Synovial Sarcoma Arising in the Retromolar Trigone: A Rare Presentation
A B S T R A C T
Synovial sarcoma is a rare malignant neoplasm of young adults with poor survival. These usually arise from large joints and articular tendons. We describe an unusual case of synovial sarcoma arising from the left retromolar trigone upon initial presentation. To the best of our knowledge, this case is the only patient with left retromolar trigone involvement recorded in the literature. A 33-year-old female presented to us with complaints of a lesion in the left retromolar trigone. An ulcerated lesion with irregular margins and a smooth base was noted at the left retromolar trigone. CT scan demonstrated a soft tissue mass predominantly involving the left buccal space measuring 5.0 × 4.2 × 2.8 cm superiorly extending into the left infratemporal region, closely abutting posterior lateral of the left maxillary sinus with gross bone thinning. Biopsy was taken from the temporal and infratemporal region, which was positive for synovial Sarcoma. She received 2 cycles of neoadjuvant chemotherapy AIM protocol followed by wide local excision, however, the margin status could not be ascertained. Subsequently, treatment with a total of 60 Gy adjuvant radiotherapy was given. Patient tolerated the treatment well and remained disease-free for 4.5 years. She then developed biopsy-proven recurrence at the primary site; her metastatic workup was negative. Unfortunately, the patient was lost to follow-up for 2 years and then presented with a very large lobulated mass in the left infratemporal fossa, now measuring 6.2 × 7.6 × 6.3 cm, encasing ramus of mandible, temporomandibular joint and muscle of mastication with intra-orbital extension. She received 2 cycles of chemotherapy with gemcitabine and docetaxel. However, she did not tolerate the chemotherapy well. Subsequently, she developed tumor bleeding and received palliative radiation for bleeding and pain control. Patient is now on the best supportive care, her general condition deteriorating rapidly with the passage of time. Synovial sarcoma of the retromolar trigone is a rare malignant tumor with a poor prognosis. As there is no standard treatment protocol for synovial sarcomas of the head and neck, optimal antineoplastic treatment remains unclear. Mainstay of treatment is surgical resection with high relapse rates. Radiation therapy, with or without chemotherapy, appears to improve survival.
Keywords
Sarcoma, synovial, retromolar trigone
Introduction
Synovial sarcoma is a rare malignant neoplasm of young adults with poor survival. These usually arise from large joints and articular tendons. Synovial sarcomas predominantly affect young adults. The most common sites are the extremities. Synovial Sarcomas rarely occur in head and neck cancers, generally accounting for only 3-5% of all head and neck cancers. The most common sites involved in the head and neck region are the hypopharynx, parapharyngeal space and post-pharyngeal region [1]. We describe an unusual case of synovial sarcoma arising from the left retromolar trigone upon initial presentation. To the best of our knowledge, this case is the only patient with left retromolar trigone involvement recorded in the literature.
Case Report
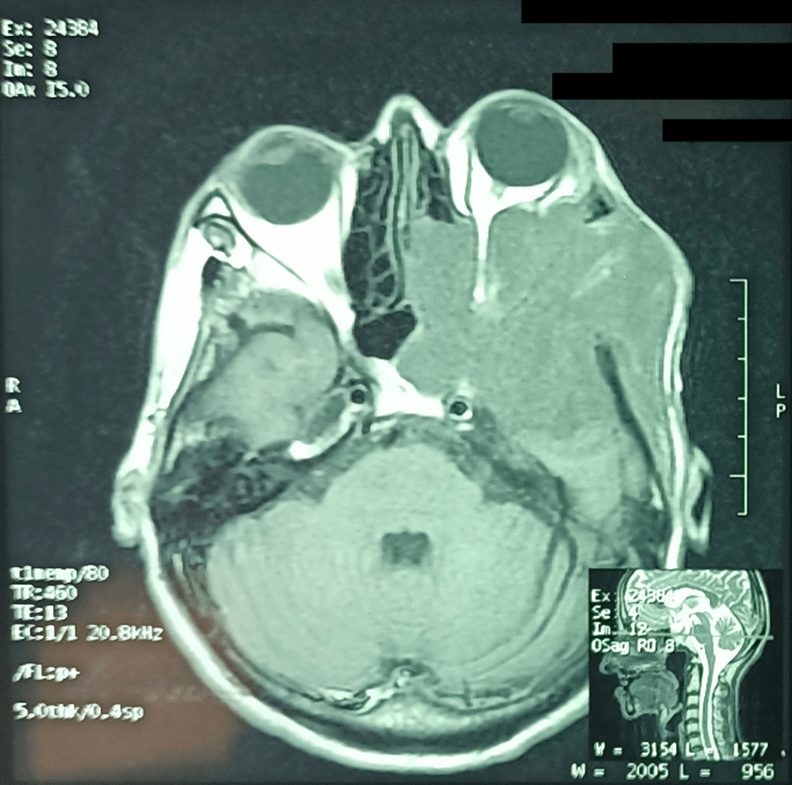
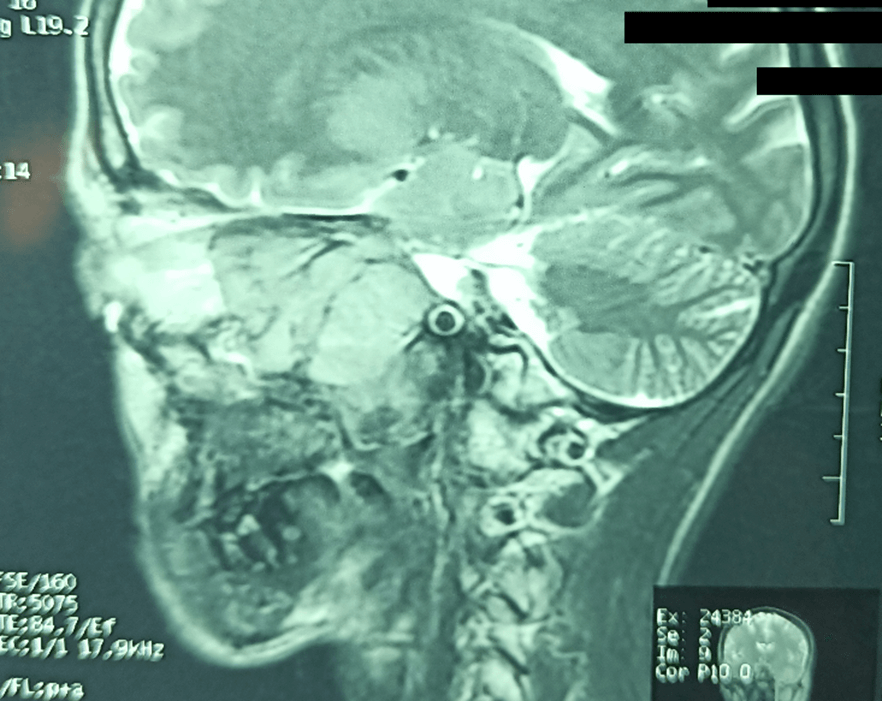
A 33-year-old female presented to us with initial complaints of a lesion in the left retromolar trigone alongside weight loss of approximately 20 kg for a year. The patient had no prior history of trauma or facial surgery. Upon physical examination, there was facial asymmetry and swelling of the left side of the cheek was noted. Her mouth opening was normal at the time. An ulcerated lesion with irregular margins and a smooth base was noted at the left retromolar trigone. The remainder of the oral cavity examination was unremarkable. The patient did not have lymphadenopathy at the time. The initial biopsy of the lesion revealed a fibro-epithelial polyp but no malignancy. However, the suspicion of malignancy was very high; therefore, imaging studies were performed. CT scan demonstrated a soft tissue mass predominantly involving the left buccal space measuring 5.0 × 4.2 × 2.8 cm superiorly extending into the left infratemporal region, closely abutting posterior lateral of the left maxillary sinus with gross bone thinning (Figures 1-3).
Figure 1: Computed tomography of head and neck with IV contrast. Axial section showing 5 × 4.2 × 2.8 cm mass of the left buccal space infiltrating the left orbit and left infratemporal fossa.
Figure 2: Computed tomography of head and neck with IV contrast. Axial section showing the mass extending into pterygopalatine fissure.
Figure 3: Computed tomography of head and neck with IV contrast, sagittal view.
Excision re-biopsy was taken from the temporal, infratemporal region and buccal mucosa. Histopathological analysis with H&E staining revealed a spindle cell tumor arranged in sheets. Individual tumor cells showed spindle to polygonal shape with pleomorphic vesicular nuclei, inconspicuous nuclei and scanty cytoplasm. The mitotic count was 8/10 HPF. Immunohistochemistry was performed that showed tumor cells were positive for epithelial membrane antigen (EMA), TLE-1 and CD99. It was only patchy positive for CKAE1/AE3. Tumor cells were negative for p63, S-100, myogenin and caldesmon (Table 1); these were conclusive for diagnosis of synovial sarcoma.
Table 1: Tumor markers involved in immunohistochemical
staining for diagnostic purposes of present case.
|
Antibody |
Reaction |
|
CKAE1/AE3 |
Patchy Positive |
|
Caldesmon |
Negative |
|
Myogenin |
Negative |
|
S-100 |
Negative |
|
TLE-1 |
Positive |
|
EMA |
Positive |
|
CD99 |
Positive |
|
Bcl-2 |
Positive |
|
CD34 |
Negative |
Figure 4: Frontal view of the patient with large exophytic mass protruding through the left orbit.
She received 2 cycles of neoadjuvant chemotherapy AIM protocol followed by wide local excision, however, the margin status could not be ascertained. Subsequently, treatment with a total of 60 Gy adjuvant radiotherapy was given via 2D technique using 2 parallel opposed fields, off cord after 44 Gy and optic nerve shield at 50 Gy. The patient tolerated the treatment well and was on surveillance. She remained disease free for approximately 4.5 years. She then developed biopsy-proven recurrence at the primary site; her metastatic workup was negative. Unfortunately, the patient was lost to follow-up for 2 years, and then she presented with a very large lobulated mass involving the left infratemporal fossa (Figure 4) now measuring 6.2 × 7.6 × 6.3 cm, encasing ramus of mandible, temporomandibular joint and muscle of mastication with intra-orbital extension. She received second-line chemotherapy with gemcitabine and docetaxel (palliative intent). However, she did not tolerate the chemotherapy well. Subsequently, she developed massive tumor bleeding (Figure 5) and received palliative radiation (30 Gy in 10 fractions) for bleeding and pain control. Patient is now on the best supportive care, her general condition deteriorating rapidly with the passage of time.
Figure 5: The patient after an episode of massive tumor bleeding.
Discussion
In contrast to its name, synovial sarcoma rarely originates from the synovial membrane [2]. It is most commonly found near large joints. It is very uncommon to be found in the head and neck region, as the location is poor in synovial tissue [3]. It is estimated that approximately 8-10 % of all soft tissue sarcomas are synovial sarcoma, and only 3-5% occur in the head and neck region [4, 5]. In the head and neck region, the most common sites involved are the hypopharynx, retropharyngeal and parapharyngeal spaces [6]. The male-to-female ratio is 3:2 and age predilection is between 25 and 36 years [5]. Generally, these types of tumors remain asymptomatic until they are large enough to produce compressive effects on neighbouring structures [4]. Synovial sarcoma has 4 subtypes: monophasic epithelial, monophasic, biphasic and poorly differentiated (round cell) tumors [7]. For diagnostic purposes, it is important to include head, neck, and chest computed tomography to define the local extent of disease and metastasis [5].
As there are no standard treatment protocols for synovial Sarcoma of the head and neck, therefore the optimal treatment regimens remain unclear [8]. Surgical resection with a wide margin to limit local recurrence is the mainstay of treatment [9]. Unfortunately, margin-negative surgery is not easy to achieve in the head and neck region. Multimodality approach consisting of extensive radical local excision, postoperative radiation therapy, and chemotherapy is often recommended. To improve local control if resection is not adequate, radiotherapy plays an important role [10].
In general, chemotherapy for head and neck synovial sarcomas should be considered only for cases with poor prognostic factors, such as large tumor size (>5 cm) or an unfavorable site of presentation [8]. The role of chemotherapy is controversial and with questionable survival benefits [11]. These tumors are precursors of a more serious prognosis, regardless of treatment modality with, a 5-year overall survival ranging from 40-70%, which was consistent with our patient’s experience. The recurrence rate of synovial sarcoma is approximately 40% in resection with positive margins. [9]. Recurrence typically exhibits in the first 2 years after initial therapy. In the case of our patient, recurrence occurred after 4.5 years of initial treatment.
Synovial sarcoma commonly metastasizes to the lungs, followed by lymph nodes and bone marrow [12]. Despite being a slow-growing tumor, the long-term survival for synovial sarcoma anywhere in the body is unfortunately unfavorable [13]. Head and neck synovial sarcoma are aggressive in nature and often confer a poor prognosis [14]. Prognosis factors generally include tumor size, site of cancer, grade of malignancy, age older than 60 years and presence of metastatic disease [15].
Conclusion
Synovial sarcoma of the retromolar trigone is a rare malignant tumor with a poor prognosis. As there is no standard treatment protocol for synovial sarcomas of the head and neck, optimal antineoplastic treatment remains unclear. Mainstay of treatment is surgical resection with high relapse rates. Radiation therapy, with or without chemotherapy, appears to improve survival.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Tue 06, Sep 2022Accepted: Wed 21, Sep 2022
Published: Mon 03, Oct 2022
Copyright
© 2023 Asma Saleem. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJCST.2022.03.03
Author Info
Asma Saleem Syed Amir Maqbool Syed Muhammad Huzaifa Shah Muhammad Atif Waqar
Corresponding Author
Asma SaleemDepartment of Radiotherapy, Karachi Institute of Radiotherapy & Nuclear Medicine (KIRAN), Karachi, Pakistan
Figures & Tables
Table 1: Tumor markers involved in immunohistochemical
staining for diagnostic purposes of present case.
|
Antibody |
Reaction |
|
CKAE1/AE3 |
Patchy Positive |
|
Caldesmon |
Negative |
|
Myogenin |
Negative |
|
S-100 |
Negative |
|
TLE-1 |
Positive |
|
EMA |
Positive |
|
CD99 |
Positive |
|
Bcl-2 |
Positive |
|
CD34 |
Negative |



References
1.
Wenig BM (1993) Synovial sarcoma: Atlas of head and neck
pathology. Philadelphia: WB Saunders Co 263-264.
2.
Betal D, Babu R, Mehmet V (2009) Monophasic synovial sarcoma
of the pharynx: a case report. Int Semin Surg Oncol 6: 9. [Crossref]
3.
Bukachevsky RP, Pincus RL, Shechtman FG, Sarti E, Chodosh P
(1992) Synovial sarcoma of the head and neck. Head Neck 14: 44-48. [Crossref]
4.
Saydam L, Kizilay A, Kalcioglu MT, Mizrak B, Bulut F (2002)
Synovial sarcoma of the pharynx: a case report. Ear Nose Throat J 81:
36-39. [Crossref]
5.
Balakrishnan V, Flatman S, Dixon BJ, Lyons B (2012) Synovial
sarcoma of the pharynx causing airway obstruction. Med J Aust 196:
72-73. [Crossref]
6.
Shaariyah MM, Mazita A, Masaany M, Razif MY, Isa MR et al.
(2010) Synovial sarcoma: a rare presentation of parapharyngeal mass. Chin J
Cancer 29: 631-633. [Crossref]
7.
Rong R, Doxtader EE, Tull J, de la Roza G, Zhang S (2010)
Metastatic poorly differentiated monophasic synovial sarcoma to lung with
unknown primary: a molecular genetic analysis. Int J Clin Exp Pathol 3:
217-221. [Crossref]
8.
Harb WJ, Luna MA, Patel SR, Ballo MT, Roberts DB et al.
(2007) Survival in patients with synovial sarcoma of the head and neck:
association with tumor location, size, and extension. Head Neck 29:
731-740. [Crossref]
9.
Crowson MG, Lalich I, Keeney MG, Garcia JJ, Price DL (2015)
Clinicopathologic factors and adjuvant treatment effects on survival in adult
head and neck synovial cell sarcoma. Head Neck 37: 375-380. [Crossref]
10. Song
S, Park J, Kim HJ, Kim IH, Han I et al. (2017) Effects of Adjuvant Radiotherapy
in Patients With Synovial Sarcoma. Am J Clin Oncol 40: 306-311. [Crossref]
11. Kampe
CE, Rosen G, Eilber F, Eckardt J, Lowenbraun S et al. (1993) Synovial sarcoma.
A study of intensive chemotherapy in 14 patients with localized disease. Cancer
72: 2161-2169. [Crossref]
12. S
Meer, H Coleman, M Altini (2003) Oral synovial sarcoma: a report of 2 cases and
a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod
96: 306-315. [Crossref]
13. Carrillo
R, Rodriguez Peralto JL, Batsakis JG (1992) Synovial sarcomas of the head and
neck. Ann Otol Rhinol Laryngol 101: 367-370. [Crossref]
14. Ramamurthy L, Nassar WY, Hasleton PS, Gattamaneni HR, Orton CI (1995) Synovial sarcoma of the pharynx. J Laryngol Otol 109: 1207-1210. [Crossref]
15. Ameerally PJ, Sira SK, Barrett AW, Hollows P (2004) Synovial sarcoma of the hard palate. Br J Oral Maxillofac Surg 42: 261-263. [Crossref]
