Spontaneous Isolated Superior Mesenteric Artery Dissection: A Case Report
A B S T R A C T
This report consists of a rare case of spontaneous isolated superior mesenteric artery dissection (ISMAD) of a 50 years old gentleman successfully managed with open retrograde mesenteric stent placement and patch angioplasty.
Keywords
Superior mesenteric artery, dissection
Case Report
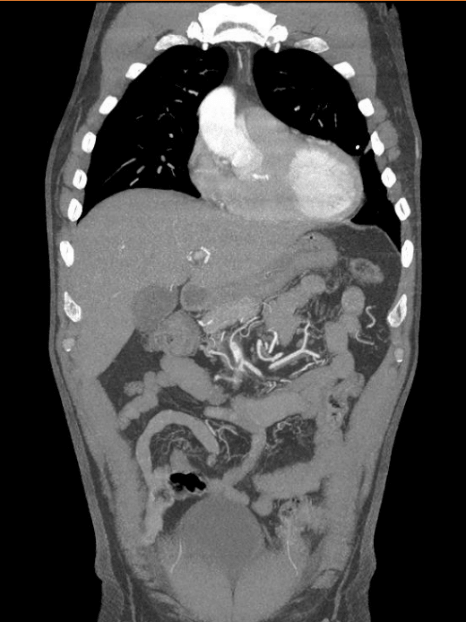
A 50-year male patient presented to the emergency department of John Hunter Hospital with 12-hour history of severe epigastric pain, which radiated to his mid back. Diaphoretic and pale on arrival, stated associated nausea and vomiting. He also noted melaena throughout the previous week, worsening in the morning of the event. His initial vital signs showed significant hypertension (205/91), with heart rate, temperature and saturation within normal limits. His initial abdominal examination was unremarkable, with a soft and non-tender abdomen. His comorbidities consisted of Coarctation of Aorta that was surgically corrected as a child, hypertension and dyslipidemia. Concern was raised about retroperitoneal perforated peptic ulcer or aortic dissection – computed tomography was then promptly organized to further elucidate his symptoms. The imaging showed an isolated superior mesenteric artery dissection (ISMAD), extending from 3cm of the origin up to 9cm.
At this point the lumen was completely occluded, and this occlusion extended for 7cm where distal filling could be appreciated (Figure 1). The end organs (small bowel and right colon) did not showed ischaemic compromise features at that stage. Decision was made to conduct the patient to the operating theatre for open exploration and stent placement. 5000UI of subcutaneous Heparin was given on induction. Intraoperative findings consisted of an extensive dissection segment from SMA origin to its third part, involving the middle colic branch. After obtaining adequate proximal control, mesenteric arteriotomy was performed. It showed a large amount of clot in the false lumen that was completely compressing the vessels true lumen.
This was subsequently evacuated and an on-table angiogram performed confirming the extensive SMA dissection from its origin. A self-expanding Nitilol stent was deployed, measuring 6mm x 150mm, and its deployment extended from SMA’s origin all the way down beyond the origin of the middle colic artery. This was all angioplastied with a 6mm x 180mm balloon. The false and true lumens were subsequently patched together with a vein patch. Excellent pulsatile flow to all SMA branches post procedure was confirmed. A repeat computed tomography angiogram day one post procedure was organized, and it also confirmed the stent patency and normal blood flow (Figure 2). Antihypertensive medications, statin and dual antiplatelet agents (aspirin and clopidogrel) were started immediately post operatively. He had an uneventful hospital recovery, being discharged in 10 days. He has been followed up with yearly mesenteric Doppler ultrasound showing excellent stent flow without evidence of stenosis. He has been asymptomatic since.
Figure 1: ISMAD imaging – diagnosis
Figure 2: Post open retrograde stent placement imaging
Literature Review
Spontaneous dissection of the SMA is considered a rare entity, where patients tend to present with unspecific abdominal symptoms. Advances in diagnostic tools such as Computed Tomography machines have certainly improved our capacity of early diagnosing this condition [1]. Several treatment options are currently available, which varies from conservative management, endovascular up to open surgical repair [2, 3].
There is still no pathophysiological evidence to how the spontaneous dissection of the SMA occurs, with speculation of the mechanism differing compared to the aortic dissection type [4]. Daoud and collaborators argue that there is some relationship between hypertension and ISMAD, but that however is yet to be proved. Treatment options for ISMAD have been shifting to less invasive tools, with most recent papers focusing on endovascular repair approach and its outcomes [5, 6]. In this current case report we opted for open retrograde repair given the patient’s florid symptomatology, which in our literature review appears to be the favored practice in this instance [2, 4, 6]. Presence of abdominal pain, peritonitis or ischaemic compromise features on imaging are the main features when opting for either endovascular stent placement or open retrograde repair as oppose to conservative management.
Two case series analyzed the median distance from SMA origin and the initial dissection point and its subsequent length [6, 7]. In both was found a median between 15 and 30mm primary tear from ostium, similarly, found in our case report (30mm). There have been 2 hypotheses that could explain this phenomenon, both involving anatomical details from this vessel. The first involves the curvature itself of the SMA, where blood flow could induce the initial intimal tear. The second entails the transition point between the adjacent fixed pancreas and SMA’s free edge into the mesenteric root [3, 6, 12]. There has been some controversy surrounding antiplatelet and anticoagulation therapy for ISMAD, with the latest literature questioning if it would be necessary at all. In our experience the patient received dual antiplatelet therapy immediately post op, which was ceased after 6-months post procedure. Gobble and collaborators analyzed the outcomes of patients who undergone expectant (i.e. in hospital observation) treatment trial, and interestingly half failed expectant management. Of this half, half died from progression of SMA dissection found in autopsy. The surviving half received endovascular stent and therefore survived. They also assessed success rate on anticoagulated group, where again half of their sample required surgical intervention (either endovascular or open). We believe that this favors early surgical intervention in symptomatic patients, which is again reinforced by the literature reviewed [3, 9, 12]. Recent papers showed that a trial of conservative management with antiplatelet agents is a reasonable and safe initial option in symptomatic ISMAD, with close inpatient monitoring and repeat imaging.
Recent papers showed that a trial of conservative management with antiplatelet agents is a reasonable and safe initial option in symptomatic ISMAD, with close inpatient monitoring and repeat imaging [8,10]. A retrospective study of 35 patients compared the outcome between symptomatic and asymptomatic groups with findings again leaning towards a more conservative approach [10]. Long term follow up and remodeling rates were found to be negligible on a large retrospective study published in 2017, reinforcing the wait-and-watch role [11]. This was contrary however to another author’s finding, where the symptomatic patients that had the best symptomatic response were in fact those who undergone endovascular treatment [13].
Conclusion
Even though ISMAD is considered rare, its diagnose has become more frequent over the last years given the improvements and widespread availability of medical imaging. Early diagnosis proves to be a key feature on patient outcome, particularly in those with symptomatic disease from imminent ischaemic events.
Article Info
Article Type
Case Report & Review of LiteraturePublication history
Received: Tue 03, Dec 2019Accepted: Tue 17, Dec 2019
Published: Thu 26, Dec 2019
Copyright
© 2023 Maria Julia Corbetta Machado. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2019.02.09
Author Info
Arvind Deshpande Maria Julia Corbetta Machado
Corresponding Author
Maria Julia Corbetta MachadoJohn Hunter Hospital, University of Newcastle
Figures & Tables

References
- Daoud H, Abugroun A, Subani A, Khalaf H (2018) Isolated superior mesenteric artery dissection: a case report and literature review. Gastroenterology Res 11: 374-378. [Crossref]
- Min SI, Yoon KC, Min SK, Ahn SH, Jae HJ et al. (2011) Current strategy for the treatment of symptomatic spontaneous isolated dissection of superior mesenteric artery. J Vasc Surg 54: 461-466. [Crossref]
- Gobble RM, Brill ER, Rockman CB, Hetch EM, Lamparello PJ et al. (2009) Endovascular treatment of spontaneous dissections of the superior mesenteric artery. J Vasc Surg 50: 1326-1332. [Crossref]
- Lv PH, Zhang XC, Wang LF, Chen ZL, Shi HB (2014) Management of isolated superior mesenteric artery dissection. World J Gastroenterol 20: 17179-17184. [Crossref]
- Li N, Lu QS, Zhou J, Bao JM, Zhao ZQ et al. (2014) Endovascular stent placement for treatment of spontaneous isolated dissection of the superior mesenteric artery. Ann Vasc Surg 28: 445-451. [Crossref]
- Dong Z, Fu W, Chen B, Guo D, Xu X et al. (2013) Treatment of symptomatic isolated dissection of superior mesenteric artery. J Vasc Surg 57: 69S-76S. [Crossref]
- Sosogi S, Sato R, Saito H, Takauji S, Sakamoto J et al. (2019) Clinical course of conservative management for isolated superior mesenteric arterial dissection. Eur J Radiol Open 24: 192-197. [Crossref]
- Ahn HY, Cho BS, Mun YS, Jang JH, Kim CN et al. (2014) Treatment results for spontaneous isolated superior mesenteric artery dissection according to our previous guidelines and collective literature review. Ann Vasc Surg 28: 1595-1601. [Crossref]
- Wang J, He Y, Zhao J, Yuan D, Xu H et al. (2018) Systematic review and meta-analysis of current evidence in spontaneous isolated celiac and superior mesenteric artery dissection. J Vasc Surg 28: 1228-1240. [Crossref]
- Kimura Y, Kato T, Nagao K, Izumi T, Haruna T et al. (2017) Outcomes and radiographic findings of isolated spontaneous superior mesenteric artery dissection. Eur J Vasc Endovasc Surg 65: 925-926. [Crossref]
- Heo SH, Kim YW, Woo SY, Park YJ, Park KB et al. (2017) Treatment strategy based on the natural course for patients with spontaneous isolated superior mesenteric artery dissection. J Vasc Surg 65: 1142-1151. [Crossref]
- Kim YW (2016) Current understandings of spontaneous isolated superior mesenteric artery dissection. Vasc Specialist Int 32: 37-43. [Crossref]
- Luan JY, Guan X, Li X, Wang CC, Li TR et al. (2016) Isolated superior mesenteric artery dissection in China. J Vasc Surg 63: 530-536. [Crossref]
