Surgical Outcome of Anterior Encephalocele: Report of Two Cases and Review of Literature
A B S T R A C T
Anterior encephalocele is unusual neurosurgical condition seen worldwide. We managed two cases of anterior encephalocele: a five-day old neonate that presented with fronto-ethmoidal swelling noticed since birth. Clinical and radiological evaluations (computerised tomography scan) were in keeping with fronto-ethmoidal encephalocele. The patient had excision and duroplasty via an extracranial-lesional approach. There was excellent post-operative recovery and good cosmetic appearance. The second case was a 6-month-old infant who was diagnosed with ethmoidal encephalocele and congenital hydrocephalus, had ventriculoperitoneal shunt, excision and repair of encephalocele and cranioplasty using autogenous bone graft had remarkable post-operative recovery and was discharged home.
Keywords
Fronto-ethmoidal encephalocele, surgical outcome, neonate
Introduction
Fronto-ethmoidal (anterior) encephalocele is a congenital malformation characterised by protrusion of intracranial contents through a defect in the skull at the junction of the frontal and ethmoidal bones [1, 2]. The incidence of encephalocele has been reported as 1 in 5,000 to 10,000 live births [3-5]. The incidence of anterior encephalocele compared to occipital encephalocele is higher in tropical regions like Africa and Asia [1]. While the ratio of occipital (posterior) to sincipital (anterior) in Europe and America varies from 2.5:1 to 15:1 [6].
The exact cause of anterior encephalocele is unknown but risks factors include; genetic aberration and environmental factors like aflatoxin, ochratoxin, found in stored farm products have been implicated [3, 4, 7]. Various theories concerning pathogenesis of fronto-ethmoidal encephalocele have been proposed, but the most accepted theorized by Sternberg: states that, the development of fronto-ethmoidal encephalocele could be related to a disturbance in the closure of the rostral neuropore during end of 3rd week of intrauterine life. This disturbance leads to sustained adhesions between neuroectoderm and surface ectoderm at the site of final closure between the nasal fields [8]. Fronto-ethmoidal encephalocele has been classified by Suwanwela and Suwanwela into naso-frontal, naso-ethmoidal and naso-orbital [9]. Neuro-imaging like computerised tomography scan of the brain aids to demonstrates the site, the size of the defect, the characteristics of the tissues within the lesion and the presence of associated anomalies of the brain [10].
The goals of surgery are: Excision of non-functional herniated brain tissue and water-tight dural closure, early prevention of rupture of thin sac and associated complications like infections, bleeding and drainage of cerebrospinal fluid and cranio-facial reconstruction to achieve acceptable cosmesis. Timing of surgery has been a subject of debate, some recommend delay surgery till child is 6-10 months old or when the baby’s weight is 6-8kg [11, 12]. While others suggest early surgery to minimise the pressure effect of the lesion on the facial growth [11].
In our setting, we opted for early surgical intervention in the first case neonatal period to reduce the risks of spontaneous rupture and meningitis, eliminates mother’s/ family distress of having an abnormal child; which may affect the parental care, love and overall survival of the child. The objective of this report was to highlight the management outcome of two cases of rarely reported anterior encephalocele seen in our centre.
Case Presentation
I Case 1
A 5 days old female neonate presented with midline fronto-ethmoidal swelling noticed since birth (Figure 1). There was no associated swelling in any other part of the body, no difficulty in breathing or refusal to breast feeds. There was history of poorly treated maternal febrile illness, mother has not had antenatal care and lives in a rural area about 350KM away from a neurosurgical centre. The child was delivered at home unsupervised and was reported to cry at birth, no history of delivery of a child with any congenital anomaly in the family. Both parents appeared worried about the health of their child.
On examination, we found an active neonate, with a fronto-ethmoidal mass with visible veins, non-tender, soft and cystic, measuring about 20 x10 x 8cm, compressing over the nasal bridge and flattening the nose. Occipito-frontal circumference was 32cm (normal for age) (Figure 1).
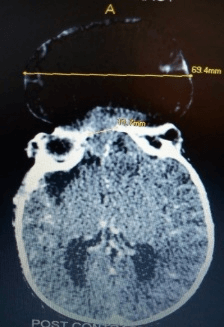
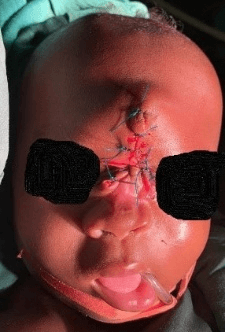
Cranial computerised tomography scan showed a huge mixed density mass with an ethmoidal skull defect measuring about 11.7mm and widest diameter of the lesion about 69mm (Figure 2). Full blood counts and serum electrolytes urea and creatinine were normal. Patients had total excision of the mass via a fronto-facial incision around the lesion, water-tight duroplasty and refreshing of the bone edges around the defects to stimulates osteogenesis (Figures 3 & 4). A firm plastic needle cover of 2ml syringe was used as stent in the nostrils to prevent nasal obstruction from post-operative oedema (Figure 4). Antibiotics were given for five days. Patient had good post-operative recovery and acceptable cosmesis to both the Neurosurgeons and the parents (Figure 5). In addition, parents were very happy and discharged home to see clinic for follow up.
Figure 1: (pre-operative picture).
Figure 2: (Axial cut CT scan).
Figure 3: (intra-operative picture).
Figure 4: (immediate Post-op).
Figure 5: (2 weeks’ post-op).
II Case 2
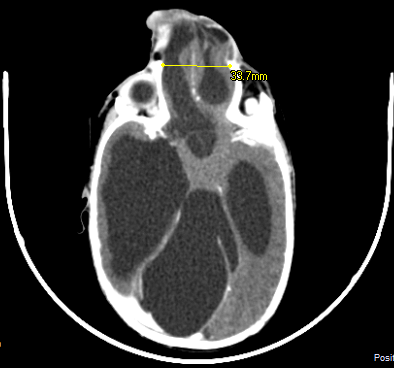
We managed a 6-month-old male infant referred from a rural hospital with progressive midline ethmoidal swelling and head enlargement noticed since birth (Figure 6). There was history of maternal febrile illness, mother has not had antenatal care and lives in a rural area. The child was delivered at home unsupervised and was reported to cry at birth, no family history of similar condition. On examination, we found an active infant, with ethmoidal mass, non-tender, soft and cystic, measuring about 10 x12 x 8cm, compressing over the nasal bridge and flattening the nose. Occipito-frontal circumference was 47cm (98.8= Percentile, 2.3=Z score). Cranial computerised tomography scan showed marked dilatation of lateral and third ventricles with a huge mixed density ethmoidal mass communicating with the frontal horn of the lateral ventricle and a bony defect measuring 39.8mm in its widest diameter (Figure 7). Full blood counts and serum electrolytes urea and creatinine were normal. Patient had ventriculo-peritoneal shunt, total excision of the mass via a facial incision around the lesion, water-tight duroplasty and cranioplasty using autogenous bone graft harvested from patient’s parietal eminence at the same sitting (Figure 8). Antibiotics were given for seven days. Patient had good post-operative recovery and acceptable cosmesis.
Figure 6: Preoperative photograph.
Figure 7: Cranial CT scan of the patient.
Figure 8: Post-operative clinical photograph.
Discussion
Fronto-ethmoidal encephalocele is an uncommon congenital neurosurgical anomaly seen worldwide [11]. Reports by several Authors have shown female preponderance which differ with the index reports that showed equal sex preponderance [6, 9]. Our present cases were born by parents who are rural dwellers. Previous earlier studies have demonstrated a higher occurrence of encephalocele in individuals with low socio-economic status, living in rural areas, due to consumption of stored farm products containing aflatoxins and other teratogens [3, 4, 7]. The parents of the first patient were worried about giving birth to a child with congenital malformation with disfigured facie. This spurred us to offer the child surgical intervention at neonatal period, despite existing problems of poor paediatric anesthesia and predicted high neonatal neurosurgical mortality. We were convinced by the fact that; parents’ acceptance and care is necessary for survival of the child in our setting.
Several surgical approach for this lesion has been proposed including transcranial, extracranial and combination of both. We opted for an extracranial-lesional approach, because it’s simple, less invasive, less risks of complications and have favorable outcome especially in neonatal period where extensive neurosurgical operations can be followed by fatal outcomes. Generally, the outcome of anterior encephalocele is better compared to posterior encephalocele (100% versus 55%) [6]. In comparison, the index cases had very good outcome, with no post-operative complication recorded and cosmetic appearance was acceptable.
Conclusion
Fronto-ethmoidal encephalocele is a rare congenital anomaly. Surgical intervention can be offered at any age presentation to minimise medical and social problems that could be associated with the condition.
Article Info
Article Type
Case Report & Review of LiteraturePublication history
Received: Thu 26, Dec 2019Accepted: Fri 17, Jan 2020
Published: Thu 30, Jan 2020
Copyright
© 2023 Aliyu Muhammad Koko. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSR.2019.01.08
Author Info
NJ Ismail Aliyu Muhammad Koko B.B Shehu Lasseini A
Corresponding Author
Aliyu Muhammad KokoDepartment of neurosurgery, regional centre for neurosurgery Usmanu Danfodiyo University Teaching Hospital Sokoto, Nigeria
Figures & Tables





References
- Anthony DH, John GM, Adam RK, Jeffrey VR, Geoffrey LK (2001) Frontoethmoidal Encephaloceles: Reconstruction and Refinements. J Craniofac Surg 12: 6-18. [Crossref]
- Xiang Y, Xiaolin A, Seidu AR, Jianguo XA () Silent Congenital Ethmoidal Encephalocele Progressing into Frontoethmoidal Meningoencephalocele with Episodic Seizures in Adulthood: A Case Report and Literature Review. Advances in Bioscience and Clinical Medicine 2203-1413.
- Dhirawani RB, Gupta R, Pathak S, Lalwani G (2014) Frontoethmoidal encephalocele: Case report and review on management. Ann Maxillofac Surg 4: 195-197. [Crossref]
- Tanwir A, Bukhari S, Shamim MS (2018) Frontoethmoidal encephalocele presenting in concert with schizencephaly. Surg Neurol Int 9: 246.
- Ecmel S, Saffet M, Tahir G, Ufuk B, Cenk G et al. (1999) Management of Frontoethmoidal (sincipital) encephalocele. J Craniofac Surg 10: 135-139. [Crossref]
- Dubey D, Pande S, Dubey P, Sawhney A (2011) A Case of Naso-Ethmoidal Meningoencephalocele. International Journal of Collaborative Research on Internal Medicine & Public Health 3: 666-669.
- Ramdurg SR, Sukanya M, Maitra J (2015) Pediatric encephaloceles: A series of 20 cases over a period of 3 years. J Pediatr Neurosci 10: 317-320. [Crossref]
- Eelco WH, Christl VK (1997) Frontoethmoidal encephalocele, a study of their pathogenesis. Pediatr Neurosurg 27: 246-256. [Crossref]
- Ahmad RA, Selvapragasam T (2008) Frontoethmoidal Encephalocele: Treatment and Outcome. J Craniofac Surgery 19: 175-183. [Crossref]
- AK Mahapatra, A Suri (2002) Anterior Encephaloceles: A Study of 92 Cases. Pediatr Neurosurg 36: 113-118. [Crossref]
- Loubna R, Amina B, Abdeslam E, Malek B, Abdessamad E (2015) Neurosurgical management of anterior meningo-encephaloceles about 60 cases. Pan African Medical Journal 21: 215.
- Ngiep O, Frédéric L, Jim G, Louisa D, Bruno J et al. (2010) Frontoethmoidal meningoencephalocele: appraisal of 200 operated cases. J Neurosurg Pediatr 6: 541-549. [Crossref]
