Takotsubo Cardiomyopathy: An Unusual Case Report in a Patient Affected with Alzheimer’s Disease
A B S T R A C T
We describe a case report regarding an elderly woman affected with Alzheimer’s disease (AD), presenting to the ER for chest pain, and showing ST-segment elevation on electrocardiography, and elevated cardiac enzyme levels. She was hospitalized and after a number of laboratory and instrumental exams she was diagnosed Tako-tsubo syndrome. One year after the event she is feeling fine, electrocardiogram is normal, and no symptoms of cardiac heart failure are present. Tako-tsubo syndrome is a stress-induced cardiomyopathy that involves left ventricular apical akinesis and mimics acute coronary syndrome. It was first described in Japan in 1991, it is rare (1:36.000) with 1:3 male/female ratio and survival is usually 96%. The novelty of this case-report is due to its rarity and to the onset of the disease in an elderly patient affected with AD.
Keywords
Tako-Tsubo syndrome, dementia, heart failure, cardiomyopathy
Background
Tako-tsubo syndrome is a stress-induced cardiomiopathy that involves left ventricular apical akinesis and mimics acute coronary syndrome. It was described in Japan in 1991. The main symptoms are chest pain, ST-segment elevation on electrocardiography (ECG), and elevated cardiac enzyme levels [1].
Case Report
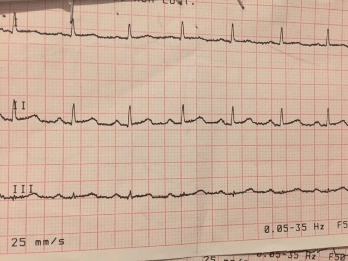
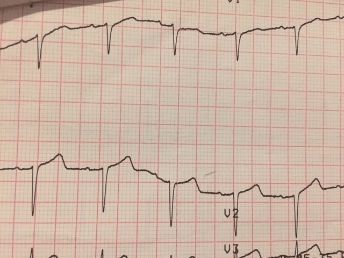
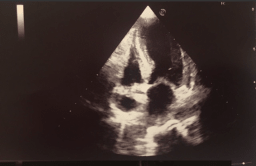
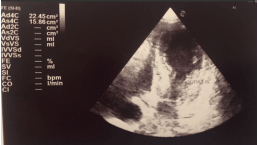
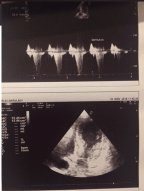
An 85-year-old woman was affected with Alzheimer’s disease (AD), hypertension, depression with behavioral disorders and diabetes. She was on treatment with valsartan 160/12.5 mg, donepezil 10 mg/day, aspirin 100 mg, metformin 500 mg after meals, promazine 20 mg as needed. Patient suddenly started to have recurrent syncope and hypotension. She was brought to the ER, where she was found to have high levels of pro-BNP (pro-Brain Natriuretic Peptide)(10936 pg/ml) (Table 1). ECG showed anteroseptal myocardial infarction (Figure 1), with mild elevation of cardiac enzymes (Table 1). Brain CT scan showed widespread hypodensity in the periventricular white matter and at the basal ganglia bilaterally, together with parenchymal atrophy. She was hospitalized at the Intensive Care Unit (ICU) and underwent cardiac angiography. Left ventricular apical ballooning was present, but there was no significant coronary artery stenosis. Clinical course was without complications. Color Doppler cardiac ultrasound showed increased parietal thicknesses of the left ventricle, which caused dynamic obstruction and mild hypokinesia of the apex (Figure 2). Doppler ultrasound showed increased aortic trans-valvular flow rate with Pmax 37 mmHg, inversion of the E/A ratio (for altered left ventricular compliance). In the view of the above reported results, Tako-Tsubo syndrome was diagnosed. She was discharged 8 days after hospitalization. Table 2 reports the medical treatment.
Six months after ECG was normal and Doppler cardiac ultrasound showed the progressive normalization of regional kinesis and of the global left ventricular function. She is feeling fine and she had further memory loss with behavioral disorders (she has been taking memantine 20 mg/day).
Table 1: The table 1 reports the labs soon after the admission to the ER. In red the exams out of the normal range. WBC = White Blood Cells; RBC = Red Blood Cells; MCV = Mean corpuscular Volume; MCH = Mean Corpuscular Hemoglobin; MCHC = Mean Corpuscular Hemoglobin Concentration; RDW = Red cells Distribution Width; MPV = Mean Platelet Volume; Luc = Large uncountable cells; INR = International Normalized Ratio; AST = Aspartate Transaminase; CK = Creatine Kinase; LDH = Lactate Dehydrogenase.
|
WBC |
8 x 103 /mm3 |
|
RBC |
4.6 x 103 /mm3 |
|
Hemoglobin |
12.8 g/dl |
|
Hematocrit |
40.1% |
|
MCV |
87.1 fl |
|
MCH |
27.8 g/dl |
|
MCHC |
31.9 % |
|
RDW |
15.4% |
|
Platelets |
358 x 103 /mm3 |
|
MPV |
7.1 fl |
|
Plateletcrite |
0.25% |
|
Neutrophils |
5.9 x 103 /mm3 – 74.9% |
|
Lymphocytes |
1.4 x 103 /mm3 – 17.2% |
|
Monocytes |
0.5 x 103 /mm3 – 6.5% |
|
Eosinophils |
0.0 – 0.5% |
|
Basophils |
0.0 – 0.4% |
|
Luc |
1.3% |
|
INR |
1.01 |
|
D-Dimer |
0.78 mg/l |
|
Glycemia |
103 mg/dl |
|
Azotemia |
42 mg/dl |
|
Creatinine |
0.6 mg/dl |
|
AST |
17 U/L |
|
CK |
87 U/L |
|
CK-MB |
11 U/L |
|
LDH |
172 U/L |
|
Sodium |
142 mEq/L |
|
Potassium |
4.1 mEq/L |
|
Calcium |
9.8 mg/dl |
|
Plasma Osmolarity |
305 mOsm/L |
|
CPK-MB mass |
6.25 ng/ml |
|
Troponin T |
0.207 ng/ml |
|
Myoglobin |
23 ng/ml |
|
Pro-BNP |
10.936 pg/ml |
Figure 1: ECG shows mild ST-segment elevation. It was present in V1-V3.
Figure 2: Doppler cardiac ultrasound shows increased aortic trans-valvular flow rate with Pmax 37 mmHg, inversion of the E/A ratio
Table 2: The table reports the suggested treatment on discharge
|
Pantoprazole 20 mg fasting |
Furosemide 25 mg at 9 am |
|
Bisoprolol 1.25 mg after breakfast |
Duloxetine 30 mg after breakfast |
|
Aspirin 100 mg after lunch |
Metformin 500 mg after lunch |
Conclusions
Takotsubo is a rare disease (1:36.000) with 1:3 male/female ratio, more frequent in postmenopausal women; indeed, it is more frequent between the 7th and 8th decade of life and it is even rarer to find it in an over-80-year-old patient with AD [1, 2].
It occurs worldwide and is responsible for about 2% of all cases of acute coronary syndrome presenting to hospitals [2]. The name "takotsubo syndrome" comes from the Japanese word takotsubo, that is "octopus trap", because the left ventricle of the heart in patients affected resembles an octopus trap [2]. Tako-Tsubo is a stress cardiomyopathy, a non-ischemic cardiomyopathy characterized by a sudden temporary weakening of the muscular portion of the heart [3, 4]. Maybe it is caused by endothelial damage of the subepicardial vessels. The fall in estrogens, the dysfunction of catecholamine-mediated microcirculation, due to emotional stress, could trigger the syndrome. Myocardial dysfunction at the apex of the left ventricle could be due to the higher presence of adrenergic receptors in this area. A central role is thought to be played by a sudden massive surge of catecholamines such as adrenaline and norepinephrine [5]. This event can occur following an extreme stress and may lead to spasm of the coronary arteries, thus dramatically decreasing the delivery of an adequate blood flow and oxygen to the cardiac muscle [5]. This in turn may potentially be the cause of congestive heart failure and decreases the heart’s output of blood. Indeed, in our patient pro-BNP was extremely high.
However, survival is usually 96%; other possible complications are cardiac arrest, heart failure, potentially lethal ventricular arrhythmias and myocardial rupture.
It is treated with β-blockers, diuretics, ACE-inhibitors, aspirin. Recovery is usually spontaneous and occurs within a few weeks. The novelty of this case-report is due to its rarity and to the onset of the disease in an elderly patient affected with AD.
Article Info
Article Type
Case ReportPublication history
Received: Sun 08, Sep 2019Accepted: Mon 23, Sep 2019
Published: Mon 30, Sep 2019
Copyright
© 2023 Pietro Gareri. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.NNB.2019.03.02
Author Info
Pietro Gareri Valeria Graziella Laura Manfredi
Corresponding Author
Pietro GareriCenter for Cognitive Disorders and Dementia, Catanzaro Lido, ASP Catanzaro
Figures & Tables
Table 1: The table 1 reports the labs soon after the admission to the ER. In red the exams out of the normal range. WBC = White Blood Cells; RBC = Red Blood Cells; MCV = Mean corpuscular Volume; MCH = Mean Corpuscular Hemoglobin; MCHC = Mean Corpuscular Hemoglobin Concentration; RDW = Red cells Distribution Width; MPV = Mean Platelet Volume; Luc = Large uncountable cells; INR = International Normalized Ratio; AST = Aspartate Transaminase; CK = Creatine Kinase; LDH = Lactate Dehydrogenase.
|
WBC |
8 x 103 /mm3 |
|
RBC |
4.6 x 103 /mm3 |
|
Hemoglobin |
12.8 g/dl |
|
Hematocrit |
40.1% |
|
MCV |
87.1 fl |
|
MCH |
27.8 g/dl |
|
MCHC |
31.9 % |
|
RDW |
15.4% |
|
Platelets |
358 x 103 /mm3 |
|
MPV |
7.1 fl |
|
Plateletcrite |
0.25% |
|
Neutrophils |
5.9 x 103 /mm3 – 74.9% |
|
Lymphocytes |
1.4 x 103 /mm3 – 17.2% |
|
Monocytes |
0.5 x 103 /mm3 – 6.5% |
|
Eosinophils |
0.0 – 0.5% |
|
Basophils |
0.0 – 0.4% |
|
Luc |
1.3% |
|
INR |
1.01 |
|
D-Dimer |
0.78 mg/l |
|
Glycemia |
103 mg/dl |
|
Azotemia |
42 mg/dl |
|
Creatinine |
0.6 mg/dl |
|
AST |
17 U/L |
|
CK |
87 U/L |
|
CK-MB |
11 U/L |
|
LDH |
172 U/L |
|
Sodium |
142 mEq/L |
|
Potassium |
4.1 mEq/L |
|
Calcium |
9.8 mg/dl |
|
Plasma Osmolarity |
305 mOsm/L |
|
CPK-MB mass |
6.25 ng/ml |
|
Troponin T |
0.207 ng/ml |
|
Myoglobin |
23 ng/ml |
|
Pro-BNP |
10.936 pg/ml |
Table 2: The table reports the suggested treatment on discharge
|
Pantoprazole 20 mg fasting |
Furosemide 25 mg at 9 am |
|
Bisoprolol 1.25 mg after breakfast |
Duloxetine 30 mg after breakfast |
|
Aspirin 100 mg after lunch |
Metformin 500 mg after lunch |
References
- Novo S, Akashi Y, Arbustini E et al. (2008) La cardiomiopatia takotsubo: documento di consenso. G Ital Cardiol 9: 785-97.
- Akashi YJ, Nef HM, Lyon AR (2015) Epidemiology and pathophysiology of Takotsubo syndrome. Nature Rev Cardiol 12: 387-397. [Crossref].
- Akashi YJ, Nef HM, Möllmann H, Ueyama T (2010) Stress cardiomyopathy. Ann Rev Med 61: 271-286.
- Zamir M (2005) The Physics of Coronary Blood Flow. Springer Science and Business Media 387.
- Tavazzi G, Zanierato M, Via G, Iotti GA, Procaccio F (2017) Are Neurogenic Stress Cardiomyopathy and Takotsubo Different Syndromes with Common Pathways? Etiopathological Insights on Dysfunctional Hearts. JACC Heart Failure 5: 940-942. [Crossref].
