Training Non-Specialists for Craniomaxillofacial Trauma in a Warzone Setting
A B S T R A C T
This study investigated a simulated craniomaxillofacial (CMF) trauma training programme for non-specialist clinicians involved in warfare environments. Many clinicians lack CMF surgical training and the course was designed as a one-day research programme to establish if non-specialists could acquire CMF trauma skills adequate for a warzone. The course consisted of six simulation skills, of which four used sheep heads to teach craniotomy, epistaxis, canthotomy and cantholysis and external pin fixation for mandibular fracture fixation. In addition, two skills utilised plaster dental models designed to enable fixation of mandibular fractures with the Erich arch bar or dental eyelet wiring. This simulation-based programme taught trauma management without the expense of cadavers or risks to patients [1]. The trainees were scored for each of the six skills by hierarchical task analysis (HTA) designed by CMF specialists [2, 3]. The trainee assessment scores improved significantly in all skills post-training, regardless of their medical or surgical deficiencies demonstrating that non-specialists can learn important surgical techniques, valuable for war environments.
Keywords
Non-specialist clinician, simulation training, skill stations, hierarchical task analysis
Introduction
A familiar aphorism applied to learning surgical skills is: “see one, do one and teach one”, but is unproven, inconvenient and medico-legally unsound. This craniomaxillofacial (CMF) surgery training course for non-specialists was designed to overcome the skills deficiency in a warzone. Extreme aggression and destruction require appropriately trained military forces [4]. The British military created a 6-week programme in Helmand Province, Afghanistan, considered equivalent to 3 years training in the UK while the US military designed a similar CMF surgery unit during the Iraq Freedom War [5, 6]. Trauma simulation training of non-specialists is successful and economical [7]. A Delphi consensus study provided a CMF trauma curriculum based on its members’ specialist experience and the Royal College of Surgeons (UK), Surgical Training course for Austere Environments (STAE). This is hosted twice annually by David Nott, an outstanding war trauma surgeon [8-11]. While approximately 85% of these courses use cadavers and last over 5 days, our single day CMF surgery course utilised sheep heads and plaster dental models, which is acceptable for non-specialist courses [12, 13].
Methods
A single day course was designed covering 6 surgical skills: craniotomy, nasal packing for epistaxis, canthotomy & cantholysis, external pin fixation for mandibular fractures, Erich arch bar and Ivy dental loops for intermaxillary fixation (IMF). We aimed to train non-specialist surgeons to perform CMF techniques improving the outcome for casualties in an austere war environment. The 11 participants had medical or dental qualifications but no CMF experience, established from a questionnaire. The 2 trainers were a maxillofacial surgeon and neurosurgeon, supported by 15 specialists. The curriculum and timetable were decided by a panel of specialised surgeons using the Delphi consensus method, consisting of 6 skills divided into 3 sessions. The first session assessed participants on each skill without prior training or assistance (Table 1). The second and third sessions were structured as the demonstration of a skill by a specialist followed by reassessment of the participants. Each assessment was based on hierarchical task analysis (HTA) designed specifically for each skill to evaluate participant success. A critical step of each skill was identified to be performed correctly for successful completion of the skill, ensuring an optimum patient outcome. The skills were designed to be performed under austere conditions with conventional instrumentations with the assumption that a high number of casualties require treatment.
Furthermore, the course was designed to be delivered in an austere environment with inexpensive and accessible simulation instruments. 4 skill stations used sheep heads and 2 skill stations utilised plaster jaw models. Sheep heads were used as they are inexpensive and likely available in warzones. All participants received written information and informed consent was obtained prior to participation. Ethical approval for the study was obtained from the Queen Mary University of London.
Results
I Craniotomy
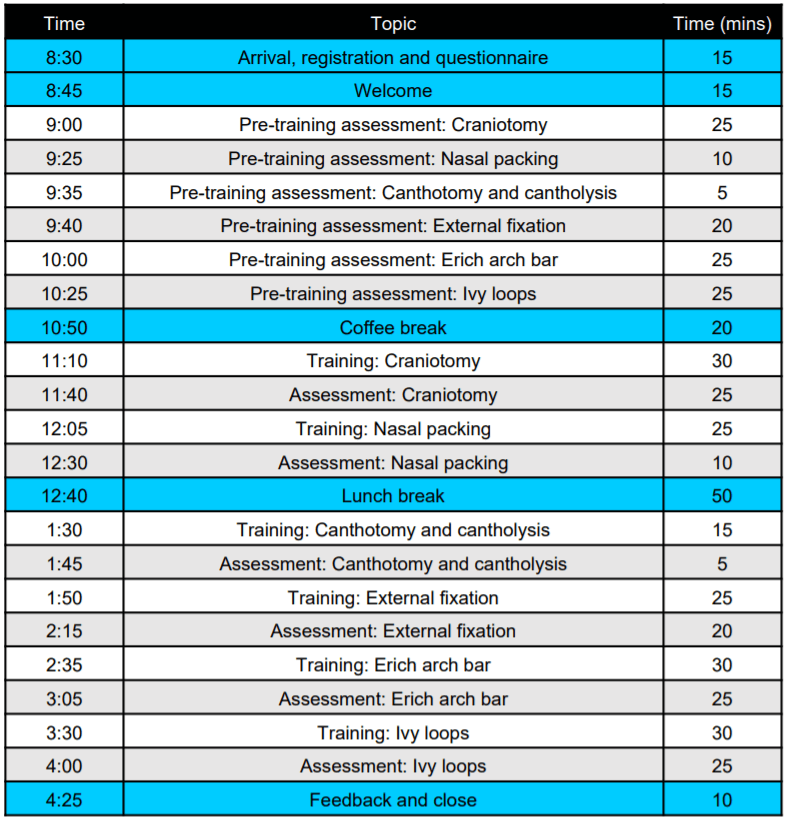
Craniotomy is a vital procedure to access extra or intracranial fractures and haemorrhage as demonstrated using a sheep head (Figure 1A). If performed incorrectly, it will result in brain damage and is, therefore, a lifesaving technique to teach in a warzone. The skill was divided into 8 steps that were agreed on by a neurosurgeon: (a) position the sheep head appropriately, (b) make the scalp incision, (c) turn the dissection of the scalp flap, (d) drill the burr holes, (e) successfully raise the bone flap – the critical step, (f) open the dura and aspirate the hematoma, (g) close the dura and replace the bone flap, (h) candidate assessed for technical use of the drill. Dental surgical pieces are not ideal for craniotomy; however, an electrical surgical drill is useful to make burr holes, although in a war environment, a manual drill may be used during a power failure. The assessment scores showed a pre-training mean of 15.9/40 compared to a post-training mean of 33.2/40, a significant improvement in craniotomy post-training with improved trainee scores in all 8 steps (Figure 1B). Furthermore, the perceived ability level for the candidates increased post-training (Figure 1C).
Figure 1: Craniotomy A) Craniotomy steps: a) dissection of the pericranium layer, b) cutting along the burr holes, c) exposing the brain, d) irrigation by normal saline, e) craniotomy closure, f) suturing the scalp. B) Candidate assessment scores pre- and post-training, red bars denote failed assessments. Wilcoxon signed-rank test showed that craniotomy training elicited a statistically significant improvement. A pre-score mean of 15.9 compared to a mean post-score of 33.2 (Z=-2.936, p<0.01). The trainee scores improved in every one of the 8 steps of craniotomy training. C) Trainee ability pre- and post-training.
Instruments: (1) electrical or manual drill, (2) scalpel blades, numbers 10 & 15, (3) periosteal elevator, (4) 10ml syringe with 22-24G needle for saline irrigation, (5) dissection forceps, (6) straight arterial forceps & scissors, (7) 4/0 polyglyconate suture or black silk 3/0 suture, (8) sheep head.
II Nasal Packing for Epistaxis
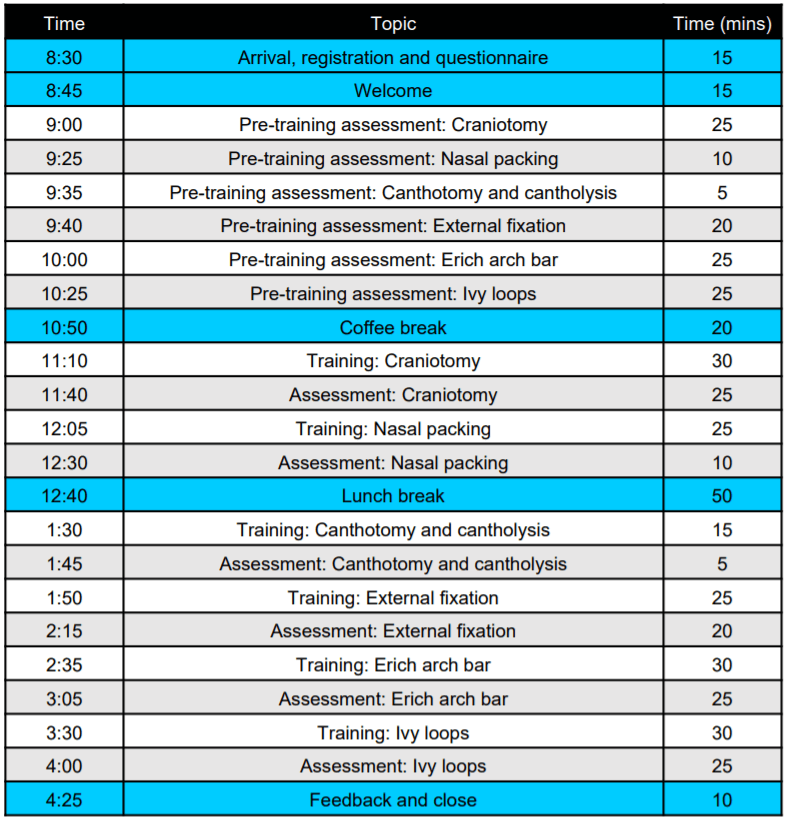
CMF trauma commonly causes epistaxis from the anteroinferior nasal septum (Littles area), where four arteries anastomose forming a vascular plexus. An anterior bleeding point is compressed or cauterised by applying silver nitrate or lidocaine (2%) with adrenaline (1/200,000) by anterior rhinoscopy; however, this cannot be demonstrated with a sheep's head [14]. Excluding a patient’s medication such as anticoagulants or aspirin is crucial but in austere settings, patient history is inaccessible. A Foley catheter was inserted into the sheep head and inflated to stop bleeding (Figure 2A). The steps for this skill were: (a) insert the Vaseline lubricated catheter – the critical step, (b) inflate the balloon by injecting 10-15ml saline, water or air, (c) retract the catheter sufficiently ensuring the balloon securely tamponades the nasopharynx, (d) anterior nasal packing with Vaseline gauze, (e) protect the columella and septum, (f) secure the catheter with an umbilical clamp. The sheep’s head was effective for simulating nasal packing, although the nasal floor is longer than a human. 5/11 trainees passed this task, which improved to 11/11 post-training (Figure 2B).
The mean pre to post-training scores were 12 to 27/30, an overall improvement of 50%. The critical step for this task was the correct insertion of the catheter and stabilisation in the nasopharynx. Post-training, all candidates scored 22/30 or above with 4 obtaining full marks which were statistically significant. Low ability was seen in 8/11 candidates pre-training, improving considerably in post-training (Figure 2C). One assessment shortcoming was the lack of fluid to determine if the packing stopped the bleeding into the nasopharynx, potentially simulated by injecting a dye through the nostril into the nasopharynx.
Figure 2: Nasal packing for epistaxis A) Nasal packing steps: a) Foley catheter insertion into the nasopharynx highlighted by the yellow arrow, b) inflation of the catheter with water, c) check the position of the inflate catheter, d) secure the catheter anteriorly with a umbilical clamp to protect the nasal cartilage (yellow arrow). B) Candidate assessment scores pre- and post-training, red bars denote failed assessments. The Wilcoxon signed-rank test showed that nasal packing training elicited a statistically significant increase in trainee scores compared to pre-training (Z=-2.94, p<0.01) with a mean post-score of 26.45 compared to a pre-score mean of 11.91. These scores improved in every one of the nasal packing training. C) Trainee ability pre- and post-training.
Instruments: (1) 10ml syringe with 22-24G needle, (2) female Foley catheter, (3) anaesthetic (lignocaine with 1/200,000 adrenaline), (4) fine dissection forceps, (5) straight arterial forceps & scissors, (6) Vaseline ribbon gauze, (7) umbilical plastic clips, (8) sheep head.
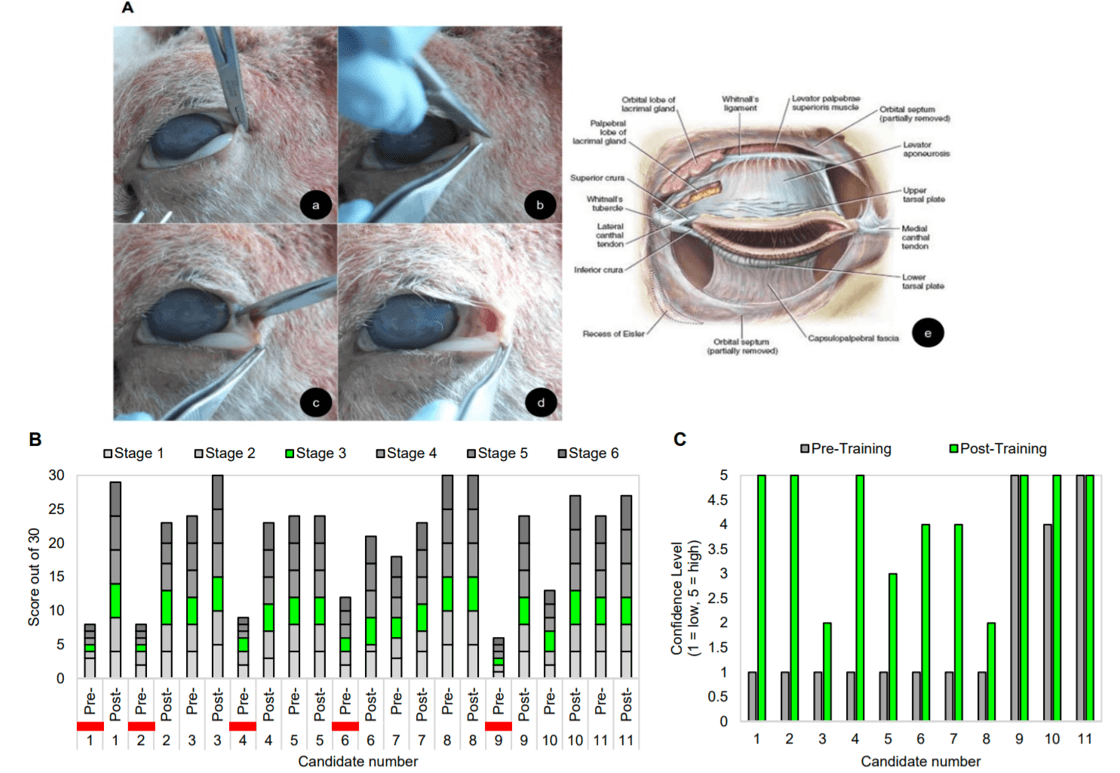
III Lateral Canthotomy and Cantholysis
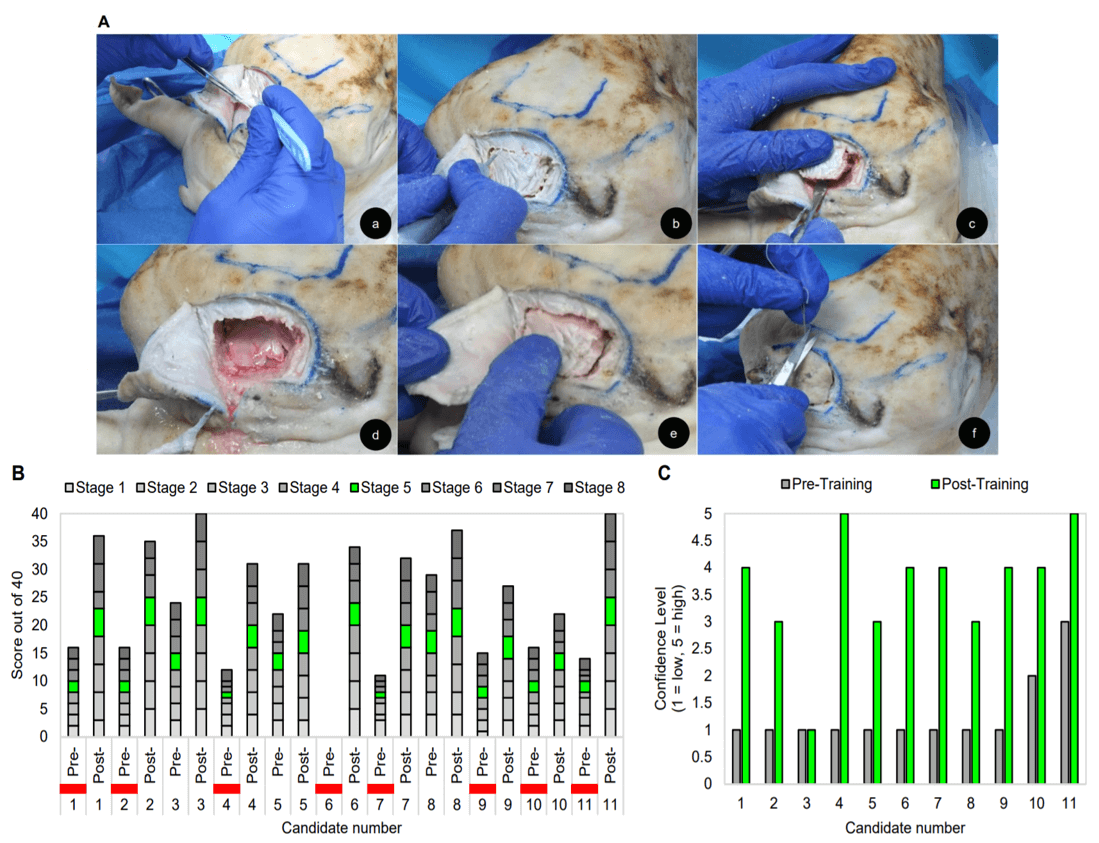
Retrobulbar haemorrhage is associated with facial traumas, rapidly filling the orbit behind the globe, pressuring the eyelid creating orbital compartment syndrome. This compresses the optic nerve and vascular supply leading to permanent sight loss. The medial and lateral canthal tendons hold the eyelids in place, creating a compartment with limited space for the globe. The lateral canthotomy is an incision through the lateral canthal ligament, relieving retrobulbar pressure. The inferior crus of the lateral canthal tendon is cut if severing the tendon fails to release the globe, termed disinsertion (Figure 3A). Rapid treatment prevents orbital compartment syndrome. In warzones, specialists are rarely available, so non-specialists should learn this sight-saving procedure. Each trainee was provided with orbits simulating compartment syndrome, created by injecting glycerine measured digitally or by tonometer to determine intraocular pressure. The candidates were video-recorded and assessments made from recordings, graded by two ophthalmic surgeons.
This task was divided into 5 steps: (a) administer anaesthesia at the lateral border of the orbit, (b) devascularise the tendon using a clamp or forceps crushing the lateral canthus, (c) cut the lateral canthus – the critical step, (d) assessments of instrument handling, (e) tissue handling and (f) surgical planning. If decompression is not achieved at the critical step, the inferior crus (crura) is cut, termed cantholysis. The inferior crus is identifiable when "strumming" it with scissors. 5/11 participants failed the pre-training assessment, but all passed post-training, scoring 16/30 pre-training and 26/30 post-training showing significant improvement (Figure 3B). Candidates also improved in ability after training, although 7/11 candidates had previous experience of cantholysis (Figure 3C).
Figure 3: Lateral canthotomy and cantholysis A) Canthotomy and cantholysis steps: a) Forceps are used to devascularised the lateral canthus tendon, b) the lateral canthus is cut, c) the lower eyelid is undermined, d) the lower eyelid is released and free to rotate, e) eyelid showing the lateral canthal tendon which is divided to relieve the orbital compartment pressure – (canthotomy); if it fails the inferior crus is also divided (cantholysis) [23]. B) Candidate assessment scores pre- and post-training, red bars denote failed assessments. The Wilcoxon signed-rank test applied to the HTA data showed that canthotomy training elicited a statistically significant increase in participant scores compared to pre-training (Z=-2.431, p<0.05) with a mean post-score of 23.27 compared to a pre-score mean of 16. Scores improved in nine canthotomy post-training steps, but two trainees were already skilled. C) Trainee ability shows a substantial improvement post-training.
Instruments: (1) 10ml syringe with 22-24G needle, (2) anaesthetic (lignocaine with adrenaline), (3) dissection forceps, (4) straight arterial forceps & tenotomy scissors, (5) Vaseline gauze, (6) sterile gauze, gloves and drapes, (7) ophthalmic antibiotic ointment such as erythromycin 0.5% or bacitracin, (8) sheep head.
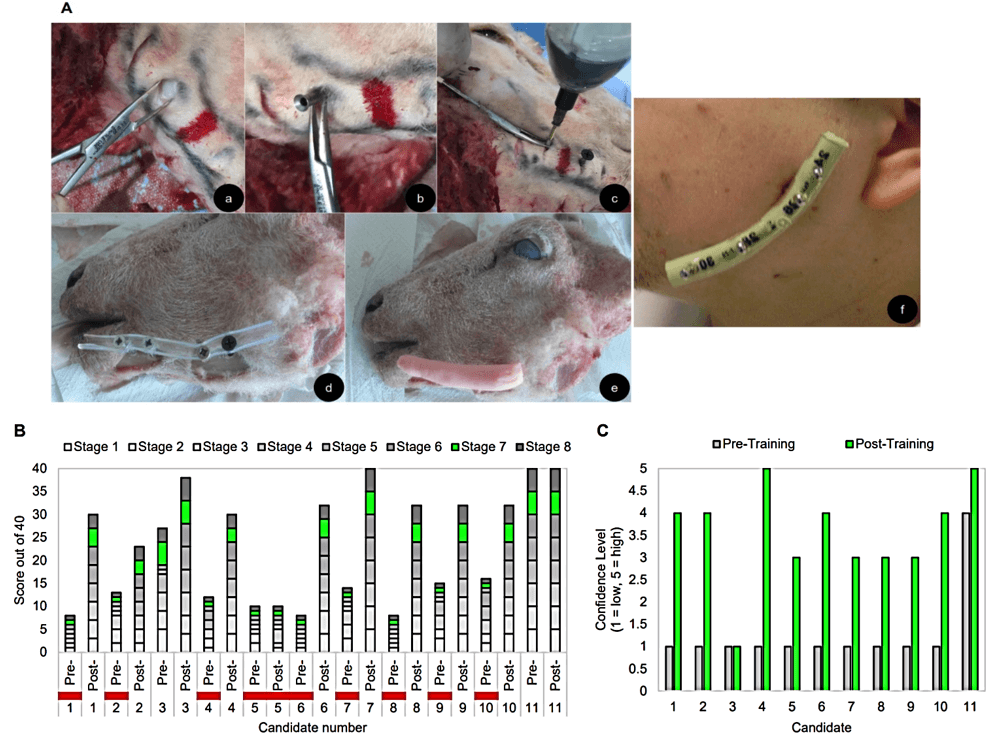
IV External Pin Fixation for Mandibular Fractures
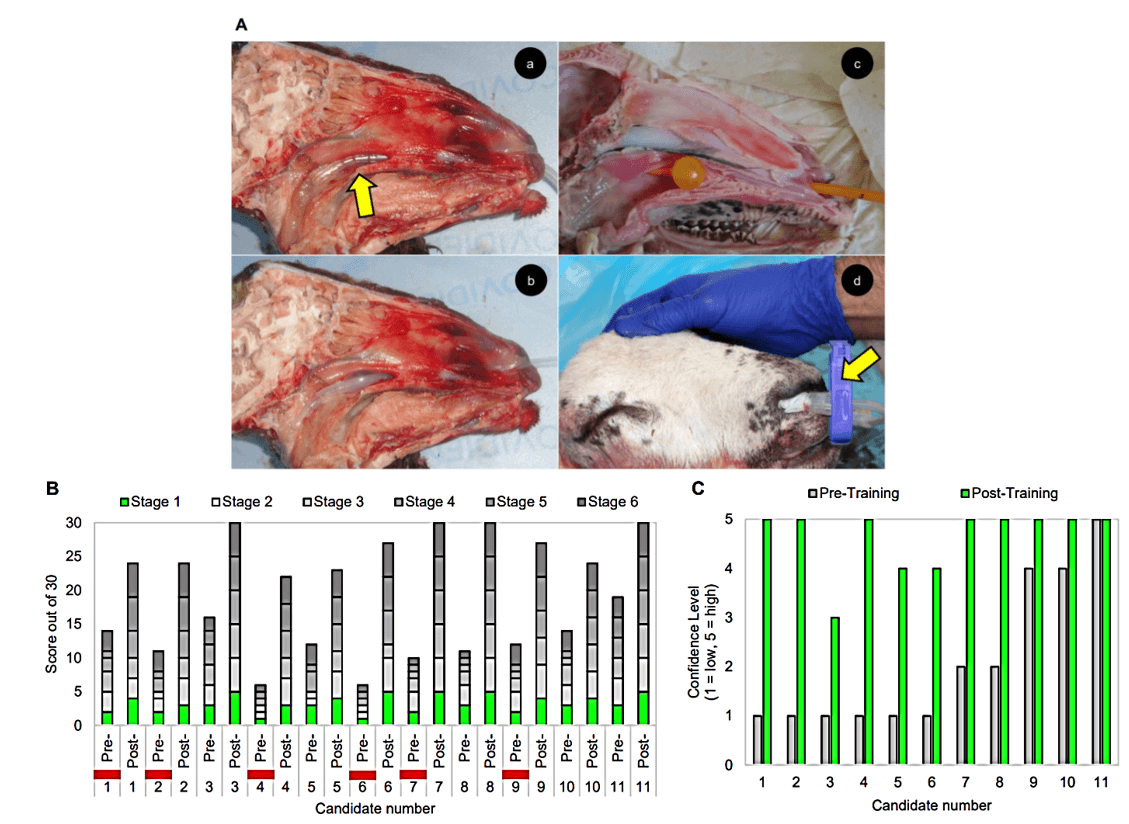
Mandibular fractures are commonly fixed using an intermaxillary Erich arch bar or Ivy eyelet wiring loops. Given the equipment, internal fixation with plates and screws provide stability to fractures [15]. External pin fixation is the combination of self-tapping orthopaedic screws (fixator pins) to localise the fracture components, which are then stabilised by an acrylic filled silicone tube instead of a metal connecting bar with screw clamps (Figure 4A) [16, 17]. An electric orthopaedic drill was used but power failures are common in war environments; hence a manual orthopaedic drill is more practicable. Sheep heads were viable for training; however, anatomical and dental differences to humans complicate IMF.
The steps for this skill are: (a) mark the anatomical features on the sheep head including the lower mandible border, inferior alveolar and mental nerves and tooth apices, (b) mark site and make incisions for inserting the screws, (c) insert mosquito forceps to expose the jawbone, (d) insert the first screw, (e) insert screws in parallel with a 10mm gap between each, through the split silicone tube, (f) make the screw fixator by mixing liquid acrylic monomer and powder polymer, then transfer into the silicone tube - the critical step, (g) check parallelism, stability and accuracy of the screws to ensure a stable occlusion. 9/11 trainees failed the pre-training assessment and only 1/11 failed the post-training test (Figure 4B). The average scores pre and post-training were 16/40 and 31/40, respectively indicating, improved levels of skill and confidence (Figure 4C). HTA data showed a significant increase in trainee scores, also improving in all of the steps.
Figure 4: External pin fixation for mandibular fractures A) External fixation steps: a) spreading the margins of the incised overlying skin to insert the bone screw, b) the screw site protected by a metal sleeve, c) inserting the screw adjacent to the red fracture site, d) split silicone tube with screws in situ e) acrylic embedded screws, f) the acrylic filled silicone tube stabilises the bone screw inserted to fix the reduced mandibular fracture [24]. B) Candidate assessment scores pre- and post-training, red bars denote failed assessments. HTA data when analysed by the Wilcoxon signed-rank test showed that fixation training produced a significant increase in trainee scores compared to pre-training (Z=-2.67, p<0.01) with a post mean score of 30.8 compared to the pre-score mean of 15.6. The trainee scores also improved in every one of the 8 steps of the fixation. C) Pre- and post-training ability showing an increase in ability.
Instruments: (1) electrical easy access screwdriver, (2) 4x 7.5x80mm screws (sky satellite screws), (3) 11mm diameter flexible silicone tube, (4) scalpel number 11, (5) mosquito forceps, (6) methyl methacrylate monomer and polymer, (7) sheep head.
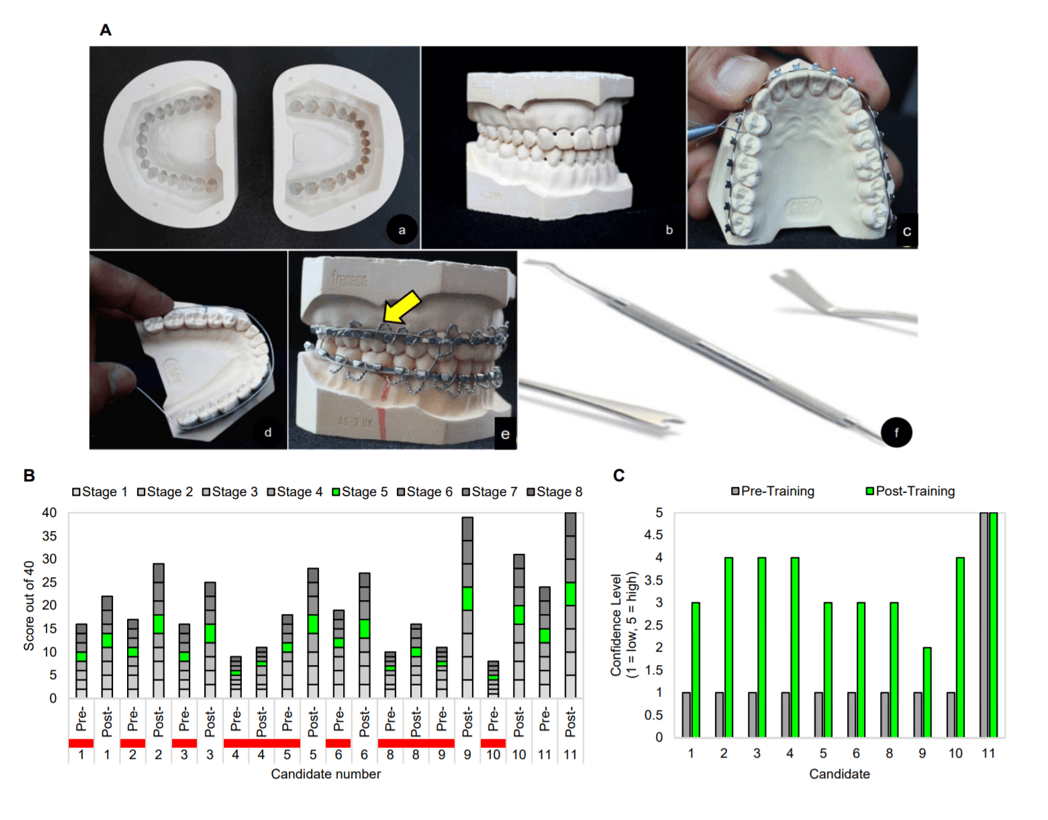
V Erich Arch Bar Fixation
The Erich arch bar is a valuable skill for non-specialists and dentoalveolar fracture management was simulated on plaster models. The plaster jaw models (with narrow interdental drill holes) are inexpensive and easy to generate; however, in clinical practice, the patients’ dentition is examined for missing teeth, malocclusion and periodontal instability to use arch bars. It is retained by wire passed through the drilled interdental holes. The technique requires candidates to manipulate steel wire as the plaster models are not articulated and do not provide buccal soft tissues, lips or tongue as landmarks (Figure 5A). The steps for the task are: (a) cut the correct length of arch bars in relation to each jaw, (b) align and position arch bars on each jaw, (c) stretched steel wire loops fix the arch bar to the dentition, (d) make 12 loops, 6 for each jaw, (e) tighten the loops - the critical step, (f) assess the dental occlusion, (g) the candidates were scored on instrument handling and (h) the logic of the sequence followed. 9/10 trainees (one resigned) failed pre-training demonstrating lacked arch bar experience (Figure 5B).
Despite this, 8/10 passed post-training with low average scores but showed a statistically significant increase. The overall ability levels also increased post-training (Figure 5C). The candidate performance was restricted by the inadequate allotted time of 25 minutes and as the final session of a day, fatigue may contribute. Another criticism of plaster model was the upper and lower jaws were not attached to an articulator and lack soft tissue.
Figure 5: Skill Erich arch bar fixation: A) Erich arch bar fixation steps: a) silicone mould, b) dental plaster model, c) a length of stainless steel wire is measured to be the circumference of the arch bar, d) twisting the wire loop to fix the arch bar, e) IMF with a wire loop (yellow arrow), f) probe or ligature director to push the wire beneath the dental cingulum. B) Candidate assessment scores pre- and post-training, red bars denote failed assessments. The Wilcoxon signed-rank test showed a statistically significant increase in trainee scores compared to pre-training (Z=-2.81, p<0.01) with a mean post-score of 26.8 compared to a pre-score mean of 14.8. Participants scores improved significantly in nine of the eleven steps within Erich arch bar training. C) Trainee ability pre- and post-training.
Instruments: (1) Erich arch bars adequate for 2 arches, (2) 24 gauge stainless steel wire; gauge 0.5mm, (3) probe or ligature director to push the wire beneath the cingulum of the teeth, (4) scalpel 15 blade l, (5) wire twister and cutter, (6) mosquito haemostat, (7) elastic bands, (8) plaster jaw model.
VI Ivy Eyelet Wire Loop
While Erich arch bars are the recommended method for IMF, Ivy loops made from stainless steel wire is an alternative method if arch bars are unavailable (Figure 6A). The same drilled plaster models were used for the task. Although the plaster jaws are easily handled, a patient is invariably recumbent with a jaw hinge axis enclosed by orofacial soft tissues. The principle skill of jaw fixation is to achieve tight wiring to provide stable dental occlusion.
The steps for this task are: (a) cut appropriate lengths of steel wire to make 8 individual loops, (b) twist wires 4 times into consistent Ivy loops, (c) insert the free ends of the loops through the papillary interdental holes from buccal to lingual, then pass one wire around the distal teeth to the buccal side through the loop. The other wire is passed around the medial tooth and twisted with its distal half to anchor the loop. Wire the jaws with an IMF wire through the loops and tighten by twisting the ends clockwise. Cut any excess and place the twisted wire along the gingivae, (d) insert 4 upper and lower loops, (e) check the tightness of the loops which is the critical stage, (f) assess the dental occlusion, (g) the candidates were scored on instrument handling and (h) the logic of the sequence followed. All candidates failed the task pre-training session but passed after (Figure 6B). The average scores pre and post-training were 15/40 and 27/40, respectively, with only 4 candidates scoring 30 and above; however, the improvement post-training was significant. Furthermore, the ability level for all candidates improved post-training (Figure 6C).
Figure 6: Ivy eyelet wire loop A) Ivy eyelet loop steps: a) individual Ivy loops are made with wire, b) loops are inserted between the interdental spaces, c) long wires are threaded through the loop and twisted together to secure, d) loops are made for both the upper and lower jaw, e) wire is used to interlock the jaws and fix the dental occlusion. B) Candidate assessment scores pre- and post-training, red bars denote failed assessments. The Wilcoxon signed-rank test of the hierarchical task analysis data showed that eyelet wiring training was statistically significantly improved in the trainee scores compared to pre-training (Z=-2.80, p<0.01) with a mean post-score of 30.8 compared to a pre-score mean of 15.55. C) The ability levels increased post-training for eyelet wire fabrication and IMF application.
Instruments: (1) 15cm of 25-26 gauge (0.5mm diameter) stainless steel wire, (2) probe to push wire beneath the cingulum of the teeth, (3) scalpel, (4) wire twister and cutter, (5) mosquito haemostat, (6) plaster jaw model.
Discussion
The results of training non-specialised clinicians demonstrated that trainees could be successfully taught CMF surgical skills on inexpensive simulation models. As the course was designed for war environments, we were unable to measure the trainee’s ability under stress but there was considerable improvement in performance. However, the timetable was demanding and could be extended to assess whether candidates retained their learned skills. Plaster jaw models were optimal for teaching IMF techniques, particularly as sheep have an incongruous dental and facial anatomy, although their soft tissues are superior to plaster models that lack a tongue, lips, facial tissue and jaw axis. This species difference could be overcome for some skills with a plaster model articulator. The HTA assessment was generated for each skill by appropriate surgical specialists which ensured accuracy. This combination of the simulation adaptation of the sheep's head and plaster models, the HTA and expert video recording can train non-specialists CMF surgery techniques in a war environment.
Conclusion
Based on this study, an extended CMF programme for non-specialist clinicians can be covered in 3 days, this supported by HTA frameworks provided by appropriate specialists. An enlarged programme should include ATLS gaps, gross soft tissue trauma management, interpretation of head and neck imaging and a maxillofacial trauma scoring software application [18, 19]. Also, of great importance are head, face and neck injuries in children which represent 67% of trauma, especially from blast injuries [20]. Other considerations are ethics, post-traumatic stress disorders, terrorism and poverty. A parallel issue has been the COVID-19 pandemic which emphasised the need for training retired clinicians, medical students and staff to compensate for an overcommitted health service. The value of simulation training contradicts the philosophy of Ambroise Paré insisting the gap between a surgical training course and its implementation, is on the battlefield; “He who desires to practice surgery must go to war”, now seen as an unproven aggressive concept (Figure 7) [21-23]. The results of this course show significantly improved trainee scores in all skills regardless of their lack of surgical experience or specialist background.
Figure 7: Ambroise Paré (1510-1590) performing an amputation in a warzone.
Acknowledgements
Invaluable support for this study was provided by: Simon Myers; Ali Ghanem; Simon Holmes; David Nott; Gehad Youssef; Mohamed Shibue, Habib Elamoshi;, Jamal El-Swiah, Michael Perry; Georgios Pafitanis, Stephen Watt-Smith, Shameem Shariff, Nasier Nasser, the Red Cross, Medicins Sans Frontier. The course also depended on the support of the David Nott Foundation and the RCS (Eng).
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 29, Jul 2020Accepted: Thu 20, Aug 2020
Published: Mon 07, Sep 2020
Copyright
© 2023 Abdulhakim W Zaggut. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JDOA.2020.02.06
Author Info
Abdulhakim W Zaggut Muhammad M Rahman Ali Ghanem Simon Myers Malcolm Harris
Corresponding Author
Abdulhakim W ZaggutCentre for Cell Biology & Cutaneous Research, The Blizard Institute, Barts and the London School of Medicine and Dentistry, Queen Mary University of London, London, UK
Figures & Tables
Instruments: (1) electrical or manual drill, (2) scalpel blades, numbers 10 & 15, (3) periosteal elevator, (4) 10ml syringe with 22-24G needle for saline irrigation, (5) dissection forceps, (6) straight arterial forceps & scissors, (7) 4/0 polyglyconate suture or black silk 3/0 suture, (8) sheep head.
Instruments: (1) 10ml syringe with 22-24G needle, (2) female Foley catheter, (3) anaesthetic (lignocaine with 1/200,000 adrenaline), (4) fine dissection forceps, (5) straight arterial forceps & scissors, (6) Vaseline ribbon gauze, (7) umbilical plastic clips, (8) sheep head.
Instruments: (1) 10ml syringe with 22-24G needle, (2) anaesthetic (lignocaine with adrenaline), (3) dissection forceps, (4) straight arterial forceps & tenotomy scissors, (5) Vaseline gauze, (6) sterile gauze, gloves and drapes, (7) ophthalmic antibiotic ointment such as erythromycin 0.5% or bacitracin, (8) sheep head.
Instruments: (1) electrical easy access screwdriver, (2) 4x 7.5x80mm screws (sky satellite screws), (3) 11mm diameter flexible silicone tube, (4) scalpel number 11, (5) mosquito forceps, (6) methyl methacrylate monomer and polymer, (7) sheep head.
Instruments: (1) Erich arch bars adequate for 2 arches, (2) 24 gauge stainless steel wire; gauge 0.5mm, (3) probe or ligature director to push the wire beneath the cingulum of the teeth, (4) scalpel 15 blade l, (5) wire twister and cutter, (6) mosquito haemostat, (7) elastic bands, (8) plaster jaw model.

Instruments: (1) 15cm of 25-26 gauge (0.5mm diameter) stainless steel wire, (2) probe to push wire beneath the cingulum of the teeth, (3) scalpel, (4) wire twister and cutter, (5) mosquito haemostat, (6) plaster jaw model.
References
- Fatimah Lateef (2010) Simulation-based learning: Just like the real thing. J Emerg Trauma Shock 3: 348-352. [Crossref]
- Sudip K Sarker, Avril Chang, Tark Albrani, Charles Vincent (2008) Constructing hierarchical task analysis in surgery. Surg Endosc 22: 107-111. [Crossref]
- R Reznick, G Regehr, H MacRae, J Martin, W McCulloch (1997) Testing Technical Skill via an Innovative “Bench Station” Examination. Am J Surg 173: 226-230. [Crossref]
- T M Krummel (1998) Surgical simulation and virtual reality: the coming revolution. Ann Surg 228: 635-637. [Crossref]
- Arul Ramasamy, David E Hinsley, Daffyd S Edwards, Michael P M Stewart, Mark Midwinter et al. (2010) Skill sets and competencies for the modern military surgeon: Lessons from UK military operations in Southern Afghanistan. Injury 41: 453-459. [Crossref]
- R Bryan Bell (2007) The role of oral and maxillofacial surgery in the trauma care center. J Oral Maxillofac Surg 65: 2544-2553. [Crossref]
- K Pringle, J M Mackey, P Modi, H Janeway, T Romero et al. (2015) "A short trauma course for physicians in a resource-limited setting: Is low-cost simulation effective?" Injury 46: 1796-1800. [Crossref]
- Gene Rowe, George Wright (1999) The Delphi technique as a forecasting tool: issues and analysis. Int J Forecast 15: 353-375.
- F Hasson, S Keeney, H McKenna (2000) Research guidelines for the Delphi survey technique. J Adv Nurs 32: 1008-1015. [Crossref]
- David Nott (2019) War Doctor: Surgery on the Front Line. Picador.
- Surgical Training for Austere Environments (2016) R Coll Surg.
- J Gilbody, A W Prasthofer, K Ho, M L Costa (2011) The use and effectiveness of cadaveric workshops in higher surgical training: a systematic review. Ann R Coll Surg Engl 93: 347-352. [Crossref]
- Definitive Surgical Trauma Skills (DSTS). (2020) R Coll Surg Engl.
- G W McGarry, D Aitken (1991) Intranasal balloon catheters: how do they work? Clin Otolaryngol Allied Sci 16: 388-392. [Crossref]
- A J Gibbons, N Mackenzie, R S Breederveld (2011) Use of a custom designed external fixator system to treat ballistic injuries to the mandible. Int J Oral Maxillofac Surg 40: 103-105. [Crossref]
- Raja Kummoona (2011) Management of maxillofacial injuries in Iraq. J Craniofac Surg 22: 1561-1566. [Crossref]
- Michael Perry, Simon Holmes (2014) Atlas of Operative Maxillofacial Trauma Surgery: Post-traumatic Deformity. Springer.
- Review W P (2019) Libya Population 2019.
- David J Thurman, Clinton Alverson, Doug Browne, Kathleen A Dunn, Janet Guerrero et al. (1999) Traumatic brain injury in the United States; a report to Congress.
- James D Westwood (2011) Battlefield tracheal intubation training using virtual simulation: a multi center operational assessment of video laryngoscope technology. Medicine Meets Virtual Reality 18: NextMed 163: 74.
- Michael B Shvyrkov (2013) Facial gunshot wound debridement: Debridement of facial soft tissue gunshot wounds. J CranioMaxillofac Surg 41: e8-e16. [Crossref]
- Michael Perry, Simon Holmes (2014) Atlas of operative maxillofacial trauma surgery: primary repair of facial injuries. Springer.
- B Kirwan (1994) A guide to practical human reliability assessment. CRC press.
- Christopher Partyka (2014) Anatomy of the orbital compartment.
