Journals
Surgical Management of Primary Pulmonary Mucoepidermoid Carcinoma of the Proximal Left Mainstem Bronchus
A B S T R A C T
A 29-year-old non-smoking female with a history of recurrent AML presented with worsening dyspnea. A CT scan revealed an 8 X 7 mm polypoid soft tissue nodule 8 mm distal to the carina in the left mainstem bronchus. She was brought to the operating room and a nearly obstructing soft fleshy tumor in the left mainstem bronchus just distal to the carina was removed with bronchoscopy. Pathology revealed a low grade mucoepidermoid carcinoma 0.8 cm in largest dimension with negative margins. The patient returned for a resection and was intubated with a right mainstem double lumen tube and placed in left lateral decubitus. After posterolateral thoracotomy, the azygos vein was divided to mobilize the esophagus and retract it laterally. Level 4 and 7 lymph node dissection were performed to obtain access to the anterior tracheal and subcarinal spaces. There was minimal dissection lateral to the trachea to minimize risk of ischemia. One centimeter of trachea just proximal to the carina was circumferentially isolated with umbilical tape for retraction. We bronchoscopically confirmed the location for transection and advanced a jet ventilator catheter distally. We resected one centimeter of left mainstem bronchus. We inspected the lumen of the airway to confirm no gross residual disease and confirmed negative pathologic margin before performing an end-to-end anastomosis with interrupted absorbable sutures under both jet and cross-table ventilation. Postoperatively, the patient had an uncomplicated course and was discharged without any supplemental oxygen on postoperative day 6. Final pathology was low grade mucoepidermoid carcinoma, T1aN0.
Keywords
primary mucoepidermoid carcinoma, airway resection, multidisciplinary tumor board
Introduction
Mucoepidermoid carcinoma is a rare cancer that is defined as a salivary gland type tumor that is made up of mucus-secreting, squamous, and intermediate cell types [1, 2]. Primary pulmonary mucoepidermoid carcinoma (PMEC) was first described in 1952 by Smetana et al. and comprises roughly 0.1-0.2% of all pulmonary cancers [3]. The lungs are the most common extra salivary gland site due to the presence of submucosal glands lining the tracheobronchial tree [4, 5]. Like many rare diseases, the low incidence of PMEC limits our ability to create treatment algorithms. Histologic grade, cancer stage, and lymph node metastasis are independent prognostic factors for PMEC [6, 7]. Because of the potential for recurrence and metastasis, many believe surgery that achieves an R0 resection can be a definitive treatment for PMEC [6, 8-10]. Here we report an experience in treating a patient with a symptomatic mucoepidermoid carcinoma of the left mainstem bronchus.
Case Report
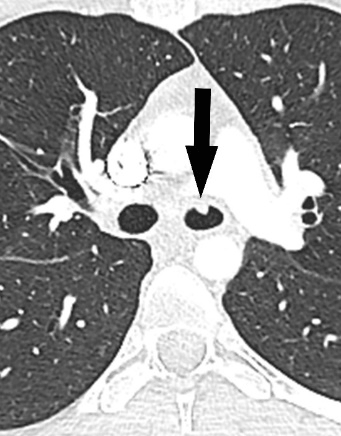
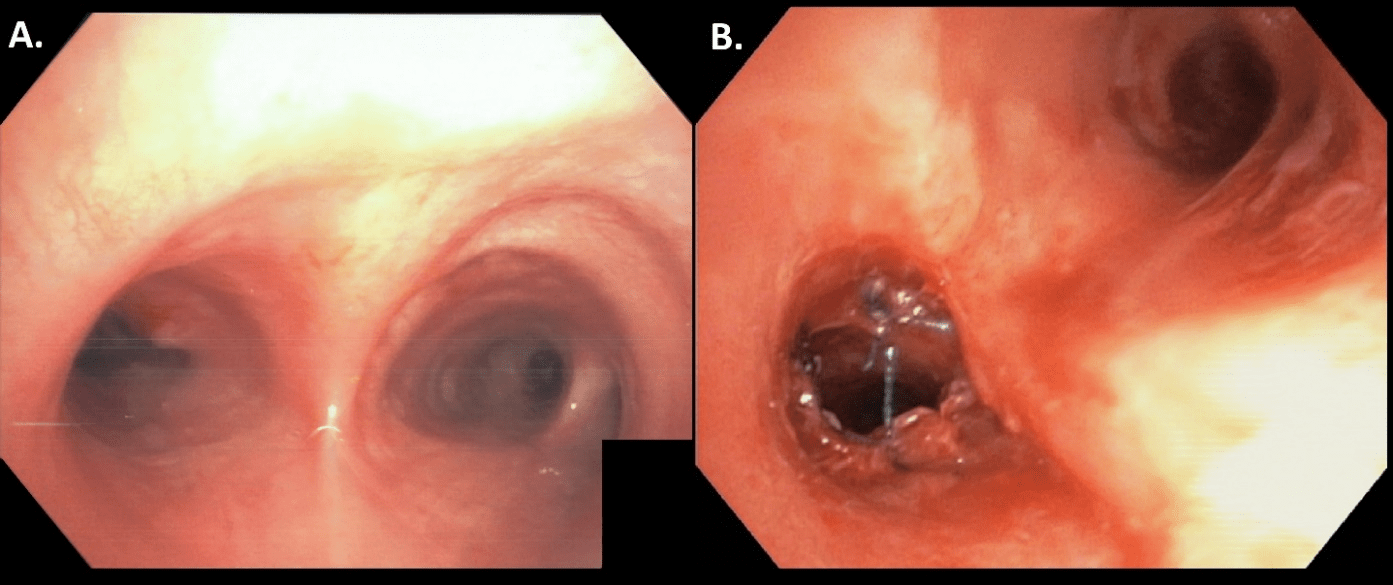
A 29-year-old non-smoking female with a history of recurrent acute myeloid leukemia presented with worsening dyspnea while lying flat for 2 to 3 months. Her oncologic history is significant for an AML 8 years ago. She was treated with chemotherapy as well as a stem cell transplant but subsequently was developed a recurrence and underwent induction with fludarabine and high dose cytosine (FLA) followed by 10 cycles of Dacogen. A computed tomography (CT) scan of the chest identified an 8 X 7 mm polypoid soft tissue nodule roughly 8 mm distal to the carina in the left mainstem bronchus with no additional findings (Figure 1B). Upon review of previous CT scans, there was evidence of slow growth of the lesion over three years (Figure 1A).
Figure 1A: On axial CT (lung window), a 4 mm nodule (arrow) arising from the anterior wall of the left main bronchus was misinterpreted as adherent mucus. 1B:On axial CT (lung and mediastinal windows) one year later, the tumor (arrow) nearly obliterates the lumen, without notable extension into the mediastinum.
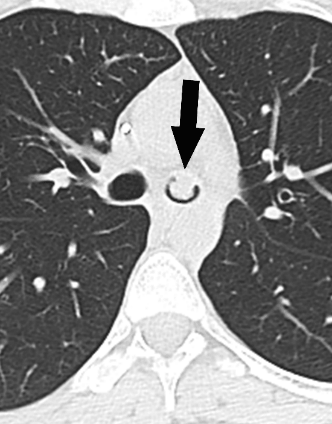
Figure 2: View of the left mainstem bronchial orifice after bronchoscopic resection and laser ablation of the near obstructing tumor just distal to the carina (arrow).
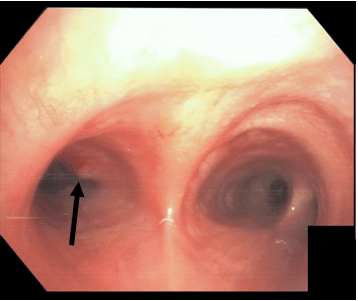
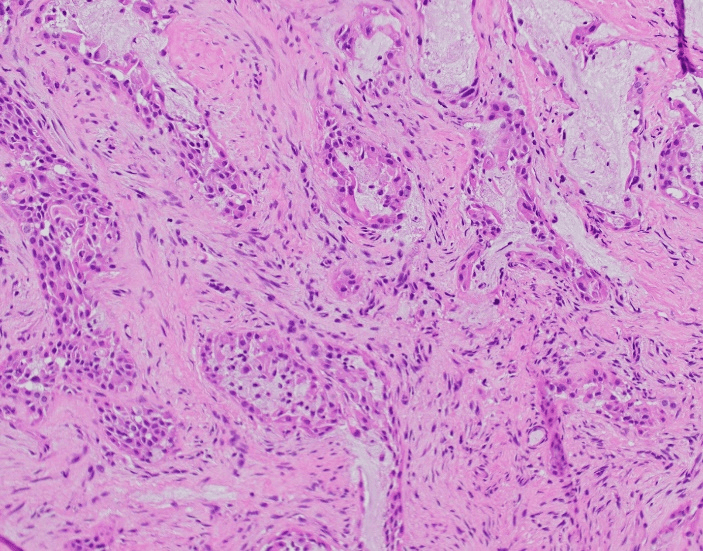
The patient was brought to the operating room and a nearly obstructing soft fleshy tumor in the left mainstem bronchus just distal to the carina was seen on flexible bronchoscopy (Figure 2). Biopsy forceps were used to detach the nodule and ND:YAG laser was used to cauterize the bleeding base. The final pathology was a 0.8 cm in largest dimension invasive malignant neoplasm composed of three cell types, mucin-producing cells, squamoid cells and the smaller intermediate cells in a solid growth pattern and forming mucinous cystic spaces filled with mucin (Figure 3). The neoplastic were negative for TTF-1 and Napsin-A, arguing against a lung primary tumor. Fluorescence in-situ hybridization (FISH) studies showed a MAML2 gene rearrangement. Overall, the histologic features, together with the immunoprofile and the presence of MAML2 gene rearrangement are diagnostic of low grade mucoepidermoid carcinoma. A PET-CT scan with IV contrast was obtained to evaluate the mediastinum and the revealed no lymphadenopathy or any FDG avidity. Additional bronchoscopic biopsies 0.5 cm proximally and distally from the lesion were found to be free of malignancy.
Figure 3: Hematoxylin and eosin section of the left mainstem bronchus tumor shows a mucoepidermoid carcinoma. Note the characteristic three cells population, the mucin-producing cells, the squamoid cells and the intermediate cells. The carcinoma grows in a solid pattern with cystic spaces (200x magnification).
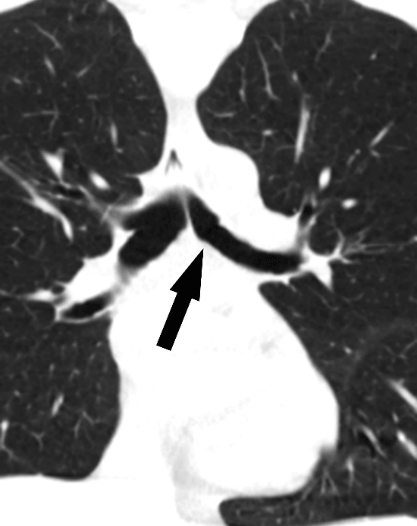
Two weeks later, she was taken to the operating room to undergo a sleeve resection as definitive surgical treatment. The patient was intubated with a right mainstem double lumen tube and placed in left lateral decubitus position. Right postero-lateral thoracotomy was performed in the 5th intercostal space. An intercostal muscle flap was created upon entry. After the azygos vein was divided, the esophagus was mobilized at the level of the carina and retracted laterally with a penrose drain. A level 4 lymph node dissection was performed to obtain access to the anterior tracheal plan. There was minimal dissection lateral to the trachea to minimize risks of ischemia. One centimeter of trachea just proximal to the carina was circumferentially isolated with umbilical tape for retraction. Additionally, level 7 lymph node dissection was performed to expose the carina and left mainstem bronchus. We bronchoscopically confirmed the location for transection and advanced a jet ventilator catheter distally. We removed roughly one centimeter of left mainstem bronchus. On frozen section, the distal margin was negative, but the proximal margin required an additional one millimeter resection for a negative margin. We inspected the lumen of the airway once more bronchoscopically and performed an anastomosis with interrupted absorbable sutures (Figure 4). This was done with both jet and cross-table ventilation to ensure adequate oxygenation. Ventilation with the anastomosis submerged revealed no leak, and the patient was extubated in the operating room. Postoperatively, she did well. The patient was discharged without any supplemental oxygen on postoperative day 6. A follow-up CT scan showed a well healed left mainstem bronchial anastomosis (Figure 5). Final pathology was low grade mucoepidermoid carcinoma, T1aN0 (16 lymph nodes sampled). No systemic therapy was given for the mucoepidermoid carcinoma, and surveillance was continued for her AML recurrence.
Figure 4: After the left mainstem bronchus was resected and negative margins were achieved, an end to end anastomosis with interrupted absorbable sutures was performed.
Figure 5: On postoperative CT (coronal lung window), the tumor has been completely resected (arrow).
Discussion
Pulmonary mucoepidermoid carcinomas are salivary gland type tumors that are comprised of mucous secreting, squamous, and intermediate cell types [1, 2]. Since the first presented case in 1952, the incidence of PMEC remains low at 0.1 to 0.2% of all pulmonary cancers. In a recent literature review of 9 studies totaling 695 cases, the majority of cases were low to intermediate grade. Distribution of disease in the tracheobronchial tree was relatively uniform in the reported cases, with the left upper lobe division being the most frequent [11]. The literature suggests that factors predicting aggressive tumor behavior include older age, presence of nodal metastasis, and high histologic grade. Regardless of the grade, in the absence of nodal disease surgical intervention with the goal of an R0 resection is generally recommended and can result in better long-term survival [6, 8-10]. While the use of adjuvant therapy is recommended when complete resection is not possible, the utility of chemotherapy and radiotherapy in these cases remains controversial.
Careful work-up is recommended to evaluate for proper operative planning, which includes PET scan, CT scan, and sometimes additional bronchoscopy with biopsy. Advanced disease at the time of diagnosis can complicate surgical intervention, especially in the setting of high grade PMEC. In the case presented, the location of the lesion mandated a left mainstem bronchus sleeve resection. What further complicated achieving a R0 resection was its close proximity to the carina and as well as its laterality. A right posterolateral thoracotomy can be performed to ensure adequate exposure to the distal trachea as well as the proximal left mainstem bronchus. After initial resection of the tumor, additional proximal and distal specimens may need to be sent for frozen section analysis. Adequate dissection of both the proximal and distal airways (while preserving their lateral blood supply) should be performed to ensure the anastomosis is tension free.
Conclusion
Primary PMEC is a rare disease of the tracheobronchial tree. While high grade lesions may portend to worse outcomes, R0 resection may offer the best oncologic results. Adjuvant therapy remains controversial as its benefit is still up for debate in a node negative lesion following complete resection.
Disclosures
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Article Info
Article Type
Case ReportPublication history
Received: Thu 30, May 2019Accepted: Fri 21, Jun 2019
Published: Thu 29, Aug 2019
Copyright
© 2023 Rajeev Dhupar. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2019.02.05
Author Info
Patrick G. Chan Chigozirim Ekeke Diane Strollo Ernest G. Chan Humberto E Trejo Bittar James D. Luketich Rajeev Dhupar
Corresponding Author
Rajeev DhuparDepartment of Cardiothoracic Surgery, University of Pittsburgh School of Medicine
Figures & Tables
References
- SMETANA HF, IVERSON L, SWAN LL (1952) Bronchogenic carcinoma; an analysis of 100 autopsy cases. Mil Surg 111: 335-351. [Crossref]
- Seifert G (1997) [Diagnosis and prognosis of salivary gland tumors. An interpretation of new revised WHO classification]. Mund Kiefer Gesichtschir 1: 252-267. [Crossref]
- Shen C, Che G (2014) Clinicopathological analysis of pulmonary mucoepidermoid carcinoma. World J Surg Oncol 12: 33. [Crossref]
- Molina JR, Aubry MC, Lewis JE, Wampfler JA, Williams BA et al. (2007) Primary salivary gland-type lung cancer: spectrum of clinical presentation, histopathologic and prognostic factors. Cancer 110: 2253-2259. [Crossref]
- Turnbull AD, Huvos AG, Goodner JT, Foote FW Jr. (1971) Mucoepidermoid tumors of bronchial glands. Cancer 28: 539-544. [Crossref]
- Jun-jie Xi, Wei Jiang, Shao-hua Lu, Chun-yan Zhang, Hong Fan et al. (2012) Primary pulmonary mucoepidermoid carcinoma: an analysis of 21 cases. World J Surg Oncolo 10: 232. [Crossref]
- Yousem SA, Hochholzer L (1987) Mucoepidermoid tumors of the lung. Cancer 60: 1346-1352. [Crossref]
- Zhang XP, Hu PZ, Shen SS, Li XY (2018) [Clinical characteristics and prognostic analyses of 87 patients with pulmonary mucoepidermoid carcinoma]. Zhonghua zhong liu Za zhi 40: 452-455. [Crossref]
- Alessandro G. Fois, Gabriella Diana, Antonella Arcadu, Viviana Marras, Paola Crivelli et al. (2017) Bronchial mucoepidermoid carcinoma: A case report. Int J Surg Case Rep 31: 159-162. [Crossref]
- Kang DY, Yoon YS, Kim HK, Choi YS, Kim K et al. (2011) Primary salivary gland-type lung cancer: surgical outcomes. Lung Cancer 72: 250-254. [Crossref]
- Xuanguang Li , Zhibin Guo, Jinghao Liu, Sen Wei, Dian Ren et al. (2018) Clinicopathological characteristics and molecular analysis of primary pulmonary mucoepidermoid carcinoma: Case report and literature review. Thorac Cancer 9: 316-323. [Crossref]
