Treatment of Nodular Fasciitis on the Front Surface of the Neck
A B S T R A C T
Nodular fasciitis (NF) is a benign reactive or inflammatory condition of mesenchymal fibroblasts. Rapid growth and histological features make nodular fasciitis a mimicker of malignancies such as sarcomas, however, nodular fasciitis is a benign lesion and does not metastasize. Although the etiology of nodular fasciitis is uncertain, histopathologically, it bears a close resemblance to organizing granulation tissue, and myofibroblastic proliferation may be initiated by a local injury or local inflammatory process, which supports a reactive proliferation theory triggered by trauma. Surgical excision is recommended for diagnosis and treatment to exclude malignancy. We are hereby reporting a case of nodular fasciitis on the front surface of the neck, 86 years old patient. Tumor grew rapidly and reached 9-10 cm., and which was clinically suspected as a malignancy located. An ultrasound examination was performed. Based on the clinical and ultrasound data, it was decided to perform an extended biopsy to establish the final diagnosis it. Tumor has been removed as a solid mass. The material was sent for histopathological examination. Based on the history, clinical picture, and histopathological examination, the lesion was diagnosed as nodular fasciitis. After surgery patient expressed satisfaction with the result of treatment. In cases of nodular fasciitis, proactive efforts are needed to perform histopathologic evaluation and treatment because nodular fasciitis tends to grow rapidly.
Keywords
Nodular fasciitis, benign tumors, proliferative soft tissue lesion, surgical excision
Introduction
Nodular fasciitis (NF) is a benign proliferative myofibroblastic reactive soft tissue lesion that may regress spontaneously and being mistaken for a sarcoma [1]. In 1955, Konwaler and associates published the first formal description of nodular fasciitis, naming it as subcutaneous pseudosarcomatous fibromatosis [2]. Lesions are typically solitary, well-defined but unencapsulated, and undergo rapid enlargement. However, nodular fasciitis is a benign lesion and does not metastasize. Nodular fasciitis should be considered in the differential diagnosis of tumors for an accurate diagnosis and timely treatment. Nodular fasciitis has to be differentiated from schwannoma, myofibroma, solitary fibrous tumor, fibrosarcoma, leiomyosarcoma, neurofibroma and malignant fibrous histiocytoma [3-5].
The etiology of nodular fasciitis is unknown. Nodular fasciitis can be distinguished from these based on histopathological examination, molecular biology, and immunohistochemistry [6, 7]. Although the etiology of nodular fasciitis is uncertain, histopathologically, it bears a close resemblance to organizing granulation tissue, and myofibroblastic proliferation may be initiated by a local injury or local inflammatory process, which supports a reactive proliferation theory triggered by trauma. The myofibroblast is thought to be the cell of origin [8-10]. The most common sites noted are the upper extremities (48%), trunk (20%), head and neck (15-20%), and lower extremities (15%). There are three types of NF depending on their location: subcutaneous, intramuscular, and intermuscular (fascial) [11]. The subcutaneous form is most common, followed by the fascial form, with the intra-muscular form being the least common. In adults, the upper extremities are the most commonly affected site [12].
There is no standard treatment for nodular fasciitis, treatment options for nodular fasciitis depend in part on the size and location of the tumor. Treatment is usually surgical excision; however, large infiltrative lesions may be difficult to manage. Surgical excision is recommended for diagnosis and treatment to exclude malignancy. Laser treatment can be effective in decreasing the size of the lesions through tissue contraction. A carbon dioxide (CO2) laser used in a pinhole pattern is a treatment option for tumors on the face or another area [13]. For the nonsurgical treatment of nodular fasciitis on the face, triamcinolone intralesional injection (TA ILI) can be used on the basis of the fact that, nodular fasciitis is a benign reactive or inflammatory condition of mesenchymal fibroblasts [14]. If the nodular fasciitis is large or on the face, a corticosteroid injection at the site may help resolve the tumor. We describe a case of nodular fasciitis on the front surface neck that demonstrated partial spontaneous regression and treated by using surgical method.
Case Report
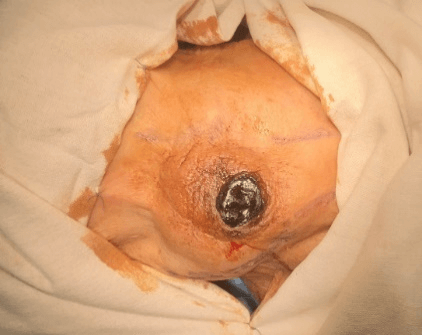
Patient, 86 years old, was taken to the Dept. of Oral and Maxillofacial Surgery of 1-st Yerevan State University Hospital Complex “Heratsi” by an ambulance team on 09.08.2018, with complaints of bleeding from the neoplasm located on the front surface of the neck. According to the patient, the tumor first noticed about 3-4 months ago. Tumor grew rapidly and reached 9-10 cm. History indicated the thyroid gland disease, about which the patient took a medication every day (presumably euthyrox). During external examination, a palpable dense consistency neoplasm was observed, covered with a dense hemorrhagic crust about 2-3 cm, blackish in color (Figure 1). There was a slight bleeding from the periphery, the blood was dark, stagnant. During palpation, the tumor was painless, partially moveable. The color of the overlying skin was not changed, with the underlying tissues not soldered. Submandibular lymph nodes were not palpated.
Figure 1: Clinical examination revealed dense consistency neoplasm, covered with a dense hemorrhagic crust about 2-3 cm, blackish in color.
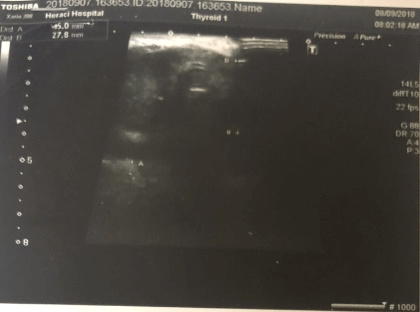
An ultrasound examination was performed, on the basis of which it was revealed that the thyroid gland is diffusely altered, there are nodes in the right lobe of the thyroid gland. In the area of the right lobe of the thyroid gland, a massive heterogeneous well vascularized neoplazm of about 10–13 cm was found with clear boundaries, located extracapsularly (Figures 2 & 3). Based on the above clinical and ultrasound data, it was decided to perform an extended biopsy to establish the final diagnosis. During the preoperative examinations of the associated diseases, a diffuse nodular goiter, chronic heart failure of the II-degree, chronic obstructive pulmonary disease, and asthma was detected. Only after the general somatic stabilization of the patient was an operation planned.
Figure 2 & 3: An ultrasound examination in the area of the right lobe of the thyroid gland, a massive heterogeneous well vascularized neoplasm of about 10-13 cm was found with clear boundaries, located extracapsularly.
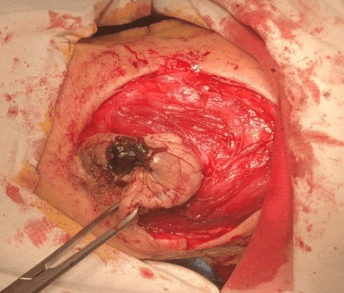
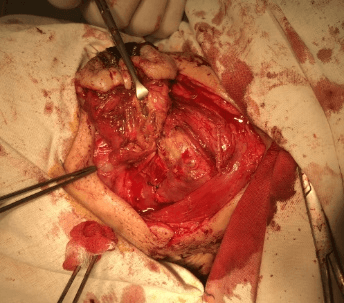
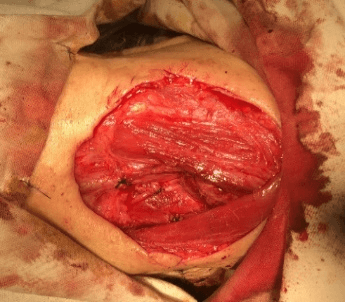
Figure 4, 5 & 6: Nodular lesion was surgically removed under general anesthesia. Intraoperative view of the excision of the of the nodular fasciitis on the front surface of the neck.
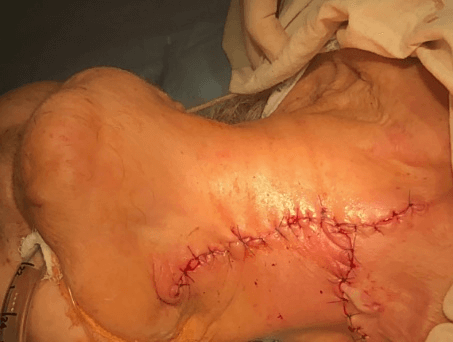
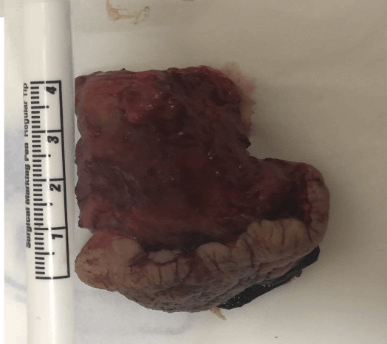
On 09.11.2018, under general anesthesia, an operation was performed – an extended biopsy. A skin incision was made, bordering the neoplasm, and retreating from the palpable tumor boundaries by 2 cm. A skin flap was cut, including a hemorrhagic crust. In a blunt way, the tumor was mobilized and exfoliated from the surrounding tissues. All the vessels involved were ligated and hemostasis was achieved. Tumor has been removed as a solid mass. After antiseptic preparation, hemostatsis was achieved and, the wound was sutured layer by layer (Figures 4-8). The material was sent for histopathological examination. Macroscopically: there was 4,0x4,0x2,5 cm dense consistency neoplasm, with smooth whitish edges. In the section there was a cavity which extended from the skin to the base of the neoplasm, filled with a homogeneous pink mass, with the presence of the surrounding yellow-whitish tissues.
Figure 7: Clinical appearance after removal of nodular fasciitis.
Figure 8: Nodular lesion after being surgically removed: there was 4,0x4,0x2,5 cm dense consistency.
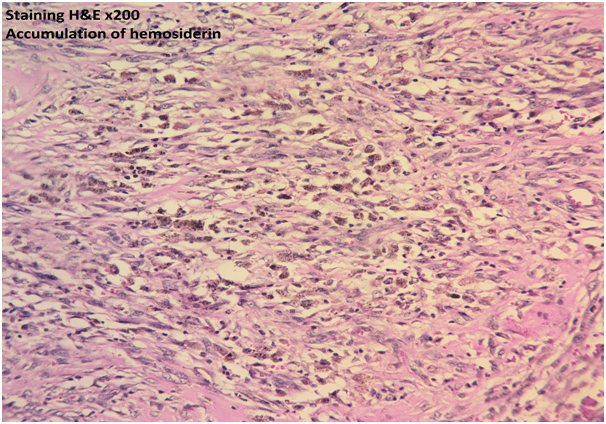
Figure 9: Accumulation of hemosiderein.
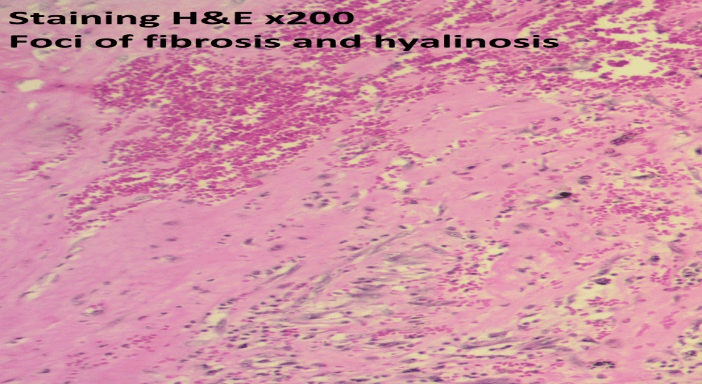
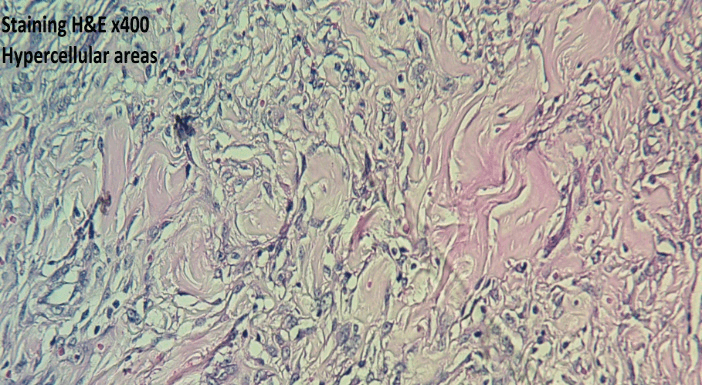
Microscopically: peripheral hypercellular zones were observed on sections, with S and C shape solid areas of rounded and elongated moderately pleomorphic cells located in different directions, with hyperchromic and weakly cytoplasmatic nucleus, having vesicular chromatin, pronounced nucleoli. There were also hypocellularity areas with the presence of keloid type collagen, extensive areas of hyalinosis, sometimes in the middle there were cavities filled with blood, diapedesing hemorrhage, accumulation of hemosiderin and hematoidin, mixed inflammatory cellular infiltration, including giant cells, focal infiltration of lymphocytes, hyperemic vessels and a lot of vascular fissures. In one of the sections, an opening of the cystic cavity was observed, with blood content, skin manifestation, tissue detritus and leukocytes. In other sections, epidermal hyper keratinization, acanthosis, dermal fibrosis, and ganglion-type cell accumulation were found. There was also a lymphoplasmacytic focal infiltration of muscle tissue. This histological picture is most comparable to the diagnosis of nodular fasciitis (Figures 9-11). Based on the history, clinical picture, and histopathological examination, the lesion was diagnosed as nodular fasciitis.
Figure 10: Foci of fibrosis and hyalinosis.
Figure 11: Hyper cellular areas.
Discussion
Nodular fasciitis is a rare benign soft tissue tumor, most commonly afflicting the soft tissues of upper extremity followed by trunk, head, and neck [15]. Oro-facial lesions involve the skin of the face, parotid gland, buccal mucosa, labial mucosa, and tongue16. Lesions are small, solitary, and are commonly located on extremities occasionally on the trunk and infrequently on the head and neck. Nodular fasciitis is also known as pseudo sarcomatous fasciitis, pseudosarcomatous fibromatosis and infiltrative fasciitis. The etiology is still unknown. It is considered to occur due to unusual proliferation of myofibroblasts triggered by local injury or inflammatory process [16].
Previously nodular fasciitis was thought to be reactive in nature. Infection and hormonal influences have also been suggested as initiating factors [2, 17, 18]. However, genetic research proves that nodular fasciitis undergoes a clonal expansion process [8]. It is commonly seen in the 40-50-year age group with almost equal distribution amongst both genders. It almost always poses a considerable diagnostic challenge. However, fuzzy cytoplasmic borders, multiple fragile cytoplasmic processes, and prominent nucleoli favor a diagnosis of nodular fasciitis [19, 20]. Nodular fasciitis can be differentiated from other facial mesenchymal tumors, including sarcomatoid carcinoma, fibrosarcoma, leiomyosarcoma, and neurofibroma, based on histology, molecular biology, and immunohistochemistry [21].
In cases of nodular fasciitis, proactive efforts are needed to perform histopathologic evaluation and treatment. The histological appearance of nodular fasciitis can be described as deceptive, due to its non- specific and, even though well demarcated, infiltrative nature. The lesion also has a rich vascularity and is mitotically active. This rapid growth and histological features make nodular fasciitis a mimicker of malignancies such as sarcomas [22, 23]. A nodular fasciitis should be surgically excised to obtain complete cure as the chances of local recurrence are almost nil (<1%) [24].
We report a rare case of nodular fasciitis of neck in an 83-year-old lady. Clinical, laboratory, radiological methods were used in the examination of patients. Aspiration of the swelling did not show any contents. Тo establish a final diagnosis, we conducted a histological examination. Tumor has been removed as a solid mass. The material was sent for histopathological examination and the lesion was diagnosed as nodular fasciitis. After surgery patient expressed satisfaction with the treatment and with good long-term results. In cases of nodular fasciitis, proactive efforts are needed to perform histopathologic evaluation and treatment because nodular fasciitis tends to grow rapidly.
Acknowledgements
We thank the Parandzem Khachatryan M.D., Ph.D. Chief Pathologist (MOH RA Head of the Department of Clinical Pathology, Heratsi Hospital Complex, YSMU, Armenia) for help with the histopathological examination.
Conflicts of Interest
None.
Protection of Human and Animal Subjects
The authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee Yerevan State Medical University after M. Heratsi (protocol N23.11.2018) and in accordance with those of the World Medical Association and the Helsinki Declaration.
Consent Statement
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Article Info
Article Type
Case ReportPublication history
Received: Wed 08, Jan 2020Accepted: Fri 07, Feb 2020
Published: Wed 19, Feb 2020
Copyright
© 2023 Gagik Hakobyan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DOBCR.2020.01.03
Author Info
Anna Pogosyan Gagik Hakobyan Margarita Hovhannisyan Martin Misakyan Seda Burnazyan
Corresponding Author
Gagik HakobyanProfessor, Head of Department of Oral and Maxillofacial Surgery Yerevan State Medical University after M. Heratsi, Armenia
Figures & Tables

References
- Konwaler BE, Keasbey L, Kaplan L (1955) Subcutaneous pseudosarcomatous fibromatosis (fasciitis). Am J Clin Pathol 25: 241-252. [Crossref]
- Han W, Hu Q, Yang X, Wang Z, Huang X (2006) Nodular fasciitis in the orofacial region. Int J Oral Maxillofac Surg 35: 924-927. [Crossref]
- Lloyd A, Witheiler D, Menter A (2015) Nodular fasciitis of the lip mucosa: a rare but clinically important entity. Clin Exp Dermatol 40: 408-412. [Crossref]
- Davies HT, Bradley N, Bowerman JE (1989) Oral nodular fasciitis. Br J Oral Maxillofac Surg 27: 147-151.
- Choi JH, Ro JY (2018) Cutaneous Spindle Cell Neoplasms Pattern-Based Diagnostic Approach. Arch Pathol Lab Med 142: 958-972. [Crossref]
- Montgomery EA, Meis JM (1991) Nodular fasciitis. Its morphologic spectrum and immunohistochemical profile. Am J Surg Pathol 15: 942-948. [Crossref]
- Graham BS, Barrett TL, Goltz RW (1999) Nodular fasciitis: response to intralesional corticosteroids. J Am Acad Dermatol 40: 490-492. [Crossref]
- de Carli ML, Sa Fernandes K, dos Santos Pinto D Jr, Witzel AL, Martins MT (2013) Nodular fasciitis of the oral cavity with partial spontaneous regression. Head Neck Pathol 7: 69-72. [Crossref]
- Ko CJ (2012) Dermal hypertrophies and benign fibroblastic/myofibroblastic tumors. In: Goldsmith LA, Fitzpatrick TB, editors. Fitzpatrick's dermatology in general medicine. 8th ed. New York: McGraw-Hill 715-716.
- Oliveira AM (2014) Mesenchymal Tissue Pathology: Nodular Fasciitis. Pathobiology of Human Disease: A Dynamic Encyclopedia of Disease Mechanisms.
- Sinhasan SP, K V B, Bhat RV, Hartimath BC (2014) Intra-muscular Nodular Fasciitis Presenting as Swelling in Neck: Challenging Entity for Diagnosis. J Clin Diagn Res 8: 155-157. [Crossref]
- Leventis M, Vardas E, Gkouzioti A, Chrysomali E, Chatzistamou IJ (2011) Cranio-Maxillofac Surg 39: 340-342.
- Oh BH, Kim, Zheng Z, Roh MR, Chung KY (2015) Treatment of Nodular Fasciitis Occurring on the Face. Ann Dermatol 27: 694-701. [Crossref]
- Shimizu S, Hashimoto H, Enjoji M (1984) Nodular fasciitis: an analysis of 250 patients. Pathology 16: 161-166. [Crossref]
- Meister P, Buckman FW, Konrad E (1978) Nodular fasciitis (analysis of 100 cases and review of the literature). Pathol Res Pract 162: 133-165. [Crossref]
- Dayan D, Nasrallah V, Vered M (2005) Clinico-pathologic correlations of myofibroblastic tumors of the oral cavity: 1. Nodular fasciitis. J Oral Pathol Med 34: 426-435. [Crossref]
- Nair P, Barrett AW, Theodossya T (2004) Oral nodular fasciitis: case report. Br J Oral Maxillofac Surg 42: 360-362. [Crossref]
- Lima FJ, Diniz de Sousa Lopes ML, Jose de Oliveira Nobrega F, Dantas da Silveira EJ (2014) A rare case of intraoral nodular fasciitis: diagnosis and immunohistochemical profile. J Oral Maxillofac Surg 72: 529-536. [Crossref]
- Cyriac MJ, Celine MI, Kurien G, Puthiode U (2004) Nodular fasciitis. Indian J Dermatol Venreol Leprol 70: 239-241.
- Reitzen SD, Dogan S, Har El G (2009) Nodular fasciitis: A case series. J Laryngol Otol 123: 541-544. [Crossref]
- Jain D, Khurana N, Jain S (2008) Nodular fasciitis of the external ear masquerading as pleomorphic adenoma: A potential diagnostic pitfall in fine needle aspiration cytology. Cytojournal 5: 14. [Crossref]
- Lenyoun EH, Wu JK, Ebert B, Lieberman B (2008) Rapidly Growing Nodular Fasciitis in the Cheek of an Infant: Case Report of a Rare Presentation. Eplasty 8: e30. [Crossref]
- Haddad AJ, Avon SL, Clokie CM, Sandor GK (2001) Nodular fasciitis in the oral cavity. J Can Dent Assoc 67: 664-667. [Crossref]
- Allen PW (1972) Nodular fasciitis. Pathology 4: 9-26. [Crossref]
