it could slightly increase the heat in the imaged subject. IV contrast should be avoided because gadolinium-based contrast agents cross the placenta [7]. MRI shows an accuracy greater than 80% for OT in the context of acute pelvic pain [8]. In the specific case of our patient, due to the difficulty in obtaining solid clinical data on interrogation, US played an important role in the diagnosis of OT, complemented with MRI, to rule out differentials. Laparoscopic confirmation and management were made.
Why Should OT Diagnosis be Important for the Radiologist?
A correct and timely diagnosis is crucial for OT, as it means that ovarian viability, and therefore fertility, may be affected. Since US remains the initial method of addressing acute pelvic pain during pregnancy, radiologists must be able to recognize findings that support this diagnosis. Ultimately, this diagnostic challenge must be addressed through multidisciplinary management and active communication between emergency physicians, obstetricians and radiologists.
Protection of Humans and Animals
The authors declare that no experiments on humans or animals have been performed for this research.
Confidentiality of Data
The authors declare that they have followed their center's protocols on the publication of patient data.
Right to Privacy and Informed Consent
The authors declare that no patient data appear in this article.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Sat 05, Nov 2022Accepted: Mon 21, Nov 2022
Published: Wed 30, Nov 2022
Copyright
© 2023 Samuel Isaí López-Martínez. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CROGR.2022.02.01
Author Info
Samuel Isaí López-Martínez Jesús Gerardo Sánchez-Valadez María Andrea Tijerina-Torres Rodrigo Melendez-Coral Javier Jesús Onofre-Castillo
Corresponding Author
Samuel Isaí López-MartínezRadiology Resident, Christus Muguerza Hospital Alta Especialidad, Monterrey, Nuevo León, México
Figures & Tables

References
1. Pan HS, Huang LW,
Lee CY, Hwang JL, Chang JZ (2004) Ovarian pregnancy torsion. Arch Gynecol
Obstet 270: 119-121. [Crossref]
2. Bernigaud O,
Fraison E, Thiberville G, Lamblin G (2021) Ovarian torsion in a twin pregnancy
at 32 weeks and 6 days: A case-report. J Gynecol Obstet Hum Reprod 50:
102117. [Crossref]
3. Huchon C,
Fauconnier A (2010) Adnexal torsion: a literature review. Eur J Obstet
Gynecol Reprod Biol 150: 8-12. [Crossref]
4. Parikh B, Hussain
FN, Brustman L (2019) Acute Abdomen in Pregnancy. Topics Obstet Gynecol
39: 1-7.
5. Ssi Yan Kai G,
Rivain AL, Trichot C, Morcelet MC, Prevot S, Deffieux X et al. (2018) What
every radiologist should know about adnexal torsion. Emerg Radiol 25:
51-59. [Crossref]
6. Grunau GL, Harris
A, Buckley J, Todd NJ (2018) Diagnosis of Ovarian Torsion: Is It Time to Forget
About Doppler? J Obstet Gynaecol Can 40: 871-875. [Crossref]
7. Moreno CC, Alexander LF, Sharma P, Mittal PK (2017) MRI Evaluation of Pregnant Women Presenting With Acute Abdominal Pain. Contemporary Diagnostic Radiol 40: 1-7.
8. Li C, Wang S, Tao X, Hu Y, Li X et al. (2018) Torsion of normal-sized ovary during late pregnancy: A case report and review of the literature: Torsion of normal ovary in pregnancy. J Obstet Gynaecol Res 44: 2110-2114. [Crossref]
