Journals
Tight Junction Protein Junctional Adhesion Molecule-A Regulates the Expression of Receptor Tyrosine Kinase EPHA2 In Triple-Negative Breast Cancer Cells
A B S T R A C T
Breast tumors lacking expression of the human epidermal growth factor receptor-2 (HER2), progesterone receptor (PR) and estrogen receptor (ERα) are defined as triple negative breast cancers (TNBC). A lack of targeted therapies has impaired TNBC patient prognosis. It has previously been shown that high expression of Junctional Adhesion Molecule-A (JAM-A) correlates with aggressive breast cancer patient phenotypes, and that JAM-A regulates the expression of HER2 in breast cancer cells. Accordingly, we hypothesized that JAM-A might regulate the expression of other receptor tyrosine kinases. We show for the first time that JAM-A may regulate the expression of the EPHA2 receptor in TNBC cells and propose that this pathway merits deeper investigation for its therapeutic value in TNBC settings.
Keywords
Triple-negative breast cancer,tumor,tetrocarcin-A,JAM-A,EPHA2,ZO-1,cell viability,anti-tumor,tight junction
Introduction
Tumors lacking the expression of HER2, PR and ERα are defined as triple negative breast cancers (TNBC). Due to a lack of targeted therapies the standard of care for treating TNBC patients during early and advanced stage of the disease is chemotherapy [1]. However, TNBC patients frequently develop resistance to chemotherapeutic drugs relatively quickly, leading to an early demise. The lack of targeted therapies and poor prognosis of patients with TNBC have fostered a major effort to discover actionable molecular targets to treat patients with these tumours [1]. In the present study we extend prior work proposing that the tight junction protein Junctional Adhesion Molecule-A (JAM-A) is a potential therapeutic target in TNBC settings. High JAM-A high expression has previously been correlated with aggressive disease and poor outcome in breast cancer patients [2, 3]. Furthermore, we have shown that JAM-A regulates the expression of the receptor tyrosine kinase HER2 in breast cancer cells [4].
We therefore hypothesized JAM-A might regulate the expression of other oncogenic receptor tyrosine kinases. In this manuscript we describe the EPHA2 receptor as a target of JAM-A in TNBC cells. EPHA2 belongs to the Ephrin family of receptor tyrosine kinases and is enriched in TNBC cells; in which EPHA2 targeting impairs cell cycle progression and inhibits cell growth [5, 6]. The epidermal growth factor receptor (EGFR) which is highly expressed in TNBC cells has been shown to interact with and activate EPHA2, and activated EPHA2 has been described to amplify pro-tumorigenic MAPK, AKT and Rho family GTPase signalling [5, 7, 8]. In our study, both the JAM-A-downregulating natural compound Tetrocarcin-A and siRNA against JAM-A downregulated EPHA2 protein expression [9, 10]. JAM-A and EPHA2 were further found to co-localize and co-precipitate. Since JAM-A regulates the expression of EPHA2 in TNBC cells, and EPHA2 regulates cell survival pathways, we propose that JAM-A merits further investigation as a potential target in TNBC settings.
Methods
I Cells
The human breast cancer cell line HCC38 was cultured in RPMI medium (Sigma-Aldrich) supplemented with 10% foetal bovine serum, 100U/ml penicillin and 100μg/ml streptomycin.
II Transfections
HCC38 cells were transfected for 72h with 25nM of control siRNA (siGENOME non-targeting siRNA #1, Dharmacon) or JAM-A siRNA (SASI_Hs01_00048785, Sigma-Aldrich) to silence JAM-A gene expression. Transfections were carried out using Lipofectamine-2000 (ThermoFisher Scientific) as per manufacturer's instructions.
III Drug treatment
HCC38 triple negative breast cancer cells were plated in 6-well plates and treated 24h later with 2.5μM Tetrocarcin-A or vehicle (0.01 % v/v DMSO) for 24h.
IV Electrophoresis and Western blot analysis
Whole cell lysates were prepared from breast cancer cells using lysis buffer composed of 0.1M KCl, 2.5mM NaCl, 3.5mM MgCl2, 10mM HEPES pH7.4, 1% Triton-X100, protease and phosphatase inhibitor cocktails (Sigma). Cells were lysed via trituration, whereupon extracts were centrifuged at 1,500xg for 5min at 4°C and supernatants stored at -20°C. Protein content was quantified via bicinchoninic (BCA) assay (Thermo Scientific), whereupon 15μg protein/lane was subjected to reducing SDS-PAGE, transferred to nitrocellulose membranes at 100V for 75min and immunoblotted with the antibodies to human JAM-A (BD Bioscience), EPHA2 (R&D Systems) and β-actin (Abcam).
V Immunofluorescence staining
HCC38 cells were fixed in 100% ice cold ethanol (Sigma), blocked for 30 min with 3% BSA and incubated with primary antibodies to human JAM-A (1:100, Santa Cruz), EPHA2 (1:100, R&D Systems) and ZO-1 (1:100, Life Technologies). These were subsequently detected with secondary anti-mouse 488/anti-goat 568 or anti-mouse 488/anti-rabbit 568 or anti-goat 488/anti-rabbit 568 and mounted in medium containing DAPI (Vectashield, Vector Laboratories). Laser scanning confocal microscopy was performed using the Zeiss LSM 710 confocal system. Images were acquired using a 40X oil-immersion objective, and image averaging was applied to reduce noise.
VI Co-immunoprecipitation
HCC8 cell lysates were prepared from T75 flasks using lysis buffer composed of 0.1M KCl, 2.5mM NaCl, 3.5mM MgCl2, 10mM HEPES pH 7.4, 1% Triton-X100, protease and phosphatase inhibitor cocktails (Sigma). Cells were lysed via trituration, whereupon extracts were centrifuged at 1,500xg for 5min at 4°C and supernatants stored at -20°C. Protein content was quantified via bicinchoninic (BCA) assay (Thermo Scientific). 1 mg of total protein was used for immunoprecipitation. Protein G beads (Sigma), anti-human JAM-A (Santa Cruz) and IgG (Sigma) were used for immunoprecipitation of the HCC38 cell lysate. Precipitates were then subjected to reducing SDS-PAGE, transferred to nitrocellulose membranes at 100V for 75min and immunoblotted with the antibodies to human JAM-A (BD Bioscience), EPHA2 (R&D Systems) and probed with secondary goat anti-mouse HRP (Sigma) or donkey anti-goat HRP (R&D Systems) antibodies.
Results
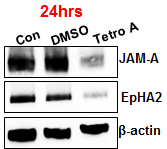
Targeting of JAM-A caused downregulation of EPHA2
Several studies have shown that expressional or functional reductions in the adhesion protein JAM-A inhibit proliferation of several types of cancer cells [3, 11]. In the TNBC setting, we previously noted that JAM-A silencing or exposure to the JAM-downregulating compound Tetrocarcin-A reduced the proliferation of HCC38 TNBC cells [10]. Since JAM-A expression has been shown to regulate the expression of HER2 in breast cancer cells, in this manuscript we sought to uncover if JAM-A regulates the expression of other receptor tyrosine kinases relevant to TNBC settings [4].
HCC38 cells were seeded in 6 well plates and either gene-silenced for 72h with 25nM siRNA to JAM-A versus negative control siRNA (a) or treated for 24h with the JAM-downregulating compound Tetrocarcin-A (The NCI/DTP Open Chemical Repository; 2.5μM) versus vehicle (0.01 % v/v DMSO) (b). Cell extracts were prepared and Western blotted for human JAM-A, EPHA2 and β-actin.
Figure 2: JAM-A and EPHA2 colocalize at the cell membrane
HCC38 cells were plated on 13 mm coverslips and subjected to double immunofluorescence staining with antibodies to JAM-A/EPHA2, JAM-A/ZO-1 or EPHA2/ZO-1. Images were acquired on an LSM710 confocal microscope.
Discussion and Conclusions
Breast cancer incidence is increasing throughout the world every year, although the mortality rates continually drop due in part to the availability of targeted therapies for HER2 or ERα positive breast cancer patients [15]. However, TNBCs, which compromise 10-15% of all breast cancer cases, retain high mortality rates due to the lack of actionable targets on the surface of their tumor cells. In the current study we propose the tight junction protein JAM-A merits consideration for potential therapeutic value in TNBC settings. Under normal circumstances JAM-A plays important physiological functions in numerous processes including intercellular tight junction assembly, cellular polarity, leukocyte transmigration, platelet activation, angiogenesis and cell morphology [16]. However, dysregulation of JAM-A expression or function has been increasingly implicated in various pathologies including cancer progression [17].
Importantly, high JAM-A expression has been correlated with aggressive disease and poor outcome in breast cancer patients [2, 3]. Since JAM-A regulates the expression of the receptor tyrosine kinase HER2 in breast cancer cells, we hypothesized that JAM-A might regulate other receptor tyrosine kinases relevant to TNBC settings [4]. A receptor tyrosine kinase PCR array identified the oncogenic receptor tyrosine kinase EPHA2 as a target of JAM-A. EPHA2 belongs to the Ephrin family, is enriched in TNBC cells, and its targeting has been shown to impair cell cycle progression and inhibit TNBC cellular growth [5, 6]. Having validated this at protein level and noted that both JAM-A and EPHA2 contain a PDZ-binding motif, we reasoned that JAM-A and EPHA2 might interact through PDZ domain-containing proteins at the tight junction [12, 13]. Accordingly, JAM-A and EPHA2 were noted to colocalize with the PDZ protein ZO-1; which was further validated by immunoprecipitation (preliminary data not shown). Since JAM-A regulates the expression of EPHA2 in TNBC cells and EPHA2 regulates cell survival pathways, we submit that JAM-A merits further investigation as a potential target in TNBC settings [5].
Acknowledgements
This research arose from research conducted with the financial support of Science Foundation Ireland (SFI) under grant number 13/IA/1994 (to AMH). The LSM710 confocal microscope was supported through the National Biophotonics and Imaging Platform, Ireland, and funded by the Irish Government's Programme for Research in Third Level Institutions, Cycle 4, Ireland’s EU Structural Funds Programmes 2007-2013. We thank the NCI/DTP Open Chemical Repository https://dtp.cancer.gov for the opportunity to work with Tetrocarcin-A (NSC 333856).
Conflicts of Interest
The authors declare no conflict of interest
Article Info
Article Type
Short CommunicationPublication history
Received: Wed 03, Jul 2019Accepted: Fri 26, Jul 2019
Published: Sat 10, Aug 2019
Copyright
© 2023 Ann M. Hopkins. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2019.04.01
Author Info
Sri HariKrishna Vellanki Viviana Bustos Brian J. Harvey Ann M. Hopkins
Corresponding Author
Ann M. HopkinsDepartment of Surgery, Royal College of Surgeons in Ireland, Dublin, Ireland
Figures & Tables


References
- Bianchini G, Balko JM, Mayer IA, Sanders ME, Gianni L (2016) Triple-negative breast cancer: challenges and opportunities of a heterogeneous disease. Nat Rev Clin Oncol 13: 674-690. [Crossref]
- McSherry EA, McGee SF, Jirstrom K, Doyle EM, Brennan DJ et al. (2009) JAM-A expression positively correlates with poor prognosis in breast cancer patients. Int J Cancer 125: 1343-1351. [Crossref]
- Murakami M, Giampietro C, Giannotta M, Corada M, Torselli I et al. (2011) Abrogation of junctional adhesion molecule-A expression induces cell apoptosis and reduces breast cancer progression. PLoS One 6: e21242. [Crossref]
- Brennan K, McSherry EA, Hudson L, Kay EW, Hill AD et al. (2013) Junctional adhesion molecule-A is co-expressed with HER2 in breast tumors and acts as a novel regulator of HER2 protein degradation and signaling. Oncogene 32: 2799-2804. [Crossref]
- Song W, Hwang Y, Youngblood VM, Cook RS, Balko JM et al. (2017) Targeting EPHA2 impairs cell cycle progression and growth of basal-like/triple-negative breast cancers. Oncogene 36: 5620-5630. [Crossref]
- Tsouko E, Wang J, Frigo DE, Aydogdu E, Williams C (2015) miR-200a inhibits migration of triple-negative breast cancer cells through direct repression of the EPHA2 oncogene. Carcinogenesis 36: 1051-1560. [Crossref]
- Changavi AA, Shashikala A, Ramji AS (2015) Epidermal Growth Factor Receptor Expression in Triple Negative and Nontriple Negative Breast Carcinomas. J Lab Physicians 7: 79-83. [Crossref]
- Larsen AB, Pedersen MW, Stockhausen MT, Grandal MV, van Deurs B et al. (2007) Activation of the EGFR gene target EPHA2 inhibits epidermal growth factor-induced cancer cell motility. Mol Cancer Res 5: 283-293. [Crossref]
- Vellanki SH, Cruz RGB, Jahns H, Hudson L, Sette G et al. (2019) Natural compound Tetrocarcin-A downregulates Junctional Adhesion Molecule-A in conjunction with HER2 and inhibitor of apoptosis proteins and inhibits tumor cell growth. Cancer Lett 440-441: 23-34. [Crossref]
- Vellanki SH, Cruz RGB, Richards CE, Smith YE, Hudson L et al. (2019) Antibiotic Tetrocarcin-A Down-regulates JAM-A, IAPs and Induces Apoptosis in Triple-negative Breast Cancer Models. Anticancer Res 39:1197-1204. [Crossref]
- Goetsch L, Haeuw JF, Beau-Larvor C, Gonzalez A, Zanna L et al. (2013) A novel role for junctional adhesion molecule-A in tumor proliferation: modulation by an anti-JAM-A monoclonal antibody. Int J Cancer 132: 1463-1474. [Crossref]
- Severson EA, Parkos CA (2009) Mechanisms of outside-in signaling at the tight junction by junctional adhesion molecule A. Ann N Y Acad Sci 1165: 10-18. [Crossref]
- Pasquale EB (2010) Eph receptors and ephrins in cancer: bidirectional signalling and beyond. Nat Rev Cancer 10: 165-180. [Crossref]
- Ebnet K, Schulz CU, Meyer Zu Brickwedde MK, Pendl GG, Vestweber D (2000) Junctional adhesion molecule interacts with the PDZ domain-containing proteins AF-6 and ZO-1. J Biol Chem 275: 27979-27988. [Crossref]
- Yin L, Shuang H, Sheng C, Liang H, Sun XJ et al. (2018) The Prognostic Value of Nodal Staging in Triple-Negative Breast Cancer - A Cohort from China. Sci Rep 8:9007. [Crossref]
- Leech AO, Cruz RG, Hill AD, Hopkins AM (2015) Paradigms lost-an emerging role for over-expression of tight junction adhesion proteins in cancer pathogenesis. Ann Transl Med 3: 184. [Crossref]
- Zhao C, Lu F, Chen H, Zhao X, Sun J et al. (2014) Dysregulation of JAM-A plays an important role in human tumor progression. Int J Clin Exp Pathol 7: 7242-7248. [Crossref]
