Reversed Bowel Rotation with Midgut Volvulus and Internal Hernia
A B S T R A C T
Congenital intestinal malrotation is a group of intestinal rotational anomalies occurring during embryogenesis. Reversed rotation is considered the rarest type of malrotation and often presents with symptoms of bowel obstruction. We present a rare case of a 27-year-old woman who presented with acute abdomen. The patient’s preoperative computed tomography (CT) scan and operative findings confirmed reverse malrotation, internal hernia of foramen of Winslow, and midgut volvulus. The transverse colon, duodenum, small bowel, cecum, and appendix were abnormally located, with the presence of Ladd bands. The patient underwent an emergency laparotomy (Ladd procedure) with an uneventful postoperative recovery and an unremarkable follow-up CT scan of the abdomen. A review of the literature for intestinal reverse malrotation is also presented to provide an understanding of the expected clinical picture and imaging findings for this rare anomaly.
Keywords
Reversed bowel rotation, midgut volvulus, foramen of Winslow internal hernia, first reported case
Introduction
Midgut malrotation is a congenital anomaly that occurs during embryonic development. The fetal intestine is rotated as a result of a deviation of normal rotation of the embryonic gut. Intestinal malrotation occurs in between 1 in 200 and 1 in 500 live births [1]. Most patients with malrotation are found to be asymptomatic, with symptomatic malrotation occurring in only 1 in 6000 live births [2]. Adult midgut malrotation is rare, with an incidence between 0.0001% and 0.19% [1]. It is reported that more than 90% of patients present by the time of their first birthday [1]. Malrotation anomalies can be subdivided into five major variants: non-rotation, mixed rotation, isolated duodenal malrotation, hyper rotation, and reversed rotation [2]. The most common variant is non-rotation [3]. Reversed rotation is considered the rarest [4]. To our knowledge, we present the first reported case of reversed rotation with associated midgut volvulus and foramen of Winslow internal hernia in an adult patient.
The majority of adult malrotation anomalies are discovered either on imaging investigations for unrelated conditions or incidentally during surgery. Adults who are affected may, however, present with symptoms of intestinal obstruction or intermittent and recurrent abdominal pain of acute or chronic onset. Despite the clear clinical presentation of intestinal obstruction and concordant radiographic findings, reaching the true diagnosis in this age group with the added complications can prove difficult and requires further radiologic investigation by computed tomography (CT). Furthermore, most surgeons have a low index of suspicion toward this diagnosis and may not consider the diagnostic possibility in the initial evaluation of adult patients presenting with abdominal pain.
Case Report
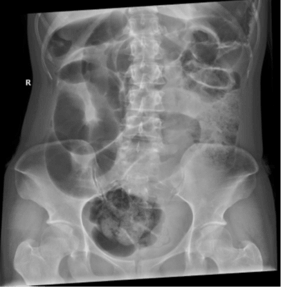
A 27-year-old Woman presented to the emergency department (ED) complaining of epigastnc pain, repeated vomiting, distention, and obstipation of a 1-day duration. The pain was colicky in nature, progressive, acute in onset, and non-radiating. The patient had not experienced similar symptoms and had no previous medical or surgical history. On examination, she was vitally stable. The abdomen was severely distended with significant tenderness in the central epigastric and right hypochondriac regions. On auscultation, the bowel sounds were sluggish. Routine blood work and investigations were ordered, and results demonstrated leucocytosis of 22109 and platelets of 239 109. Radiographs of the abdomen performed in the ED showed markedly distended small bowel loops with multiple air-fluid levels and no free air under the diaphragm. ( Figures 1A & 1B).
Figure 1 A & B: Erect and supine radiographs show small bowel dilatation and multiple air fluid level.
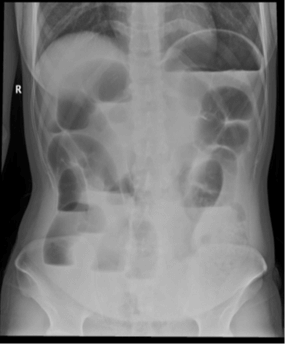
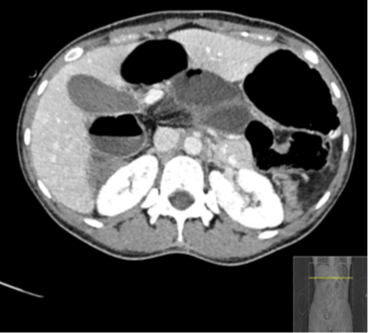
Figure 2: Enhanced CT of the abdomen, Shows abnormal position of the transverse colon posterior to the mesenteric vessels and anterior to IVC and aorta.
A nasogastric tube and Foley catheter were inserted. The patient was ordered to have no food and was put on intravenous fluids (50% dextrose solution and normal saline at 150 mL/hr). Considering the vital stability of the patient a CT study of the abdomen was then performed using Siemens SOMATOM Perspective CT scanner using the I30s Kernel with 1.5-mm and 5.0-mm slice thickness reconstructions. The images were acquired in the Porto venous phase, after the injection of 90 mL of Omnipaque 350 mg/mL contrast agent. The study showed the following: dilated small bowel loops with maximum diameter of 3.7 cm with features of reversed rotation, midgut volvulus, and an obstructed foramen of Winslow hernia. A minimal amount of intraperitoneal free fluid was noted.
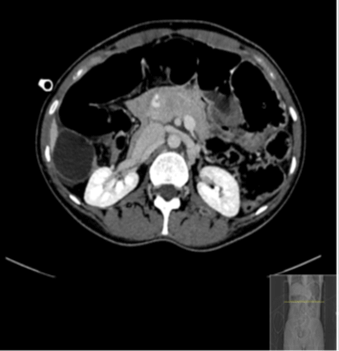
Figure 3: Enhanced CT of the abdomen at the level of the midgut shown is “whirl sign” with a worrisome finding of a centrally attenuated vessel.
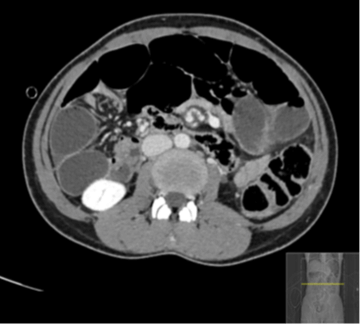
Figure 4: Enhanced CT of the abdomen at the level of the junction between the lesser and greater sac, shows dilated duodenal loops, converging and congested mesentery with tapering of the bowel loops, and “beak sign” at the foramen of Winslow.
The dilated duodenal loops with converging, twisting, and congested mesentery at the level of the upper right abdomen are findings consistent with the appearance and location suggestive of an obstructed foramen of Winston internal hernia (Figure 4). Twisting/swirling (“whirl sign”) of the mesentery and bowel at the level of midgut with centrally attenuated vessel, adjacent collapsed loops (Figure 3), multiple local lymph nodes, and congested mesentery are compatible with midgut volvulus [1]. A transverse colon that is collapsed and lies anterior to the abdominal aorta and inferior vena cava (IVC) and posterior to the superior mesenteric vessels with reversed relation of superior mesenteric vessels is an extraordinary finding suggestive of reversed rotation type of congenital malrotation [4] (Figure 2).
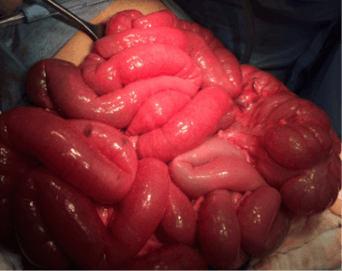
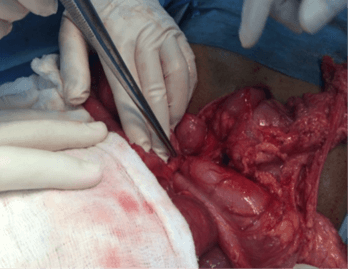
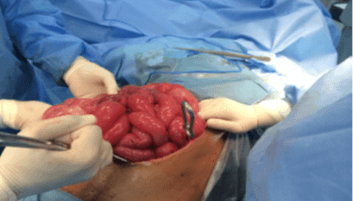
The patient immediately underwent an open laparotomy that supported the radiologic findings. On OR, the bowel was viable but markedly congested (Figures 5A & 5B). The bowel was twisted along their mesenteric axis about 720 degrees clockwise with adhesion ladd bands (Figure 5C). The cecum and transverse colon were appreciated in an abnormal location to the left-side and anteriorly, respectively. A lesser sac internal hernia was also identified containing twisted duodenum and proximal jejunal loops. Adhesiolysis, counterclockwise detorsion, reduction of the foramen of Winslow internal hernia were performed without colopexy (Figure 5D). No complications during or immediately after the OR.
Figure 5: Laparotomy showing, A & B) viable congested dilated small bowel and midgut volvulus with Ladd bands and C) left side location of the caecum; D) Appearance after reversal of the bowel to the normal position.
Postoperatively, the patient was kept without food for 48 hours and on I.V fluids and she had a bowel movement on the third day. Aside from pain, which was controlled by medication, the patient remained vitally stable with no fever or other new onset symptoms.
The patient recovered from surgery and was doing well. She was discharged home on postoperative day 9. A follow-up radiograph taken 3 months later showed a non-specific bowel gas distribution with no significant dilatation or air-fluid levels (Figure 6), The patient is doing well to date; she conceived and had an uneventful spontaneous vaginal delivery of a healthy baby.
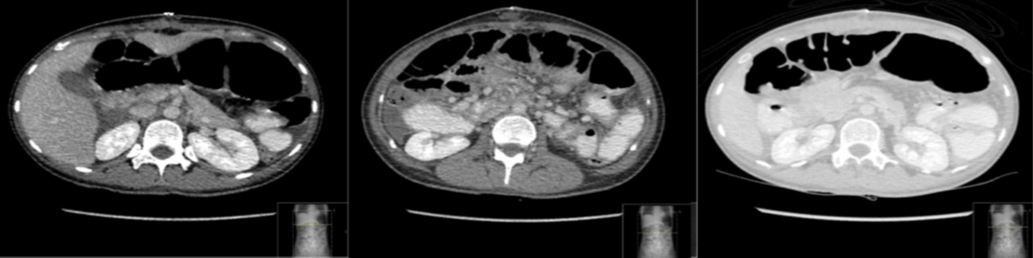
Figure 6: Multiple follow-up enhanced CT cuts of abdomen showing A) reduction of foramen of Winslow hernia, B) detrosed midgut, and C) anterior position of the transverse colon.
Discussion
The midgut is typically noted outside the coelomic cavity and protrudes through the umbilical ring at approximately week 4 of fetal development. By week 10 of gestation, the midgut rotates in a counterclockwise rotation around the axis of the superior mesenteric artery (SMA) for 270 degree to migrate into the abdominal cavity. The first to return is the duodenojejunal segment to fix to the upper left quadrant at the ligament of Treitz. The cecocolic segment also rotates counterclockwise around the SMA to rest in its final position in the right lower quadrant. By week 12, intestinal rotation is complete, and the colon becomes fixed to the retro peritoneum [1, 5, 6]. Any deviation, interruption, or reversal of any of the phases of rotation results in a range of intestinal malrotation anomalies.
Reversed rotation is one of the congenital intestinal malrotation anomalies and is considered to be the rarest [4]. Robert et at. have discussed and reviewed only 27 previously reported cases of reversed rotation [7]. It is a result of a 90-degree clockwise rotation of the midgut rather than the normal 270-degree counterclockwise rotation [8]. The duodenum is located anterior to the SMA. The transverse colon may be pre-arterial or may be rotated clockwise or counterclockwise in a retro-arterial position. In either case, the cecum may be right-sided or left-sided. The most common anomaly is a retro-arterial clockwise rotation in which the transverse colon is seen posterior to the SMA and anterior to the aorta. Also, the presence of congenital bands, known as Ladd bands, extending across the duodenum and attaching to the cecum, can compress the small bowel and cause obstruction [1, 6, 8]. The abnormal location of the bowel can result in a narrow superior mesenteric vascular pedicle and predisposes the patient to subsequent midgut volvulus and obstruction with possible vascular compromise [8].
Midgut malrotation in adults may be asymptomatic or have non-specific symptoms that are incidentally discovered during investigations or laparotomy for other unrelated problems [1]. Presentation of malrotation can vary clinically, according to the mechanism of obstruction and whether it is complicated by a compromised bowel. The symptoms are related to the presence of associated complications such as midgut volvulus, internal hernia, and duodenal obstruction. The acute presentation is characterized by sudden acute colicky abdominal pain and distention, repeated vomiting, nausea, and obstipation, which may progress rapidly over hours. The chronic presentation, which is more common, is characterized by intermittent colicky abdominal pain, vomiting, nausea, and bloating over several months. The different clinical presentations of such patients need a high index of suspicion for midgut malrotation when investigating the cause of intermittent abdominal symptoms in adults [8]. Dietz et al. studied a series of 10 adults with bowel obstruction resulting from intestinal malrotation [5]. Fu et al. reported that 6 of 12 patients in their series presented with chronic intermittent abdominal symptoms [8].
Adults typically present with symptoms of acute bowel obstruction and possible signs and symptoms of bowel ischemia. Moldrem et al. reported that 48.5% of their 33 patients presented with an acute abdomen [9]. Patients can also have atypical presentations that might mimic other diseases, leading to an incorrect diagnosis such as acute appendicitis, cholecystitis, pancreatitis, perforated peptic ulcer disease, and colonic diverticulitis. Several authors have reported observing atypical presentations of this nature before discovering gut malrotation with abnormal location of the cecum and appendix at surgery [5, 8].
Surgical intervention is required for symptomatic patients with midgut malrotation. Surgical Intervention for asymptomatic patients is still a topic of debate. Choi et al. reviewed 177 patients over a 35-year period and found that asymptomatic patients had a low risk of intestinal volvulus and advised that routine investigations, screening, and elective surgery were not necessary with close follow-up [10]. However, some surgeons recommend intervention for all patients with intestinal malrotation, as it is impossible to predict whether and when complications may develop. Surgical intervention should be based on clinical presentation and radiologic diagnosis while weighing risk factors and co-morbidities.
The Ladd procedure continues to be the surgical treatment of choice for malrotation. Before William Ladd's publication in 1936, surgical treatment for malrotation with or without volvulus had a mortality rate higher than 90% [6]. The classic Ladd procedure consists of four parts: widening of the narrowed root of the small bowel mesentery by mobilizing the duodenum, and division of the adhesions around the SMA to prevent further volvulus; counterclockwise detorsion of the midgut volvulus if present and appendectomy to avoid a future diagnostic dilemma of atypical appendicitis [6]. Fu et a1. Reported a complete resolution of symptoms in nine patients and a near complete resolution in two of eleven patients [8]. Dietz et al. also reported a complete symptomatic resolution in eight of their ten patients treated surgically [5]. Additional techniques used to prevent recurrent volvulus include re-establishments of the normal gut anatomy by duodenopexy, caecopexy, and suture fixation of the ascending colon; the necessity of these techniques is debatable, and they were not performed in our patient [1, 5].
Conclusion
Understanding the normal and abnormal patterns of embryonal midgut rotation is critical in diagnosing and managing intestinal malrotations. Reversed intestinal rotation has been reported and revered in the literature as the rarest of the congenital midgut malrotation anomalies. This anomaly predisposes the patient to an increased risk of developing and presenting with bowel obstruction as a result of obstructed internal hernias or/and volvulus. Appropriate radiologic diagnosis, prompt surgical intervention, and follow-up can improve the patient survivability and surgical outcome.
Funding
None.
Consent
The patient has consented for publication of this case report and provided images.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Fri 24, Jan 2020Accepted: Wed 19, Feb 2020
Published: Sat 29, Feb 2020
Copyright
© 2023 Mona Mogahed. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2020.01.07
Author Info
Atif Mahmoud Mahdi Hasn Hifni Hassan Juma Mona Mogahed Mona Saleh Allaf
Corresponding Author
Mona MogahedAssistant Professor of Anesthesiology, Surgical ICU and Pain Medicine, Faculty of Medicine Tanta University, Egypt
Figures & Tables

References
- Wang CA, Welch CE (1963) Anomalies of Intestinal Rotation in Adolescents and Adults. Surgery 54: 839-855. [Crossref]
- Kapfer SA, Rappold JF (2004) Intestinal malrotation-not just the pediatric surgeon's problem. J Am Coll Surg 199: 628-635.
- Schey WL, Donaldson JS, Sty JR (1993) Malrotation of bowel: variable patterns with different surgical considerations. J Pediatr Surg 28: 96-101. [Crossref]
- GR Giles (l966) Reversed intestinal rotation. Postgrad Med J 42: 782-784. [Crossref]
- Diem DW, Walsh RM, Grundfest Broniatowski S, Lavery IC, Fazio VW et al. (2002) Intestinal malrotation: a rare but important cause of bowel obstruction in adults. Dis Colon Rectum 45: 1381-1386. [Crossref]
- Ladd WE (1936) Surgical diseases of the alimentary tract in infants. N Engl I Med 215: 705-708.
- Warthen RO, Lattman I, White CS (1952) Reversed rotation of the bowel, review of the literature and report of an unusual case. AMA Am J Dis Child 83: 487-492. [Crossref]
- Fu T, Tong WD, He YJ, Wen YY, Luo DL et al. (2007) Surgical management of intestinal malrotation in adults. World J Surg 31: 1797-1803. [Crossref]
- Moldrem AW, Papaconstantinou H, Broker H, Megison S, Jeyarajah DR (2008) Late presentation of intestinal malrotation: an argument for elective repair. World J Surg 32: 1426-1431. [Crossref]
- Choi M, Borenstein S, Homberger L, Langer J (2005) Heterotaxia syndrome. The role of screening for intestinal rotation abnormalities. Arch Dis Child 90: 81 3-815. [Crossref]
