Soft Tissue Reconstruction Strategy of Spontaneous Calcaneal Fracture in a Patient with Diabetic Penetrating Foot Ulcer
A B S T R A C T
Background: Spontaneous pathologic fractures of the calcaneum in diabetic patients are rarely described in the literature. The pathologic fractures following osteomyelitis represent a possibly limb-threatening condition and if associated with a concomitant calcaneal ulcer, they present defiance for the surgeon and furthermore an outstandingly challenging condition to handle.
Methods: A 61-year-old diabetic female patient on insulin therapy has been treated for a penetrating foot ulcer. In sequence the following procedures were carried out: Negative pressure wound therapy with instillation and dwell time (NPWTi-d), Negative Pressure Wound Therapy (NPWT), arterial percutaneous angioplasty (PTA), calcanectomy and temporary arthrodesis, application of Dermal Regeneration Template (DRT) and transplantation of microfractured autologous adipose graft (LIPOGEMS®), treatment of residual dehiscence with physical cold plasma (kINPen®MED).
Results: The patient completely healed within 20 months and was able to walk without further aids.
Conclusion: The authors point to the promptness within the treatment of pathologic calcaneal fractures, whether throughout the usage of technical devices targeting the reduction of the bacterial load and stimulation of healthy tissue, like in NPWTi-d and kINPen®MED. The use of a dermal regeneration template followed by skin grafting enriched with autologous microfractured adipose tissue (LIPOGEMS®), therefore represents today the most advanced regenerative surgical procedures.
Keywords
Autologous microfractured adipose tissue, cold atmospheric plasma (CAP), dermal regeneration template (DRT), diabetic foot, NPWTi-d, spontaneous calcaneal fracture, Lipogems®
Introduction
Diabetes is a chronic systemic illness causing damage to either the vascular nervous or to the osteoarticular system and increasing the risk of infections. The calcaneus plays a fundamental role within the gait pattern and, in diabetic patients, this bone is particularly predisposed to fractures and osteomyelitis, even without a certain association with trauma [1]. Considering the analysis of Mitchell et al. the incidence of calcaneal fractures accounts for 11.5/100000 [2]. When it comes to open fractures, possible complications vary from infection, going further to limb amputation, and in the worst case to a fatal outcome [3, 4]. Here we report the case of a 61-year-old diabetic female patient suffering from a calcaneal ulcer and a consequent pathological fracture of the calcaneus, classified as type 3 according to Hedlund and also classified as A considering the Essex-Lopresti classification [1, 5]. In this patient we managed to save the limb by obtaining the complete rehabilitation of autonomous walking. Our first goal was to restore correct revascularization and subsequently we chose a conservative, biotechnological and regenerative surgical approach.
Materials and Methods
A female 61 years old patient presents at our emergency department, referring an open blister with a diameter of 1 cm localized at the left heel, with perilesional evidence of infection, evolving over the past 15 days. Formerly known for Diabetes mellitus (DM) type 2 (treated with insulin) and arterial hypertension (treated with atenolol). The patient working as a waitress, affirms that the lesion appeared after wearing new footwear. A treatment including dressings with iodopovidone and a study using a colour doppler ultrasonography of the inferior limbs were initially performed, detecting peripheral arterial vascular disease affecting the left lower extremity with a >75% stenosis of the superficial femoral artery and suspect complete occlusion of the posterior tibial artery. After performing PTA of the lower left limb, Clopidogrel was introduced. In the following weeks, despite the angiographic success of PTA, there was a worsening of the clinical picture consisting of the appearance of a wet ulcer, with a diameter of 3 cm, extending deep to the calcaneum (Figure 1).
Figure 1: Penetrating calcaneal ulcera due to preexisting high pressure.
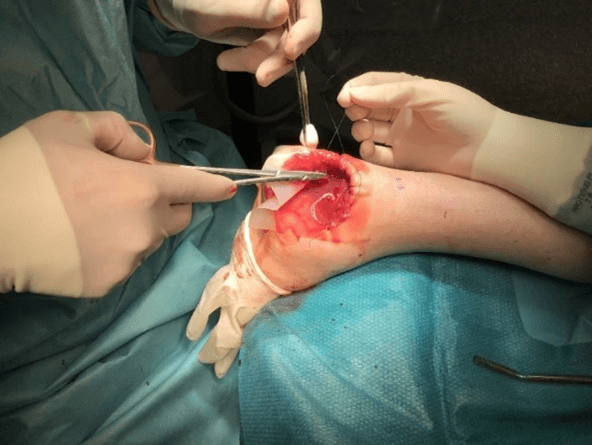
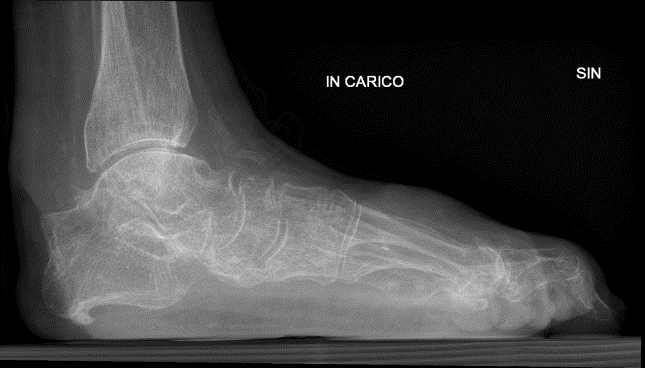
The radiologic assessment relying on RX and MRI, showed a calcaneal fracture classified as type 3 according to Hedlund and a type A meanwhile according to Essex-Lopresti (Figure 2). An antibiotic therapy consisting of Ceftriaxone iv. was administered because local biopsies showed the presence of osteomyelitis caused by E. coli. The blood tests indicated an inflammatory process with a CRP 203mg/L and WBC 15.8 x10E9/L. The patient underwent a conservative surgical therapy consisting of debridement of the necrotic tissue and pose of NPWTi-d supplemented with Octènidine. Negative pressure instillation therapy was maintained for 5 days to be subsequently replaced with conventional NPWT. Two weeks later a further debridement was performed, including samples for bacteriological analysis. In consideration of the negative result of the bacteriological cultures, a partial calcanectomy, a temporary ankle arthrodesis and the placement of a skin regeneration template (DRT) were performed (Figure 3).
Figure 2: Calcaneal fracture following penetrating ulcer.
Figure 3: Temporary arthrodesis performed contextually with partial calcanaectomy.
Five weeks later the first skin grafting was performed, leading to an attachment of about 50% of the engrafted area. In the following months the patient underwent a further debridement and skin graft, complemented with a perilesional injection of microfractured autologous adipose tissue (LIPOGEMS®), collected from the flanks and abdomen. The superficial residual dehiscence limited to the plantar region was subsequently treated with a small flap of local rotation, supplemented with daily local application of an ointment based on allantoin and polyethyleneglycol and furthermore the application of cold atmospheric plasma (CAP kINPen®MED) in a cycle of 2 weeks.
Results
This whole process leads ultimately to the complete healing of the lesion and the rehabilitation of autonomous walking, over a period of 20 months from the first clinical manifestation (Figures 4, 5 & 6).
Figure 4: Pose of a dermal matrix with the performance of running dowel suture with double passing through DRT.
Figure 5: The wound healed 20 months since the first surgery.
Figure 6: Radiological control at the end of the therapy.
Discussion
Most spontaneous heel fractures occur in the context of a diabetic foot [6]. Pathological spontaneous calcaneal fractures can also be caused by other factors such as bone loss, chronic renal failure, avascular necrosis, secondary hyperparathyroidism, smoking, drug abuse, and malnutrition [7]. The most common type within the group of calcaneal fractures is the stress fracture type. The decision in selecting the most appropriate form of treatment is influenced on one hand by the complex anatomy, on the other hand by the location and type of fracture. The cortical part of the bony structure of the calcaneum is relatively subtle in terms of a load of weight it bears [8]. The posture and mechanical stress of the foot bones, the intensity and direction of the vectors, and the mineral density of the bones are all important and decisive factors for the origin and morphology of fractures. Calcaneal insufficiency avulsions (CIA) are defined to be caused by exhaustion and are typically located around the posterior tuberosity of the calcaneum. This type of fracture is related to a long-lasting DM and its pathogenesis is based on micro-fractures resulting from stress during daily activity [9]. Initially, nondisplaced insufficiency fractures occur but later evolve into complete dislocations of the calcaneal fragments.
Even though neuropathy is the most common etiologic agent in ulcer of a diabetic foot (DFU), other factors like peripheral vascular problems, infections and anatomical malformations have to be taken in consideration [10]. About 60% of patients suffering from DFU develop osteomyelitis [11]. In case of far-reaching non-healing diabetic foot ulcers, osteomyelitis must generally be ruled out. This can be done by performing deep biopsies within the ulcer; however gold standard in non-invasive diagnostics is the MRI, having a specificity of over 90% [12, 13]. Therapeutic strategies concerning the handling of calcaneal fractures described so far include: conservative therapy, open reduction and internal fixation, calcanaectomy and arthrodesis. Contrarily the strategy of sealing the soft tissues heads to primary wound closure, closure by secondary intent, local flap or free tissue transfer [14, 15].
In our case the initial phase of treatment consisted of wound bed preparation using NPWTi-d with instillation, followed by optimization of arterial perfusion achieved with percutaneous angioplasty (PTA). A subsequent calcanectomy with temporary arthrodesis was necessary to maintain on site only the healthy tissues. The subsequent therapeutic phases involved the adoption of several tissue repair strategies through the application of Dermal regeneration template (DRT), skin grafts and NPWT [16-19]. The second skin grafting procedure was finally performed in combination with a microfractured autologous tissue transplantation to achieve a strong regenerative boost.
The regenerative boost is due to the paracrine action of adipose tissue that is composed of mature adipocytes, extracellular matrix and a stromal vascular fraction (SVF), constituted by different cells including adipose-derived stem cells (ADSCs), pericytes, endothelial cells, erythrocytes, fibroblasts, vascular smooth muscle cells, hematopoietic cells and other immune cells [20-22]. Noteworthy, recent reports have identified adipose tissue as the tissue in the body that contains the highest percentage of adult stem cells (ADSCs, MSCs) [23, 24]. These ADSCs can undergo multilinear differentiation. These characteristics allow the evolution of a microenvironment favourable for the grafts commitment and the locoregional trophic enhancement. The residual substance loss resulted to be superficial and limited to the footbed region, was therefore subsequently treated with a small local rotation flap, supplemented with daily innovative dressings such as polyethyleneglycol ointment and advanced wound healing techniques such as cold atmospheric plasma applications [25]. The spontaneous calcaneal fractures in patients suffering from diabetic polyneuropathy are seen rarely and are often classified as not curable and therefore in the large part end with amputation. Rates of morbidity and mortality are both highly influenced by factors including the extent of the ulcer, the severity of the inflammatory process, as well as the number of comorbidities.
Nowadays we can make additive usage of non-invasive surgical and radiologic techniques, alongside technical devices like the NPWTi-d, allowing a conservative approach even in major lesions, guaranteeing subsequently the possibility of a slow and stepwise course of recovery based on reconstructive and regenerative surgical procedures, beyond the methods of advanced wound care.
Conclusion
Currently, spontaneous calcaneal fractures represent a complex therapeutic challenge, without scientific evidence indicating the favourable outcome of one type of approach. The key to success in the process of recovery, especially regarding the reacquisition of independent walking, should not be based on the individual decisions of a singular surgeon but instead involves the expertise and utilization of all available techniques within a wound care team.
Author Contributions
A.T. : acquisition of data and writer, clinical management of the case ; L. DP. : supervision of the paper, formal analysis ; M.T. : CWOCN nurse, clinical management of the case ; M.DM. : surgeon, conceptualization, planning and supervision of the paper, corresponding Author. All authors have read and agreed to the published version of the manuscript.
Funding
None.
Institutional Review Board Statement
Not applicable.
Informed Consent
Written informed consent has been obtained from the patient to publish this paper.
Conflicts of Interest
None.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 01, Aug 2022Accepted: Tue 16, Aug 2022
Published: Wed 07, Sep 2022
Copyright
© 2023 Marco De Monti. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2022.02.03
Author Info
Alessandro Torre Laura De Pellegrin Marta Teglas Marco De Monti
Corresponding Author
Marco De MontiEOC - Beata Vergine Regional Hospital, Department of Surgery, Mendrisio, Switzerland
Figures & Tables




References
1.
Hedlund LJ, Maki DD, Griffiths HJ (1998) Calcaneal
fractures in diabetic patients. J Diabetes Complications 12: 81-87. [Crossref]
2.
Mitchell MJ, McKinley JC, Robinson CM (2009) The
epidemiology of calcaneal fractures. Foot (Edinb) 19: 197-200. [Crossref]
3.
Chantelau E, Richter A, Ghassem Zadeh N, Poll LW
(2007) "Silent" bone stress injuries in the feet of diabetic patients
with polyneuropathy: a report on 12 cases. Arch Orthop Trauma Surg 127:
171-177. [Crossref]
4.
Fukuda T, Reddy V, Ptaszek AJ (2010) The infected
calcaneus. Foot Ankle Clin 15: 477-486. [Crossref]
5.
Essex Lopresti P (1993) The mechanism, reduction
technique, and results in fractures of the os calcis, 1951-52. Clin Orthop
Relat Res 290: 3-16. [Crossref]
6.
Clare MP, SRFa, dislocations of the calcaneus. In
Bucholz RW HJ, Court-Brown C, Tornetta P eRagsfiate, Philadelphia: Lippincott
Williams & Wilkins.
7.
Vestergaard P (2007) Discrepancies in bone mineral
density and fracture risk in patients with type 1 and type 2 diabetes--a
meta-analysis. Osteoporos Int 18: 427-444. [Crossref]
8.
Işıklar ZU, Bilen FE (2006) Kalkaneus kırıkları. TOTBÝD
(Türk Ortopedive Travmatoloji Birliği Derneği) Dergisi 5: 1-2.
9.
Kathol MH, el Khoury GY, Moore TE, Marsh JL (1991)
Calcaneal insufficiency avulsion fractures in patients with diabetes mellitus. Radiology
180: 725-729. [Crossref]
10. Compression Therapy in Diabetic Foot Ulcer Management: A Review of
Clinical Effectiveness, Cost-effectiveness and Guidelines. 2014. [Crossref]
11. Grayson ML, Gibbons GW, Balogh K, Levin E, Karchmer AW (1995) Probing to
bone in infected pedal ulcers. A clinical sign of underlying osteomyelitis in
diabetic patients. JAMA 273: 721-723. [Crossref]
12. Khatri G, Wagner DK, Sohnle PG (2001) Effect of bone biopsy in guiding
antimicrobial therapy for osteomyelitis complicating open wounds. Am J Med
Sci 321: 367-371. [Crossref]
13. Morrison WB, Ledermann HP (2002) Work-up of the diabetic foot. Radiol
Clin North Am 40: 1171-1192. [Crossref]
14. Sanders R, Fortin P, DiPasquale T, Walling A (1993) Operative treatment
in 120 displaced intraarticular calcaneal fractures. Results using a prognostic
computed tomography scan classification. Clin Orthop Relat Res 290:
87-95. [Crossref]
15. Radnay CS, Clare MP, Sanders RW (2010) Subtalar fusion after displaced
intra-articular calcaneal fractures: does initial operative treatment matter?
Surgical technique. J Bone Joint Surg Am 1: 32-43. [Crossref]
16. Cestaro G, Fasolini F, Regusci L, Torre A, De Monti M (2019) NPWTi-d in
the treatment of infected diabetic foot. G Chir 40: 445-449. [Crossref]
17. Cestaro G, Torre A, Fasolini F, De Monti M. Trick or Treat in plastic
reconstructive surgery with Dermal Regeneration Template A Retrospective Study
on Technique Refinement for a better outcome of reconstructive surgery with
Dermal Regeneration Template. XXIV Annual Meeting of the European Society of
Surgery.
18. Torre A, Fasolini F, De Monti M. Technical Refinements for quicker and
more effective integration of Dermal Regeneration Template in full thickness
skin defects. 55th Congress of Swiss Plastic Surgery (SGPRAC-SSCPRE).
19. De Monti M, Cestaro G, Bertani A, Torre A, Fasolini F (2020) Disposable
Negative Pressure Wound Therapy for Outpatient Management of Wounds: Outcomes
comparison Between Electrically- Powered and Mechanially- Powered Devices. Minerva
Biotecnol 32: 6-1.
20. Tabit CJ, Slack GC, Fan K, Wan DC, Bradley JP (2012) Fat grafting versus
adipose-derived stem cell therapy: distinguishing indications, techniques, and
outcomes. Aesthetic Plast Surg 36: 704-713. [Crossref]
21. Bourin P, Bunnell BA, Casteilla L, Dominici M, Katz AJ et al. (2013)
Stromal cells from the adipose tissue-derived stromal vascular fraction and
culture expanded adipose tissue-derived stromal/stem cells: a joint statement
of the International Federation for Adipose Therapeutics and Science (IFATS)
and the International Society for Cellular Therapy (ISCT). Cytotherapy
15: 641-648. [Crossref]
22. Tocco I, Widgerow AD, Lalezari S, Banyard D, Shaterian A et al. (2014)
Lipotransfer: the potential from bench to bedside. Ann Plast Surg 72:
599-609. [Crossref]
23. Bellini E, Grieco MP, Raposio E (2017) The science behind autologous fat
grafting. Ann Med Surg (Lond) 24: 65-73. [Crossref]
24. Baer PC (2020) Adipose-Derived Stromal/Stem Cells. Cells 9: 1997. [Crossref]
27. Stratmann B, Costea TC, Nolte C, Hiller J, Schmidt J et al. (2020) Effect of Cold Atmospheric Plasma Therapy vs Standard Therapy Placebo on Wound Healing in Patients With Diabetic Foot Ulcers: A Randomized Clinical Trial. JAMA Netw Open 3: e2010411. [Crossref]
