Torsional Stability of a Chevron Interface for Intercalary Allograft Fixation of the Femur
A B S T R A C T
Intercalary allografts are frequently used for diaphyseal long bone reconstruction following tumor resection. Torsional stability between allograft and host bone is an important factor in achieving osseous union at the interface and reducing fracture risk of the allograft. The purpose of this study was to evaluate the torsional stability of an intercalary allograft construct using a new chevron type of osteotomy. The torsional load of up to 4.0 Nm in both directions were applied to six matching pairs of fresh frozen cadaveric femurs, reconstructed using either a 60-degree chevron or a modified step-cut interface. The torsional stiffness of the construct and the interface rotation were compared between the two groups. The results showed that a construct with a 60-degree chevron interface had comparable interface rotations and stiffness as those with the modified step-cut interface. However, the large inter-specimen variations observed in rotation results of the modified step-cut suggest higher technical requirements associated with this procedure. The study also revealed a trend towards improved torsional stiffness with increased axial load of the chevron construct, combined with its 55% more surface area across the graft-host interface over the modified step-cut, which prove that 60-degree chevron interface may serve as a good alternative in intercalary allograft fixation.
Keywords
Intercalary allograft, torsional stability, implant fixation, tumor resection, limb-salvage
Introduction
Intercalary allografts have been used for diaphyseal long bone reconstructions following tumor resection for nearly a century [1]. Previous studies have shown that these reconstructions usually provide good to excellent results [1-9]. Mankin and colleagues, who reported the largest series of allograft replacements, demonstrated a 75% rate of successful outcome and graft retention at 20 years follow-up [7]. The three main causes for the 25% failure rate in the series were fractures, nonunions, and infections [1, 4, 10]. Studies have demonstrated that both nonunion and fracture rates are significantly affected by the method of fixation used [1, 2, 6-16]. An intramedullary (IM) nail allograft-host fixation has been demonstrated to resist axial load well, but weak in resisting rotational loads [9, 17, 18]. To combat this, various step-cut configurations have been suggested with some success. More recently, a modified step-cut has been shown to provide greater torsional stability when compared to the traditional step-cut [12, 18, 19]. However, the modified step-cut is a demanding procedure. In addition to the technical challenge of performing the modified step-cut, the rate of fracture failure of 43% has been reported with the 2 mm modified step-cut [18]. The objective of the study is to compare the allograft-host interface torsional stability of a 60-degree chevron type osteotomy to the 2 mm modified step-cut osteotomy in a cadaveric model and to examine the potential effect of the axial compressive preload on the interface stability.
Methods
Six matched pairs of adult fresh-frozen cadaveric femurs were retrieved for the study and assigned to two matched study groups based on the type of graft-host interface - Group 1: 60-degree chevron (Chevron), and Group 2: modified step-cut (ModStep). Prior to creating the osteotomies, each femur was reamed and instrumented with either 12 mm or a 13 mm AO (Synthes, USA, Paoli, PA) retrograde IM nail following the manufacturer's guideline. Two distal locking screws were placed statically. A single proximal interlocking screw, positioned in the dynamic slot of the nail, was placed after the osteotomies had been performed. We chose this configuration to ensure that the IM nail provided the minimal contribution to the torsional stability of the construct while maintaining the basic integrity between the proximal and distal fragments and allowing axial compression. Next, the IM nail hardware was removed, and the osteotomies were created 10 cm apart, centered about the mid-shaft of the femur, within the femoral diaphysis.
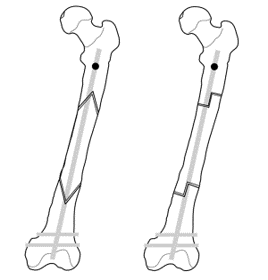
For Group 1, the chevron osteotomy was created with a 60-degree angle between limbs of the osteotomy, with the apex centered within the diaphysis and the limb lengths equal at the outer cortex of the femoral diaphysis. The apices of the chevron osteotomies were oriented away from the intercalary segment of the femoral bone (Figure 1). For Group 2, the modified step-cut was performed by initially creating transverse osteotomies. This was followed by 1 cm step-cut resection of bone with the proximal sagittal line drawn 2 mm lateral to the mid-sagittal plane, and the distal sagittal line drawn 2 mm medial to the mid-sagittal plane. The offset sagittal plane osteotomy will theoretically improve compressive force across the vertical interfaces of the osteotomy. For both groups, templates were prepared as a guide for cutting. A bone file was used to remove minor imperfections in the osteotomy interface, and to assure optimum congruence between interface surfaces. The previously placed IM nail was then reinserted, with replacement of the static distal interlocking screws and a single dynamically placed proximal interlock screw positioned with fluoroscopic imaging using the perfect circle technique.
Figure 1: Illustration of the two study groups: 60-degree Chevron (left) and modified step-cut (right).
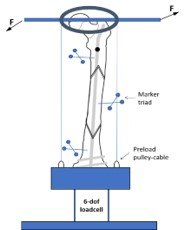
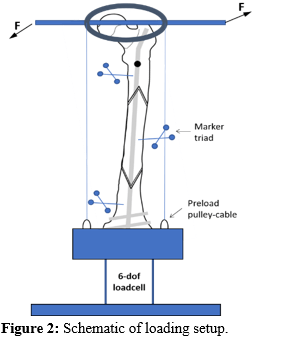
Each femur was then potted vertically in dental cement with a 10-degree valgus angle and mounted on a customized loading frame. Coupled static loads were applied to the proximal femur through a cable-pulley system to generate a torque up to 4.0 Nm in five steps (0.5, 1.0, 2.0, 3.0, and 4.0 Nm), in the directions of left and right axial rotation. To measure the relative rotation at the graft-host bone interface with each step of loading, a set of three reflective markers from a motion analysis system (Optotrak Certus, Northern Digital Inc, Waterloo, Ontario, Canada) was mounted on the proximal, middle (bone graft), and distal segments of the femur (Figure 2). To evaluate the effect of partial weight-bearing on the torsional stability of the interface, this experiment was repeated three times under a compressive preload of 10 lbs, 20 lbs, and 40 lbs. The range of motion between the proximal and distal segments (across the graft and two graft-host interfaces) was determined by combining the rotation angles during the left and right rotations.
Figure 2: Schematic of loading setup.
Rotations at each of the two interfaces were also determined to evaluate the distribution of the motion. Construct stiffness was derived from the linear portion of the load-displacement curve. Matched pair comparisons were made between the Chevron and ModStep groups. The two-tailed Wilcoxon signed-rank test was chosen due to a small sample size. A secondary comparison was made within each interface group to evaluate the influence of axial preload, using repeated measure ANOVA. All statistical analysis was conducted using software JMP 12 (SAS Institute Inc, Cary, NC), with statistical significance set to p<0.05.
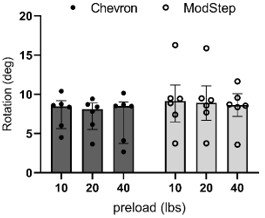
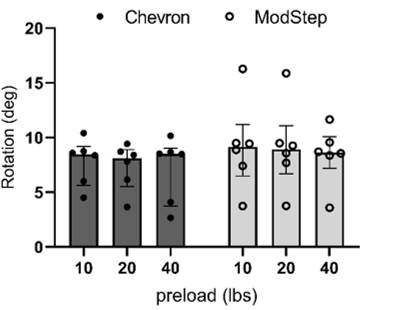
Figure 3: The median (inter-quartile range and individual datapoints) of the combined rotation across the two graft-host interfaces under 4 Nm torque at three preloads for the 60-degree chevron group and modified step cut group.
Results
Under the torsional load of 4 Nm in both directions, the median (range) of combined rotation across the proximal and distal graft-host interfaces for the Chevron group were 8.5 (4.5-10.4) degrees at 10lbs preload, 8.1 (3.7-9.4) degrees at 20lbs and 8.5 (2.7-10.2) degrees at 40lbs. For the ModStep group, the median (range) of combined rotation at the three preloads were 9.1(3.7-16.3), 8.9 (3.8-15.9), and 8.6 (3.6-11.7) degrees respectively (Figure 3). The ModStep group showed much larger inter-specimen variations than the Chevron group, indicated by the large range (10.9 versus 6.4 degrees) and standard deviation (3.6 vs. 2.4 degrees).
The median rotations of the ModStep group were slightly higher (less than 10%) than Chevron at all three preload levels, but none of the differences was statistically significant. The increase in the compressive preload had no influence on the range of motion for either Chevron group or ModStep group.
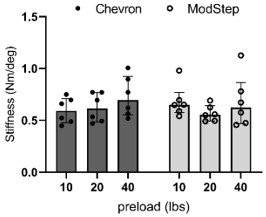
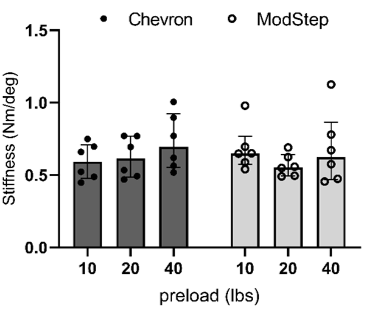
Figure 4: The median (interquartile range and individual datapoints) of the construct stiffness at three preload levels for the 60-degree chevron group and modified step cut groups.
Discussion
Limb sparing surgery has become more important as newer therapies continue to prolong the lives of cancer patients. Fractures and nonunions of intercalary allografts cause a high rate of revision surgeries and even amputations. Creating a construct that can lower the rates of these two complications may significantly decrease the morbidity and cost associated with limb-sparing surgery.
In this study, we proposed a novel chevron type intercalary interface that increases the surface area available for healing and improve the torsional stability of the construct. Findings from this study reveal that a construct with a 60-degree chevron interface has comparable interface rotation and stiffness as the modified step-cut construct. The results also show a trend of improved torsional stiffness of the 60-degree chevron construct with increasing axial load. Although not clinically proven by this biomechanical cadaveric study, the stability offered by the 60-degree chevron osteotomy may correlate with improved torsional stiffness during clinical weight-bearing activities.
Previously, Van Boerum et al. compared rotational stability of 2 mm modified step-cut to conventional step-cut in a similarly loaded cadaver model [9]. The magnitude of the applied torque was half the level as the present study, and the only interface was included in the model. The mean (±SD) rotation under 2 Nm torque was 3.0 (±4.6) degrees. The present cadaver model, incorporating both interfaces of the intercalary bone graft, found the total interface rotation to be 8.6 to 9.1 degrees under 4 Nm torque. Taking into account the above-mentioned differences, the two studies are in good agreement. In addition, both studies showed large inter-specimen variations in rotation with the modified step-cut construct.
The 60-degree chevron osteotomy provides a larger contact area of the allograft to the host bone than the modified step-cut. This finding is based on the mid-shaft dimension of the cadaver femoral model used in our study. The contact area of 12.6 cm2 for the 60-degree chevron is 55% greater than the modified step-cut method. In the immediate post-operative period, the larger contact area enhances torsional resistance through friction. But more importantly, the greater surface area under load accelerates the bone healing and incorporation of the intercalary allograft to the host bone.
The limitations of the study include small sample size, and the potential for mismatch between femoral rod and cadaveric femur. Rod diameter was selected during specimen preparation, based on reamer chatter during canal reaming. Several factors including bone quality, canal diameter, sharpness of the reamer, and reamer speed add potential sources of variation in the selection of the rod for each femoral specimen. The dynamic screw in the proximal aspect of the femur is a factor that may have obscured the differences in torsional control between the constructs because some degree of torsional stiffness is inherent in the nail itself. This may have concealed the true differences in osteotomy stability. On the other hand, interlocking nails are often used in intercalary reconstruction. Therefore, these models are fair representations of clinical practice.
In conclusion, the present study confirms the equivalent torsional stability of the 60-degree chevron osteotomy and the 2 mm modified step-cut osteotomy. The greater contact area of the 60-degree chevron osteotomy yields a larger surface for one healing. Further clinical studies are needed to demonstrate the contribution of the increased surface area to improved union rate of the 60-degree chevron osteotomy.
Acknowledgements
The study was supported in part by the Musculoskeletal Transplant Foundation.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 15, Jan 2020Accepted: Mon 03, Feb 2020
Published: Wed 12, Feb 2020
Copyright
© 2023 Mei Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSO.2020.01.03
Author Info
Jeremy P Zebroski Donald A Hackbarth Jr Mei Wang Sean C Tracy
Corresponding Author
Mei WangDepartment of Orthopaedic Surgery, Medical College of Wisconsin, Milwaukee, Wisconsin, USA
Figures & Tables
References
- Mankin HJ, Doppelt S, Tomford W (1983) Clinical experience with allograft implantation. The first ten years. Clin Orthop Relat Res 174: 69-86. [Crossref]
- Brigman BE, Hornicek FJ, Gebhardt MC, Mankin HJ (2004) Allografts about the Knee in Young Patients with High-Grade Sarcoma. Clin Orthop Relat Res 421: 232-239. [Crossref]
- Chang DW, Weber KL (2004) Segmental femur reconstruction using an intercalary allograft with an intramedullary vascularized fibula bone flap. J Reconstr Microsurg 20: 195-199. [Crossref]
- DiCaprio MR, Friedlaender GE (2003) Malignant bone tumors: limb sparing versus amputation. J Am Acad Orthop Surg 11: 25-37. [Crossref]
- Dion N, Sim FH (2002) The use of allografts in musculoskeletal oncology. Instr Course Lect 51: 499-506. [Crossref]
- Fox EJ, Hau MA, Gebhardt MC, Hornicek FJ, Tomford WW et al. (2002) Long-term followup of proximal femoral allografts. Clin Orthop Relat Res 397: 106-113. [Crossref]
- Mankin HJ, Gebhardt MC, Jennings LC, Springfield DS, Tomford WW (1996) Long-term results of allograft replacement in the management of bone tumors. Clin Orthop Relat Res 324: 86-97. [Crossref]
- Ortiz Cruz E, Gebhardt MC, Jennings LC, Springfield DS, Mankin HJ et al. (1997) The results of transplantation of intercalary allografts after resection of tumors. A long-term follow-up study. J Bone Joint Surg Am 79: 97-106. [Crossref]
- Vander Griend RA (1994) The effect of internal fixation on the healing of large allografts. J Bone Joint Surg Am 76: 657-663. [Crossref]
- Gebhardt MC, Flugstad DI, Springfield DS, Mankin HJ (1991) The use of bone allografts for limb salvage in high-grade extremity osteosarcoma. Clin Orthop Relat Res 270: 181-196. [Crossref]
- Cara JA, Lacleriga A, Canadell J (1994) Intercalary bone allografts. 23 tumor cases followed for 3 years. Acta Orthop Scand 65: 42-46. [Crossref]
- Moran MC (1995) Postoperative fracture of the host femur in allograft-prosthetic reconstruction of the hip. J Arthroplasty 10: 550-553. [Crossref]
- Muir P, Johnson KA (1995) Tibial intercalary allograft incorporation: comparison of fixation with locked intramedullary nail and dynamic compression plate. J Orthop Res 13: 132-137. [Crossref]
- Hornicek FJ, Gebhardt MC, Tomford WW, Sorger JI, Zavatta M et al. (2001) Factors affecting nonunion of the allograft-host junction. Clin Orthop Relat Res 382: 87-98. [Crossref]
- Sorger JI, Hornicek FJ, Zavatta M, Menzner JP, Gebhardt MC et al. (2001) Allograft fractures revisited. Clin Orthop Relat Res 382: 66-74. [Crossref]
- Stevenson S, Emery SE, Goldberg VM (1996) Factors affecting bone graft incorporation. Clin Orthop Relat Res 324: 66-74. [Crossref]
- Kohles SS, Markel MD, Rock MG, Chao EY, Vanderby R Jr. (1994) Mechanical evaluation of six types of reconstruction following 25, 50, and 75% resection of the proximal femur. J Orthop Res 12: 834-843. [Crossref]
- Van Boerum DH, Randall RL, Mohr RA, Conrad EU, Bachus KN (2003) Rotational stability of a modified step-cut for use in intercalary allografts. J Bone Joint Surg Am 85: 1073-1078. [Crossref]
- Markel MD, Wood SA, Bogdanske JJ, Rapoff AJ, Kalscheur VL et al. (1995) Comparison of allograft/endoprosthetic composites with a step-cut or transverse osteotomy configuration. J Orthop Res 13: 639-641. [Crossref]