There is a Correlation between Fragility Fractures of the Pelvis and a Circle-Type Morphology of the True Pelvis, but Not with Pelvic Incidence
A B S T R A C T
Purpose: Osteoporosis is a major risk factor for the development of fragility fractures of the pelvis (FFP). There is a lack of information about the influence of anatomical conditions such as Pelvic Incidence and Pelvic Ratio (DT/DS ratio) on this kind of fractures.
Methods: This is a monocentric retrospective analysis. X-ray images of the lumbar spine and pelvis and 3D-MPR CT reconstructions of the pelvis were analysed to determine Pelvic Incidence (PI) and Pelvic Ratio (PR) in 141 fragility fractures of the pelvis. Statistical analyses were performed to examine the correlation between these spinopelvic parameters and fragility fractures of the pelvis.
Results: A total of 141 fragility fractures of the pelvis (14 men = 9.93%, 127 women = 90.07%) were analysed. According to the FFP-classification we recognized FFP type 1 fractures in 19.15%, FFP type 2 in 41.13%, FFP type 3 in 8.51% and FFP type 4 fractures in 32.21%. The mean PI was 58.83º. There was no statistical correlation between PI and fracture types (p=0.81). The mean PR was 1.099. 57 patients (40.43%) demonstrated a DT/DS ratio ≤ 1.06, corresponding to a circle-type morphology. 24 patients (17.02%) demonstrated a DT/DS ratio ≥ 1.18, corresponding to an ellipse-type pelvis. A circle-type pelvis is significantly more often associated with fragility fractures of the pelvis than an ellipse-type morphology (p<0.001).
Conclusion: The results of our work demonstrate a strong statistical correlation between the circle-type morphology of the pelvis (PR ≤ 1.06) and fragility fractures of the pelvis. There is no statistical correlation between fragility fractures of the pelvis and Pelvic Incidence.
Keywords
Fragility fractures of the pelvis, pelvic incidence, pelvic ratio, osteoporotic pelvic ring fracture
Introduction
Fragility fractures of the pelvis represent an increasing focus in geriatric trauma centers. The need for an interdisciplinary treatment and proper indication for non-operative therapy or surgery is the subject of the current literature. This is well-founded in significant 1-year mortality, which is up to 27%, and the level of activity and desired quality of life in the elderly [1-3]. It has been proven that osteoporosis is a major risk factor for the development of these fractures. 60% of the fragility fractures of the pelvis are caused by osteoporosis [2-5]. To the authors’ opinion, it has not been sufficiently investigated if further and what kind of factors influence the development and course of these fractures. We analysed the influence of Pelvic Incidence (PI) and Pelvic Ratio (PR) on fragility fractures of the pelvis (FFP).
Materials and Methods
This is a single-center retrospective study of patients who had to undergo inpatient treatment for fragility fractures of the pelvis at a local trauma center and center for geriatric medicine from January 2017 to December 2019. General patient data (sex, age) were obtained from the electronic patient file. X-ray images of the lumbar spine and pelvis and CT images of the pelvis, including 3-dimensional multiplanar reconstructions (3D-MPR) were analysed by the authors. Fractures were classified according to FFP-classification (fragility fractures of the pelvis classification) [6]. PI and PR were determined on an approved diagnostic monitor using radiological software (Sectra Workstation PACS IDS7, Sectra AB). The ratio of the diameter of transverse true pelvis (DT) and diameter of the sagittal true pelvis (DS) was calculated to classify the circle-type and ellipse-type morphology of the pelvis [7]. Statistical tests (t-test for unequal variances, one-way analysis of variance) were performed to examine the correlation between FFP, PI and PR.
I Patients
i. Treatment period: January 2017-December 2019.
ii. Inclusion criterion: patients aged ≥ 65 years with fragility fractures of the pelvis.
iii. Exclusion criterion: patients aged < 65 years, polytrauma, ISS> 16, fall> 1m, traffic accident.
iv. Fracture classification: FFP-classification [6].
II Evaluation of Pelvic Incidence
PI was determined using the measurement tools of the Sectra Workstation software in a standard fashion [8]. Due to different image qualities, the femoral heads were not always overlapping. In these cases, the center of the bicoxofemoral axis was determined for PI measurement.
III Evaluation of Pelvic Ratio
PR (DT/DS ratio) was determined using CT-3D-MPR and measurement tools of the Sectra Workstation software according to Lee et al. The classification of the pelvic morphology was made according to this publication into a circle-type and an ellipse-type of the pelvis [7].
IV Statistical Analyses
The following statistical analyses were performed:
i. Correlation between sex and FFP (t-test for unequal variances).
ii. Correlation between PI and fracture type (one-way analysis of variance-ANOVA).
iii. Correlation between PR and fracture type (one-way analysis of variance-ANOVA).
iv. Correlation between circle-type/ellipse-type and FFP (t-test for unequal variances).
Results
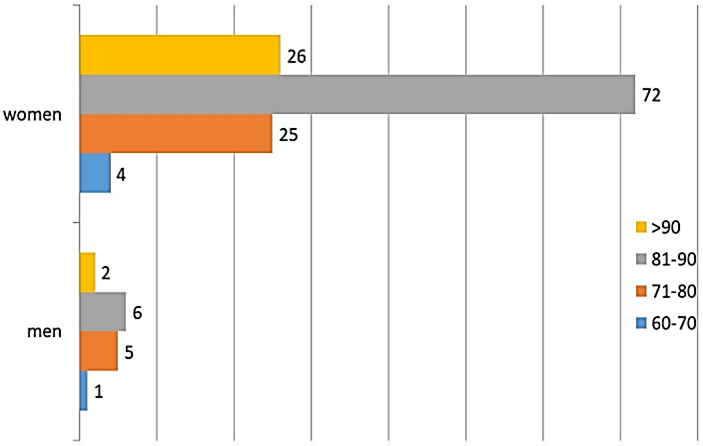
From January 2017 to December 2019, a total of 141 patients (14 men = 9.93%, 127 women = 90.07%) underwent inpatient treatment of fragility fractures of the pelvis. The mean age was 84.87 years (xmed: 86 years; 65-102 years). The mean age of the men was 81.5 years (65-94 years). The mean age of the women was 85 years (65-102 years). There was no statistically significant difference in age in the two groups (t-test for unequal variances: p = 0.14) (Figure 1).
Figure 1: Sex and age distribution (n=141 patients).
I Distribution of Fracture Types (According to FFP-Classification)
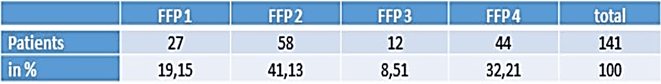
FFP type 2 fractures were the most common fractures with 41%, followed by FFP`` type 4 fractures with 32%. FFP type 1 fractures were found in 19%. FFP type 3 fractures were the least represented with 8.5% (Tables 1 & 2).
Table 1: Frequency and distribution of FFP-types.
Table 2: Frequency and distribution of FFP-subtypes.
II Correlation between Pelvic Incidence and FFP-Type
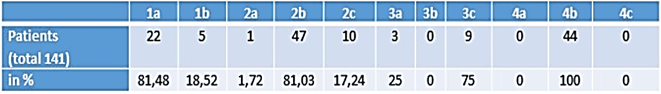
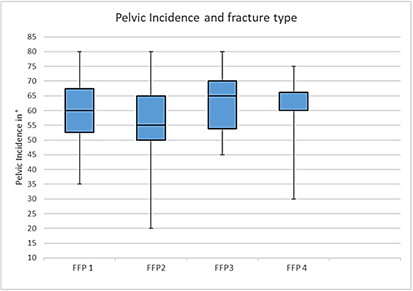
Patients with FFP type 1 fractures had a mean PI of 60º (± 10.46º). Patients with FFP type 2 fractures had a mean PI of 56.8º (± 11.26º). Patients with FFP type 3 fractures demonstrated a mean PI of 62.08º (± 10.96º). Patients with FFP type 4 fractures had a mean PI of 59.65º (± 9.78º). There is no statistically significant correlation between PI and FFP-types (ANOVA, p = 0.81) (Figure 2) (Table 3).
Figure 2: Boxplot to demonstrate the correlation of PI and FFP-types.
Table 3: PI and FFP-types.
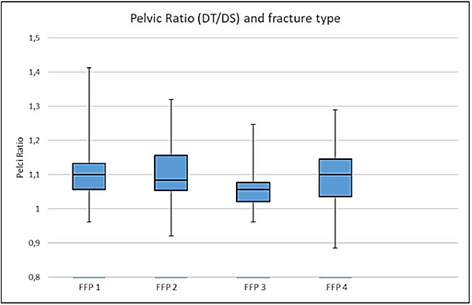
III Relationship between Pelvic Ratio (DT/DS Ratio) and Fracture Type
The average DT/DS ratio was 1.099 (95% CI:1.08-1.11). Patients with FFP type 1 fractures had a mean PR of 1.10 (± 0.07), patients with FFP 2 fractures of 1.10 (± 0.04), patients with FFP 3 fractures of 1.06 (± 0.08) and patients with FFP type 4 fractures had a mean PR of 1.09º (± 0.04). There is no statistically significant correlation between the PR and FFP- types (ANOVA, p = 0.562) (Figure 3) (Table 4).
Figure 3: Boxplot to demonstrate the correlation of PR and FFP-types.
Table 4: PR and FFP-types.
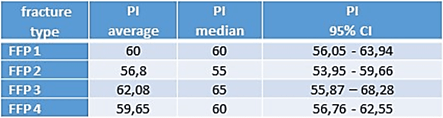
IV Classification of the Pelvic Morphology into Circle-Type and Ellipse-Type Depending on PR (DT/DS Ratio)
A total of 57 patients (40.43%) showed a DT/DS ratio ≤ 1.06, corresponding to a circle-type pelvis. In 24 patients (17.02%), the DT/DS ratio was ≥ 1.18, which corresponds to an ellipse-type pelvis. There is a strong statistical correlation between the pelvic morphology and fragility fractures of the pelvis. The circle-type pelvis is significantly more common in FFP-fractures than an ellipse-type pelvis (t-test unequal variances: p <0.001) (Table 5).
Table 5: Circle-type and ellipse-type morphology of the true pelvis in the overall collective.
Discussion
Fragility fractures of the pelvis are associated with reduced quality of life, functional impairment, restricted mobility and increased mortality. Osteoporosis is one of the major causes and women older than 65 years are mostly affected [1, 9]. 60% of the fragility fractures of the pelvis are related to osteoporosis [2, 3]. There is little information about the influence of anatomical conditions such as pelvic incidence and pelvic morphology (pelvic ratio) on fragility fractures of the pelvis. A further understanding is desirable for the future as increased aging of the population and an increased fracture incidence have been proven [10]. In this study, the average age was 84.87 years (men 81.5 years, women 85 years). The female sex predominates with 90.07%. These data do not differ significantly from the previously largest published population by Rommens et al. The reported average age of the 245 patients was 79.2 years and female patients were affected in 80.8% (data from the years 2007-2012, progressive aging of the population) [6]. In our collective, FFP type 2 fractures (41%) occurred most frequently, followed by type 4 (32%) and type 1 fractures (19%). FFP type III fractures (8.5%) were the least represented. This distribution is just about similar to the reported data in the literature [6]. According to the literature, the results of our work demonstrate that female patients are more often affected than male patients (90.07% women vs. 9.93% men). There was no significant difference in age between men and women (p = 0.14). Regarding the literature, the predisposition of the female sex is due to the higher incidence of osteoporosis in this population [2, 9, 11-13].
I Influence of Osteoporosis
Remodeling processes in osteoporotic pelvic bones can lead to failure and fracture, even in the case of physiological load sharing forces. This is impressive in the sacrum, where reduction of cancellous and cortical bone and the fatty conversion lead to “alar void”. Progressive fracture dissociation leads to load share transmission in non-fractured regions (pubic ramus, symphysis) with subsequent fractures [14-16]. This might also explain the influence of osteoporosis on the progression of fragility fractures of the pelvis. [2, 3, 11, 12].
II Influence of the Pelvic Anatomy
To the best of our knowledge, there is little evidence in the current literature that anatomical and positional spinopelvic parameters influence the development of fragility fractures of the pelvis. The changes of the global alignment in the elderly are well known: decrease of lumbal lordosis (LL), increase of thoracic kyphosis (TK), increase of sagittal vertical axis (SVA). The relation of osteoporotic-related sagittal imbalance and the resulting spinopelvic compensation has been demonstrated [17]. Compensatory mechanisms and adaptations of the positional spinopelvic parameters are required to keep the balance in a comfort position: increase of pelvic tilt (PT), decrease of sacral slope (SS). This possibility of compensation depends on anatomical conditions: the higher the SS (correspondingly PI), the higher the PT [18-20]. Positional spinopelvic parameters, particularly the PT, might influence the development of sacral insufficiency fractures. An increased pelvic retroversion to compensate for a sagittal imbalance leads to increased stress forces in the sacral plateau, the ala and in the S1/S2 interval. This can lead to insufficiency fractures in reduced bone quality [21]. Accordingly, the higher the PI, the higher the required PT for compensation and finally, the higher the fracture risk. To the authors’ opinion, little evidence-based literature is currently available in this regard. Finite element analyses could demonstrate a significant correlation between resulting stress forces at the lumbosacral junction and the PI: the higher the PI, the higher the stress forces at the lumbosacral junction. In conclusion, high-grade PI leads to increased stress forces and possibly increased fracture risk in reduced bone density [22-26].
The results of our work can not support these considerations. Patients with FFP type 1 fractures had a mean PI of 60º (± 10.46º). Patients with FFP type 2 fractures had a mean PI of 56.8º (± 11.26º). Patients with FFP type 3 fractures demonstrated a mean PI of 62.08º (± 10.96º). Patients with FFP type 4 fractures had a mean PI of 59.65º (± 9.78º). We could demonstrate no statistically significant correlation between the PI and fragility fractures of the pelvis (p = 0.81). In particular, there is no indication that a higher-grade instability (type 4 fracture) correlates with a higher-grade PI, vice versa. Lee et al. examined the influence of the morphology of the true pelvis on the development of FFP type 2 fractures. They determined the relation between the transverse and sagittal pelvic diameter of the true pelvis using 3D-MPR-CT and classified an ellipse-type and circle-type pelvis. The authors concluded that patients with a circle-type morphology have an increased fracture risk [7]. We evaluated the pelvic ratio (DT/DS ratio) in our collective. The mean DT/DS ratio was 1,099 (95% CI: 1.08-1.11). 57 patients (40.43%) revealed a circle-type pelvis and 24 patients (17.02%) an ellipse-type pelvis. There is a strong statistical correlation between the pelvic morphology and fragility fractures of the pelvis. The circle-type pelvis is significantly more common in FFP than an ellipse-type pelvis (p <0.001).
Thus we can confirm that the circle-type is associated with a higher risk of a fragility fracture of the pelvis. Lee et al. evaluated a mean DT/DS ratio of 1.13 (± 0.09) in FFP type 2 fractures. They found a circle-type morphology in 43.4% and an ellipse-type mophology in 10.5%. In our collective, patients with FFP type 2 fractures had a mean PR of 1.10 (± 0.04), a circle-type was present in 36.21% and an ellipse-type in 22.41% of the FFP type 2 fractures. These deviations can be based on ethnic differences [27, 28]. In conclusion, the results of our work could demonstrate a correlation between the circle-type shape of the pelvis and fragility fractures of the pelvis. There was no correlation between pelvic incidence and fragility fractures of the pelvis.
Limitation
This is a retrospective study. We analysed patients who required inpatient treatment of a fragility fracture of the pelvis. We could demonstrate no statistical correlation between pelvic incidence and FFP. The influence of the positional spinopelvic parameters (PT, LL, SS) could not be analysed, due to missing long spine and standing lumbar X-ray images. Further examinations will be helpful to analyse the influence of the positional spinopelvic parameters on fragility fractures of the pelvis.
Conclusion
The results of our work demonstrate a correlation between the morphology of the true pelvis and fragility fractures of the pelvis: the circle-type shape is more often associated with fractures than the ellipse-type. There was no correlation between pelvic incidence and fragility fractures of the pelvis. The influence of the positional spinopelvic parameters could not be assessed in this study. Further examinations with standing and long spine X-ray images are required.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Tue 22, Jun 2021Accepted: Wed 07, Jul 2021
Published: Mon 30, Aug 2021
Copyright
© 2023 Matthias Spalteholz. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.GGR.2021.01.01
Author Info
Matthias Spalteholz Gulow Jens Pap Geza
Corresponding Author
Matthias SpalteholzDepartment of Spine Surgery, Helios Park-Klinikum Leipzig, Leipzig, Germany
Figures & Tables

References
1.
Andrich S, Haastert B,
Neuhaus E, Neidert K, Arend W et al. (2017) Excess Mortality After Pelvic
Fractures Among Older People. J Bone Miner Res 32: 1789-1801. [Crossref]
2.
Rollmann MF, Herath
SC, Kirchhoff F, Braun BJ, Holstein JH et al. (2017) Pelvic ring fractures in
the elderly now and then - a pelvic registry study. Arch Gerontol Geriatr
71: 83-88. [Crossref]
3.
Maier GS, Kolbow K,
Lazovic D, Horas K, Roth KE et al. (2016) Risk factors for pelvic insufficiency
fractures and outcome after conservative therapyRisk factors for pelvic
insufficiency fractures and outcome after conservative therapy. Arch
Gerontol Geriatr 67: 80-85. [Crossref]
4.
Rommens PM, Drees P,
Thomczyk S, et al. (2018) The fragility fracture of the pelvis is a fracture
indicating osteoporosis. Osteologie 144-153.
5.
Rommens PM, Arand C,
Hopf JC, Mehling I, Dietz SO et al. (2019) Progress of instability in fragility fractures of the pelvis: An
observational study. Injury 50: 1966-1973. [Crossref]
6.
Rommens PM, Hofmann A
(2013) Comprehensive classification of fragility fractures of the pelvic ring:
Recommendations for surgical treatment. Injury 44: 1733-1744. [Crossref]
7.
Lee HH, Kim WY, Lim
YW, Byun YS, Lee SW (2021) Is there a correlation between fragility fractures
of the pelvis (FFP) and the morphology of the true pelvis in geriatric
patients? Eur J Trauma Emerg Surg 47: 3-10. [Crossref]
8.
Vrtovec T, Janssen
MMA, Likar B, Castelein RM, Viergever MA et al. (2012) A review of methods for
evaluating the quantitative parameters of sagittal pelvic alignment. Spine J
12: 433-446. [Crossref]
9.
Hadji P, Klein S,
Gothe H, Häussler B, Kless T et al. (2013) The epidemiology of
osteoporosis--Bone Evaluation Study (BEST): an analysis of routine health
insurance data. Dtsch Arztebl Int 110: 52-57. [Crossref]
10. Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C et al. (2013)
Osteoporosis in the European Union: medical management, epidemiology and
economic burden. A report prepared in collaboration with the International
Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical
Industry Associations (EFPIA). Arch Osteoporos 8: 136. [Crossref]
11. Burge R, Dawson Hughes B, Solomon DH, Wong JB, King A et al. (2007)
Incidence and economic burden of osteoporosis-related fractures in the United
States, 2005-2025. J Bone Miner Res 22: 465-475. [Crossref]
12.
Morris RO, Sonibare A,
Green DJ, Masud T (2000) Closed pelvic fractures: characteristics and outcomes
in older patients admitted to medical and geriatric wards. Postgraduate Med
J 76: 646-650. [Crossref]
13. Balogh Z, King KL, Mackay P, McDougall D, Mackenzie S et al. (2007) The
epidemiology of pelvic ring fractures: a population-based study. J Trauma
63: 1066-1073. [Crossref]
14. Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H et al. (2016) Sacral
Bone Mass Distribution Assessed by Averaged Three-Dimensional CT Models:
Implications for Pathogenesis and Treatment of Fragility Fractures of the
Sacrum. J Bone Joint Surg Am 98: 584-590. [Crossref]
15. Josten C, Höch A (2017) Fractures of the sacrum: operative/conservative
Pro: Why insufficiency fractures of the sacrum should be treated operatively. Die
Wirbelsäule 1: 31-40.
16. Kurz S, Fischer B, Böhme J (2017) Biomechanik des Beckens. Orthopäd
Unfallchirur up2date 12: 27-44.
17. Fechtenbaum J, Etcheto A, Kolta S, Feydy A, Roux C et al. (2016) Sagittal
balance of the spine in patients with osteoporotic vertebral fractures. Osteoporos
Int 27: 559-567. [Crossref]
18. Labelle H, Roussouly P, Chopin D, Berthonnaud E, Hresko T et al. (2008)
Spino-pelvic alignment after surgical correction for developmental
spondylolisthesis. Eur Spine J 17: 1170-1176. [Crossref]
19. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of
the normal variation in the sagittal alignment of the human lumbar spine and
pelvis in the standing position. Spine (Phila Pa 1976) 30: 346-353. [Crossref]
20. Vialle R, Levassor N, Rillardon L, Templier A, Skalli W et al. (2005)
Radiographic analysis of the sagittal alignment and balance of the spine in
asymptomatic subjects. J Bone Joint Surg Am 87: 260-267. [Crossref]
21. Sato T, Shiota N, Sawaguchi T (2017) Non-Operative Treatment. Fragil
Fract Pelvis 88-95.
22. Sevrain A, Aubin CE, Gharbi H, Wang
X, Labelle H (2012) Biomechanical evaluation of predictive parameters of
progression in adolescent isthmic spondylolisthesis: a computer modeling and
simulation study. Scoliosis 7: 2. [Crossref]
23. Hanson DS, Bridwell KH, Rhee JM, Lenke LG (2002) Correlation of pelvic
incidence with low- and high-grade isthmic spondylolisthesis. Spine (Phila
Pa 1976) 27: 2026-2029. [Crossref]
24. Labelle H, Roussouly P, Berthonnaud E, Transfeldt E, O'Brien M et al.
(2004) Spondylolisthesis, pelvic incidence, and spinopelvic balance: a
correlation study. Spine (Phila Pa 1976) 29: 2049-2054. [Crossref]
25. Tebet MA (2014) Current concepts on the sagittal balance and classification
of spondylolysis and spondylolisthesis. Rev Bras Ortop 49: 3-12. [Crossref]
26. Zhao J, Xiao Y, Zhai X, Chen Z, Li
M (2018) Difference of Sagittal Alignment between Adolescents with
Symptomatic Lumbar Isthmic Spondylolisthesis and the General Population. Sci Rep 8: 10956. [Crossref]
27. Fei H, Li WS, Sun ZR, Ma QW, Chen ZQ (2017) Analysis of Spino-pelvic Sagittal Alignment in Young Chinese Patients with Lumbar Disc Herniation. Orthop Surg 9: 271-276. [Crossref]
28. Zhu Z, Xu L, Zhu F, Jiang L, Wang Z et al. (2014) Sagittal alignment of spine and pelvis in asymptomatic adults: norms in Chinese populations. Spine (Phila Pa 1976) 39: E1-E6. [Crossref]
