Teaching Review on Approach of Esophageal Intubation as Complications in Emergency Airway Management
A B S T R A C T
Background: Intubation is daily process in hospitals, it’s insertion of tube to secure an airway, non-emergent intubation is done in well controlled circumstances, while emergent intubation is not. Most emergency intubated are cardiac or respiratory arrest patients. Intubation helps to secure airway for patient breathing, also could protect from aspiration. Most common complications are: esophagus intubation and hypotension. This research will be divided into two main topics, emergency intubation as a whole, and unrecognized esophagus intubation as a complication. Emergency intubation discuss: knowledge about the procedure, equipment needed, airway assessment, preoxygenation, difficulties and risks, outcomes. While Unrecognized esophagus intubation will be discussed as complication in ER settings, point to clear: Epidemiology, tools of detection, equipment, human and environmental bias and consideration for cardiac arrest patients. Finishing with a conclusion and recommendation. Therefore, we aim to look into the common pitfalls that both medical students and new physicians face in the recognition, diagnosis, and Emergency Airway Management.
Targeted Population: Airway cardiorespiratory arrest patients who are requiring urgent management in the ED, with emergency physicians for teaching approach protocol.
Aim of the Study: Appropriate for assessment and priorities for Airway cardiorespiratory arrest patients by training protocol to emergency physicians. Based on patients’ causes of Airway injuries.
Methods: Collection of all possible available data about the Esophageal Intubation as Complications in the Emergency department. By many research questions to achieve these aims so a midline literature search was performed with the keywords “critical care”, “emergency medicine”, “principals of airway management”, “Esophageal Intubation as Complications”. Literature search included an overview of recent definition, causes and recent therapeutic strategies.
Results: All studies introduced that the initial diagnosis of Esophageal Intubation as Complications is a lifesaving conditions that face patients of the emergency and critical care departments.
Conclusion: Intubation in emergency settings require a good preparation, available equipment (e.g. ready cart for all time), and supportive anatomical airway of the patient. Following a checklist will improve outcomes, prevent malpractice and complications. Preoxygenation and RSI play major roles for successful intubations with decrease risk of complications. Follow procedure steps, and expect difficult intubation for any patient, so consider LEMON mnemonic to evaluate risk of difficulty, and after 3 attempts try a different technique or equipment. More training and education are essential to decrease congenital and equipotential mistakes/errors.
Keywords
Airway, emergency physicians, skill approach, management
Introduction
Intubations in the hospital is a daily process aimed to secure an airway, which further makes a route for oxygen and ventilation delivery, also protect from aspiration. Our topic is going to discuss the emergent intubation, which is different than the nonemergent, which done under controlled circumstances [1]. Emergent intubation usually involves a patient suffers cardiac or respiratory arrest, and it’s done under resuscitation activities. Endotracheal intubation plays the cornerstone role of emergent airway management. Intubation maybe accomplished by the emergency physician, anaesthesiologist, pulmonologist, respiratory therapist or even a nurse practitioner. Before intubation many preparations are taken to improve the outcomes, like rapid sequence intubation, preoxygenation, equipment checking and positioning the patient. Mallampati criteria and LEMON mnemonic give idea about difficulty of intubation [2].
During emergency intubation, some complications may surface, and most common two are esophagus intubation and hypotension, while esophagus intubation results from mispositioning, hypotension usually is result of RSI induction [3]. Unrecognized esophagus intubation of ETT has incidence between 3-17%, it is the most common complication of emergency intubation, and it’s a found cause of morbidity and mortality in emergency rooms, specially brain damage and death. Because of danger effects esophagus intubation may cause, some checklists and tools are used to check positioning as ETCO2. However, arrest patients need better alternative and Acoustic reflectometry shows a promising one [3].
To Do Before Intubation
Figure 1: Tools Pre-intubations.
The preparation is very important for a successful intubation, and for that there is a list of equipment practitioner should prepare before the procedure (Figure 1). This equipment preferably be ready in the special cart, along with other considerations, like a small sized laryngoscope in case of pediatric case, next step would be ensuring ongoing cardiac rhythm, heart rate, blood pressure, O2 saturation and carbon dioxide partial pressure. During the preparation patient is ventilated and oxygenated with bag-mask ventilation (BMV, Figure 2).
Figure 2: The Bag Mask Ventilation.
Figure 3: Positioning During Intubation.
Figure 4: Intubation Operator isn’t correct on the left; Intubation Operator is correct on the right.
Next, IV access establishment and appropriate fluids: Next, patient positioning, a trained staff is called to adjust patient position, patient need to be supine, with head hyperextended in a ‘sniffing’ position, his external ear is aligned with the sternal notch (Figure 3) this shall help for better glottis visualization. The bed should be elevated till the operator’s xiphoid; this will give a better access to the mouth above patient head during intubation (Figure 4). It’s not optimal for intubation to apply padding under neck or shoulder [1].
Figure 5: Yankauer Catheter.
Sometimes a more upright intubation position might be used when patient can’t lay supine, as a patient with severe pulmonary edema or is morbidly obese (Figure 7). If patient is vomiting or with large stuck particles, use Yankauer catheter (Figure 5) or other suction tube in the side of the mouth, suction will be made along with intubation (Figure 6).
Figure 6: Suction with Intubation.
Figure 7: Intubations in morbid obese with pulmonary edema.
After you finish preparing your equipment, make sure of its functionality, including oxygen mask, suction tube, laryngoscope lighting and blade and so on. Check the availability of a mechanical ventilator for applying after intubation has been made, do not forget to calculate the body mass and appropriate doses of the adjuvant intubation medications, rapid sequence induction (RSI) and types of laryngoscopes will be covered later on in this research [4]. Collect all possible clinical information, patient condition, his history and define your care goals and discus it with your team. A checklist could be used for easy application and for prevention of any kind of errors (Figure 8). Patient parameters are important to normalize before intubating drugs induction, it includes heart rate, oxygen saturation and blood pressure, the reason that cardiac arrests are possible when any parameter of these are abnormal [2].
Airway Assessment
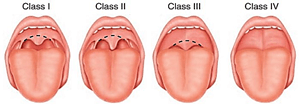
About 15% of initial emergent intubation attempts fail in recent study, and 2% of overall endotracheal attempts also fail with the standard method, “Expect difficulty with all emergency airway cases, apply a uniform approach to all patients” Tintinalli said in his 9th edition [1]. Some factors defined for airway management and intubation difficulty, which are: facial hair, lack teeth, history of OSAS, short neck, limited neck mobility, small or large chin, prominent incisors, high arched palate, facial or airway trauma, head or neck tumors, angioedema, Ludwig’s angina and finally inflammation of the airway as in burning patients. Mallampati criteria suggests the difficulty of intubation according to tongue level (Figure 9) [1].
Figure 9: Mallampati criteria for Assessment Airway.
Preoxygenation
Process of giving O2 before the intubation, aim of it to improve oxygen saturation, further decreases risks of dysrhythmias, decompensation and cardiac arrest, also helps to make more space for oxygen by removing nitrogen from alveoli. Preoxygenation is induced with tidal breathing and with sealing the mask. If oxygen saturation fails to reach above 90% with spontaneous breathing, bag-valve-mask, continuous positive airway pressure or other solutions should be considered. Sometimes, head elevation could be useful, as sedatives for agitated patients [4].
Procedure (Back to Figure 8 for more details)
i. Clear the mouth, remove any unsecured particles (e.g. fallen tooth, food).
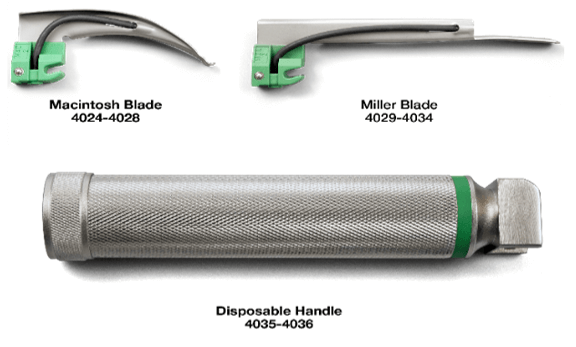
ii. Carry the laryngoscope (Figure 10) from its base with left hand.
iii. With your right hand, open the mouth, insert suction tube, manipulate the larynx, insert ETT (Endo tracheal tube).
iv. Insert the blade into the right side of the mouth, and carefully advance through it.
v. After reaching epiglottis and visualize glottis (Figure 11), lift it to provide access for ETT.
vi. CARE for vocal cords injury by excessive insertion.
vii. Put the ETT with caution.
viii. Inflate the balloon, use from 5-7 mL of air.
ix. Confirm correct placing, by stethoscope, bilateral breath sounds, no epigastric sounds. Also, by colorimetric carbon dioxide detector (Figure 12), usually accompany ETT. Later, radiograph (end tube has a ‘shiny’ part) (Figure 13) and echo shall be made to confirm the positioning.
x. Secure ETT, use taping or tube holder [1].
Figure 10: laryngoscope.
Figure 11: Uvula for Assessment Airway.
Figure 12: Colorimetric Carbon Dioxide Detector.
Figure 13: Endotracheal Tube on X-ray to confirm position by “a shiny part”.
Difficulties of Emergency Intubation
Researchers usually use the number of attempts to evaluate intubation success. Some indications for difficult intubation prior the procedure forms a mnemonic: LEMON, it’s been tested in adult cases only not children.
L: Look for indications for difficult intubation, facial hair, burns… etc.
E: Evaluate mouth opening, thyromental and mandible to thyroid cartilage distances with head fully extended.
M: Mallampati score (Figure 9).
O: Obstruction of upper airway tract signs, stridor, wheezing and muffled voice.
N: Neck immobility, cervical injury and congenital abnormalities.
However, many studies conducted to measure success rate of intubation, two examples were studies that made on 10 years. First between 1990 and 2000, the other between 2002 and 2012, it found 68% success rate in first attempt, while 83% in the other one, putting into consideration, the larger sample size of second study (19,629), compared to smaller (2,833) sample size in the first one [1, 4, 5]
Complications of Emergency Intubation
Preparation could prevent many complications that may arise, but few issues to be expected or associated with three or more attempts, such as, hypoxemia, regurgitation and aspiration, tract trauma, bradycardia and esophageal intubation. Other possible complications, like: teeth trauma, right bronchus intubation, damage to vocal cords and infections.
Figure 14: A) laryngeal mask airway; B) Multiple Lumen Esophageal Airway (Combitube).
That is why the American Society of Anaesthesiologists, advices to limit attempts of 3 times, if procedures kept failing to switch to other alternatives and use of special aids, laryngeal mask airway (Figure 14A). Or esophageal tracheal double lumen airway (Figure 14B). Along through, most frequent complication for intubation was esophagus intubation, comes hypotension in next (other complications with prevention and correction strategies) (Figure 15) [4, 5].
Figure 15: Complications of Endotracheal Intubation with Correct Actions.
In 1980, 11% of brain death cases raise a claim of esophagus intubation, number deceased to 3% in 1990 after invention of end-tidal CO2 monitoring (ETCO2, Figure 16). This doesn’t mean misplacement wasn’t occurring anymore, more clearly, it was corrected due the detection by CO2 monitor. In some study, auscultation, ETCO2, self-inflating bulb and transillumination using torchlight were all used to determine which one is more reliable in ETT insertion, ETCO2 was best for verification the proper placement, but poorer outcomes showed with people of cardiac arrests.
Figure 16: End-tidal CO2 Monitoring.
Figure 17: Fiberoptic Evaluation technique.
Figure 18: Acoustic Reflectometry.
So, what could make an excellent choice for cardiac arrest patients? X-rays are of limited value, because delay of diagnosis. Fiberoptic evaluation (Figure 17) needs special equipment and preparation, hence, time consuming. Acoustic reflectometry (Figure 18) shows promising results with experienced hands, Raphael and colleagues made a study on 200 adults intubated with acoustic reflectometry, having a 99% correct endotracheal intubation, 100% esophageal intubation detection [6-8].
The ETT displacement is common among inexperienced anaesthetics, but being unrecognized is actually rare, most of these cases arise due neglecting use of confirmation procedures and could be easily fixed if noticed. Confirmation procedures as vocal cords visualization while installing the tube, CO2 detectors, equal chest expansion, auscultation, ultrasound and radiographs could all prevent the displacement. Unfortunately, problem may appear after following some clinical procedures because lack of experience, thus it needs more training to reach practicality. Sometimes, issue connected to cognitional factors, top 3 that were identified are: fixation error, confirmation bias and overconfidence.
For example, fast air flowing to stomach may mistake the practitioner that tube is inserted correctly, mechanical ventilator tidal volume if high might be mistaken as breath sound as leakage of NG tube prevents abdomen distention. In some settings, lack of proper equipment as ETCO2 monitors caused delayed detection, further death [9-11].
Conclusion and Recommendations
Intubation is a daily procedure, and emergency intubation usually involves patients with cardiac or pulmonary arrests, and as esophagus intubation is most common complication but with less reliability to arrest patients using ETCO2, alternative gold standard method should be defined. Intubation in emergency settings require a good preparation, available equipment (e.g. ready cart for all time), and supportive anatomical airway of the patient.
Following a checklist will improve outcomes, prevent malpractice and complications. Preoxygenation and RSI play major roles for successful intubations with decreased complications. Follow procedure steps, and expect difficult intubation for any patient, so consider LEMON mnemonic to evaluate risk of difficulty, and after 3 attempts try a different technique or equipment. More training and education are essential to decrease congenital and equipotential mistakes/errors. Workplace should be supportive with adequate materials and space.
Article Info
Article Type
Review ArticlePublication history
Received: Wed 26, Aug 2020Accepted: Fri 25, Sep 2020
Published: Thu 29, Oct 2020
Copyright
© 2023 Adel Hamed Elbaih. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2020.03.13
Author Info
Adel Hamed Elbaih Mohammad Assef Mousa
Corresponding Author
Adel Hamed ElbaihAssociate Professor of Emergency Medicine, Faculty of Medicine, Suez Canal University, Ismailia, Egypt
Figures & Tables

















References
- TINTINALLI'S Emergency Medicine 9th edition.
- Hart D, Clinton J, Anders S, Reihsen T, McNeil MA et al. (2016) Validation of an Assessment Tool for Field Endotracheal Intubation. Mil Med 181: e1484-e1490. [Crossref]
- Elbaih AH, Taha M, Elsakaya MS, Elshemally AA, Alshorbagy ME (2019) Assessment of cardiopulmonary resuscitation knowledge and experiences between emergency department nurses hospital pre and post basic life support training course, Egypt. Ann Med Res 26: 2320-2327.
- Pruitt B (2019) Emergency intubations are almost always associated with cardiac or respiratory arrest in hospitalized patients and often occur during intense resuscitation activities.
- Elbaih AH, Elsayed ZM, Ahmed RM, Abd Elwahed SA (2019) Sepsis patient evaluation emergency department (SPEED) score & mortality in emergency department sepsis (MEDS) score in predicting 28-day mortality of emergency sepsis patients. Chin J Traumatol 22: 316-322. [Crossref]
- Kumar N, Kumar A, Dubey PK, Kumar S (2018) Delayed detection of esophageal intubation: Nasogastric tube was the cause? Saudi Crit Care J 2: 27-28.
- Krafft P, Frass M (2007) Airway Management in Intensive Care Medicine. Benumof's Airway Management 1016-1054.
- Elbaih AH, Basyouni FH (2020) Teaching Approach of Primary Survey in Trauma Patients. SunText Rev Surg 1: 1-7.
- Mansfield JP, Wodicka GR (1995) Using Acoustic Reflectometry To Determine Breathing Tube Position And Patency. J Sound Vibration 188: 167-188.
- Boqué MC, Gualis B, Sandiumenge A, Rello J (2004) Endotracheal tube intraluminal diameter narrowing after mechanical ventilation: use of acoustic reflectometry. Intensive Care Med 30: 2204-2209. [Crossref]
- Elbaih AH, El Sayed DA, Abou Zeid AE, Elhadary GK (2018) Patterns of brain injuries associated with maxillofacial fractures and its fate in emergency Egyptian polytrauma patients. Chin J Traumatol 21: 287-292. [Crossref]
