Surgical Management for Acute Occlusion of the Left Main Coronary Artery Stenosis: A Case Series
A B S T R A C T
There is growing global attention concerning the short and long term prognosis of acute coronary syndrome (ACS) in patients with prior coronary artery bypass grafting (CABG). Significant left main coronary artery (LMCA) disease occurs in 5%-7% of patients undergoing coronary angiography, which is associated with a worse prognosis. We report a series of 3 patients presenting with LMCA disease out of which one patient successfully underwent CABG, and two patients managed with optimal medical therapy.
Keywords
Left main coronary artery (LMCA), coronary artery bypass grafting (CABG), acute coronary syndrome (ACS), acute myocardial infarction (AWMI)
Introduction
The various anatomic types of obstructive coronary artery disease (CAD), significant left main coronary artery (LMCA) disease is the highest risk lesion subset and is associated with poorer clinical outcomes compared with the non-LMCA disease [1]. Based on early clinical trials demonstrating a definite survival benefit of coronary artery bypass grafting (CABG) over medical therapy [2]. CABG has been the standard of care for the revascularization of significant LMCA disease for a long time. Percutaneous coronary intervention (PCI) was performed on a limited basis, mostly in surgically ineligible patients. PTCA for LMCA disease has become technically feasible and shows favourable clinical outcomes [3].
Case Profile
We report a case series of 2 male and one female patient aged 40-60 years, of which two patients had Anterior Wall Myocardial Infarction [AWMI] and one patient had Non-ST-elevation myocardial infarction [NSTEMI]. Table 1 shows the de¬mographic characteristics of the patients. There was no history of smoking and bleeding disorders in the family; routine blood examinations, chest X-ray, coagulation profile & comprehensive metabolic panel were normal. All three patients underwent coronary angiography, which revealed a total occlusion of LMCA, which was filling retrogradely from the right coronary artery. Subsequently, one patient underwent coronary artery bypass surgery [CABG], one patient was not willing for CABG, and one patient was medically managed as MPI revealed nonviable myocardium (Table 2). All the patients started given dual antiplatelet therapy and followed-up for 1year.
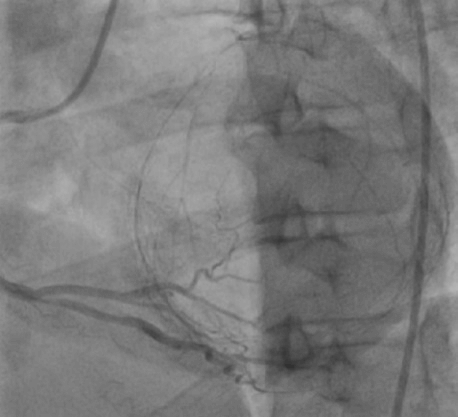
Figure 1A: Left coronary angiography showing LMCA total occlusion.
Figure 1B & 1C: Right Coronary angiography showing dominant RCA and retrograde filling.
Table 1: Demographic characteristics of the patients.
|
Patient No |
Age (years) |
Sex |
Presenting complaints |
H/o DM/HTN |
ACS |
|
I |
45 |
M |
Chest Pain |
Yes |
AWMI |
|
II |
60 |
M |
Chest pain |
Yes |
AWMI |
|
III |
55 |
F |
Breathlessness |
No |
NSTEMI |
Table 2: Angiographic & Management profile.
|
S No. |
Lesion |
Thrombolysis |
MPI |
Revascularization |
Results |
Figures |
|
1 |
LMCA Total occlusion |
Yes |
Non-transmural infarcts in the anterior wall, anteroseptal wall and apex septum is well perfused |
Medical management |
Good |
1A, 1B & 1C |
|
2 |
LMCA Total occlusion |
Yes |
Reversible Inducible Ischemia saw in the anterior wall anteroseptal and apex septum |
CABG |
Good |
2A, 2B & 2C |
|
3 |
LMCA Total Occlusion |
No |
Reversible Inducible Ischemia has seen in the anterior wall anteroseptal and apex septum |
CABG not willing Continued on Medical management |
Good |
3A, 3B & 3C |
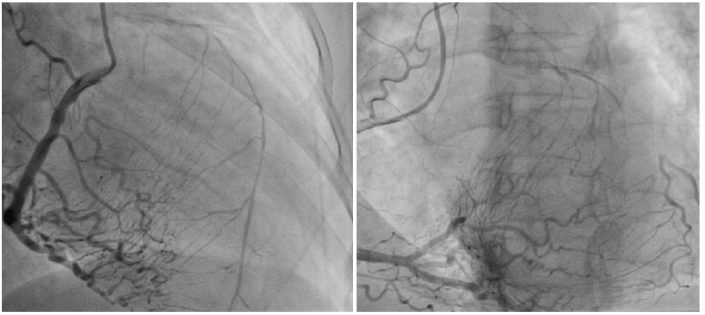
Figure 2A: Left coronary angiography showing LMCA total occlusion.
Figure 2B & 2C: Right Coronary angiography showing dominant RCA and retrograde filling.
Figure 3A: Left coronary angiography showing LMCA total occlusion.
Figure 3B & 3C: Right Coronary angiography showing dominant RCA and retrograde filling.
Discussion
Acute coronary syndrome (ACS) is a significant cause of death and morbidity among coronary artery disease patients. In recent years, the treatment of ACS patients has significantly improved, leading to a decrease in in-hospital and long-term mortality [4]. Coronary artery bypass graft (CABG) was broadly introduced in the 1970s, and since then has become one of the most common surgical procedures [5]. Despite successful revascularization and secondary prevention measures, the progression of atherosclerosis after CABG occurs both in grafts and native coronary arteries, resulting in significant morbidity and mortality, especially in patients who present with acute coronary syndromes (ACS) [6]. The Timing of surgical revascularization after acute myocardial infarction (AMI) is still controversial. Emergency CABG is recommended in patients who attempt at PCI have been unsuccessful, have signs of ischemia despite optimal medical treatment, and have complications of AMI [7].
Conclusion
The performance of CABG during the index hospitalization for ACS seems to represent a short-term mortality benefit. We conclude that early CABG should be considered more often in eligible ACS patients.
Article Info
Article Type
Case SeriesPublication history
Received: Thu 19, Mar 2020Accepted: Thu 09, Apr 2020
Published: Mon 13, Apr 2020
Copyright
© 2023 H. S. Natraj Setty. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.HCS.2020.01.02
Author Info
B.K. Geetha C.N. Manjunath H. S. Natraj Setty Jayashree Kharge P.C. Raghavendra Rahul Patil Santhosh Jadav Stawik Raj T.R. Raghu
Corresponding Author
H. S. Natraj SettySri Jayadeva Institute of Cardiovascular Sciences and Research, Bangalore, Karnataka, India
Figures & Tables
Table 1: Demographic characteristics of the patients.
|
Patient No |
Age (years) |
Sex |
Presenting complaints |
H/o DM/HTN |
ACS |
|
I |
45 |
M |
Chest Pain |
Yes |
AWMI |
|
II |
60 |
M |
Chest pain |
Yes |
AWMI |
|
III |
55 |
F |
Breathlessness |
No |
NSTEMI |
Table 2: Angiographic & Management profile.
|
S No. |
Lesion |
Thrombolysis |
MPI |
Revascularization |
Results |
Figures |
|
1 |
LMCA Total occlusion |
Yes |
Non-transmural infarcts in the anterior wall, anteroseptal wall and apex septum is well perfused |
Medical management |
Good |
1A, 1B & 1C |
|
2 |
LMCA Total occlusion |
Yes |
Reversible Inducible Ischemia saw in the anterior wall anteroseptal and apex septum |
CABG |
Good |
2A, 2B & 2C |
|
3 |
LMCA Total Occlusion |
No |
Reversible Inducible Ischemia has seen in the anterior wall anteroseptal and apex septum |
CABG not willing Continued on Medical management |
Good |
3A, 3B & 3C |





References
- Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T et al. (1994) Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet 344: 563-570. [Crossref]
- Caracciolo EA, Davis KB, Sopko G, Kaiser GC, Corley SD et al. (1995) Comparison of surgical and medical group survival in patients with left main equivalent coronary artery disease. Long-term CASS experience. Circulation 91: 2335-2344. [Crossref]
- Park SJ, Park DW (2009) Percutaneous coronary intervention with stent implantation versus coronary artery bypass surgery for treatment of left main coronary artery disease: is it time to change guidelines? Circ Cardiovasc Interv 2: 59-68. [Crossref]
- Bertrand ME, Simoons ML, Fox KA, Wallentin LC, Hamm CW et al. (2002) Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 23:1809-1840. [Crossref]
- Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD et al. (2011) Heart disease and stroke statistics-2011 update: a report from the American Heart Association. Circulation 123: e18-e209. [Crossref]
- Mangano DT (1995) Cardiovascular morbidity and CABG surgery-a perspective: epidemiology, costs, and potential therapeutic solutions. J Card Surg 10: 366-368. [Crossref]
- Ismail Cihan Ozbek, Kenan Sever, Ozkan Demirhan, Denyan Mansuroglu, Muslum Cicek et al. (2016) Timing of coronary artery bypass surgery in patients with non-ST-segment elevation myocardial infarction and postoperative outcomes. Arch Med Sci 12: 766-771. [Crossref]
