Resection of Adrenocortical Carcinoma with Bilobar Liver Metastasis Following Neoadjuvant Therapy Using a Modified Mini-ALPPS Approach: A Case Report
A B S T R A C T
Introduction: Adrenocortical carcinoma (ACC) is an aggressive tumor with high proportion of patients presenting with metastatic disease, most commonly in the liver. Prognosis in this population is extremely poor. Resection of the primary tumor and liver metastasis offers a survival benefit in well-selected patients. However, the extent of surgery is often significant and can limit the ability to accomplish a safe margin-negative resection.
Presentation of case: A 35-year-old male presented with a large left ACC (15.2cm) and multiple bilobar liver metastases (1.5-12.5cm). He was treated with mitotane and chemotherapy / immunotherapy, with excellent response. Multidisciplinary discussion led to recommendations for a curative-intent approach with surgery. A staged approach was performed for the resection, using a modified Mini-ALPPS technique. A complete margin-negative resection of all disease was accomplished. The patient recovered well and remains free of disease 24-months following diagnosis.
Discussion: This case highlights novel components of treatment for metastatic ACC and for hepatectomy for bilobar liver metastasis. The decisions to proceed to surgery for complete resection and to use a staged approach with a modified Mini-ALPPS technique were both critical components to render the patient disease-free. Appropriate expertise and multidisciplinary teamwork are essential for implementation of these approaches.
Conclusion: Neoadjuvant chemotherapy for stage IV ACC can result in disease control and improved selection of candidates for curative-intent surgery. In the setting of bilobar liver disease and a large primary in place, a modified Mini-ALPPS approach provides a safe and feasible way to accomplish complete resection and improved survival.
Keywords
Adrenocortical carcinoma, mitotane, neoadjuvant chemotherapy, liver metastasis, mini-alpps, staged hepatectomy, case report
Introduction
Adrenocortical carcinoma is a rare and aggressive tumor with poor prognosis in part due to the advanced stage at diagnosis; patients typically present with large primary tumors (median size 13cm) involving surrounding organs and/or have associated metastatic disease [1]. Metastasis most commonly occur in the lymph nodes and liver and treatment is with systemic chemotherapy including cytotoxic agents (etoposide, doxorubicin, cisplatin - EDP) and/or mitotane [2]. Despite improvements in systemic treatment, median overall survival remains low (9 months) with the only potential for cure in well-selected patients in whom complete resection can be accomplished [1].
For patients presenting with synchronous ACC and liver metastasis, resection can be limited by the ability to remove all disease; the primary tumor is typically large and requires multi-visceral resection, and the liver metastases are commonly multifocal with a bilobar distribution [3]. Further, the remaining liver following surgery (future liver remnant - FLR) is typically small, increasing the risk of post-hepatectomy liver failure and death [4]. Staged hepatectomy has evolved as the standard of care for patients with bilobar liver metastasis and a small FLR; a first-stage resection is performed removing tumor/s from one side of the liver (typically those in the FLR), followed by postoperative portal vein embolization, to induce liver hypertrophy of the FLR [4, 5]. Subsequently, a second-stage major hepatectomy is performed (4-6 weeks later), of the contralateral lobe to accomplish complete resection. More recently, an alternative to this approach was introduced: Associating Liver Partition and Portal Vein Ligation for Staged hepatectomy (ALPPS) [6].
This approach includes adding portal vein ligation and splitting the liver through the desired future resection plane, to the first stage, and completion major hepatectomy during the second stage. The described benefits of this approach include faster and potentially a more significant liver hypertrophy, which allows for a shorter time to second-stage (usually within 7-14 days), and has translated into higher rates of second-stage completion (faster and more significant hypertrophy and lower rates of disease progression), although at the expense of higher postoperative morbidity and mortality [6].
We present a case of a patient with large ACC and synchronous bilobar liver metastasis, having complete resection following response to immunotherapy, and using a modified Mini-ALPPS approach for primary tumor resection and extended hepatectomy, that provides a safer and equally effective strategy. The case is reported in compliance with the SCARE guidelines [7].
Presentation of Case
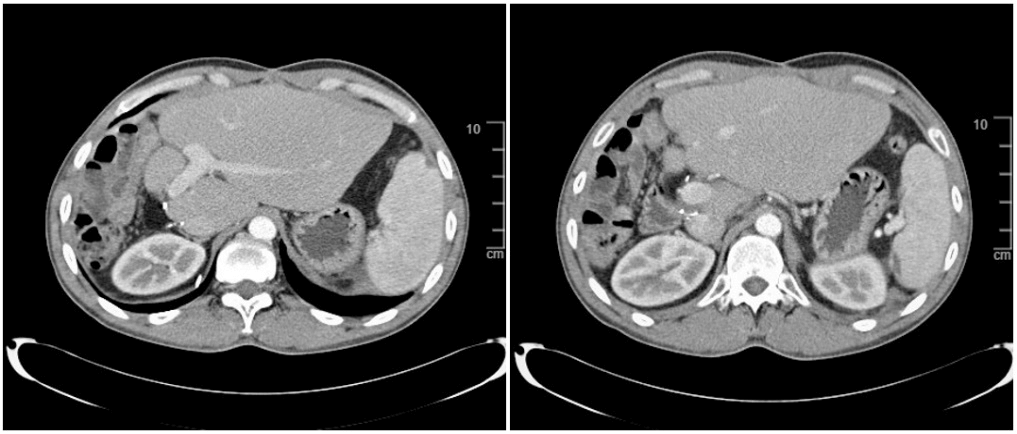
A 35-year-old man was referred to our institution for work-up of a left adrenal mass and liver lesions found during work-up for acute onset of right abdominal pain. The patient denied clinical symptoms of Cushing’s Disease, hyperaldosteronism, pheochromcytoma or hyperandrogenism. Notably the patient had a strong history of alcohol use and possible cirrhosis. Physical exam was within normal limits. Laboratory work-up revealed a normal blood count, chemistry and liver function tests. Endocrine work-up revealed elevated ACTH (115pg/ml [ normal range 7-69]), androstenedione 803 ng/mL (normal range 40-190), and dehydroepiandrosterone sulfate (588 ug/dl [normal range 120-520]). A contrast-enhanced multiphasic thoracoabdominal CT revealed a large 15cm left adrenal mass with diaphragmatic, stomach and spleen involvement and 6 liver metastases involving the right lobe and segment 4 of the left liver (ranging 1.8cm - 12cm) (Figure 1A & 1B). Liver biopsy confirmed adenocarcinoma with immunohistochemistry profile consistent with metastatic ACC (Negative: Glypican-3, Arginase, hep-par-1, CK7, CK20, RCC, CD31, CEA, CD10, PAX-8 and Positive: CAM5.2, Mart-1 and Inhibin).
Figure 1: Pre-treatment (A-B) and post-chemotherapy (C-D) computed tomography (CT), illustrating significant response to therapy with decrease in size of the liver lesions (largest from 12cm to 6.8cm) and the primary tumor (from 15cm to 11cm). Note the primary tumor is in close proximity to the stomach, spleen and left diaphragm and the liver lesions have a bilobar distribution sparing only segments 2 and 3.
With diagnosis of stage IV ACC (T3-4N0M1) treatment with mitotane and EDP-based regimen was initiated. The patient received 6 cycles with mixed response, leading to the decision of switching to nivolumab and mitotane (5 cycles), with excellent response characterized by decreased size of the primary tumor and the liver metastases (Figures 1 A- 1D). The patient’s case was discussed in the multidisciplinary tumor board with a recommendation to proceed with a curative-intent resection of both the primary tumor and the liver metastases. A thorough assessment of the tumor extension and the operation required was performed by the hepatobiliary and sarcoma/adrenal surgical teams. This included 3D-liver volumetric measurement of the FLR (segments 1-3) which was found to be 28% (Figure 2A). The operation was planned using a two-stage approach with a modified Mini-ALPPS technique; in short, the patient had a preoperative percutaneous portal vein embolization of the right portal vein and segment 4 branches [day 0] (Figure 2B), followed by a first-stage operation: radical left adrenalectomy with en-bloc left diaphragmatic resection (sarcoma surgical team - RG) and a liver partition (linear hepatotomy) along the left lateral fissure (hepatobiliary surgical team - DAA) [day 1] (Figure 3A).
Figure 2: Imaging and 3D-liver volumetric analysis before and after portal vein embolization (PVE).
2A) 3D-liver volumetry (CT) pre-PVE;2B) Fluoroscopic image after completion of PVE of the right portal branches (horizontal arrow) and left segment 4A and 4B portal branches (vertical arrow); 2C) CT scan after first-stage procedure, depicting the hepatotomy plane along the left lateral fissure and deep to the area of the segment 4 PVE coils; 2D) 3D-liver volumetry (CT) 10 days after PVE, illustrating the growth in the FLR.
Figure 3: Intraoperative photographs.
3A) First-stage operation , illustrating the linear hepatotomy and antiadhesive barrier placement. Note the right liver is avoided and the area of future resection left with virgin planes for the second-stage procedure; 3B) Findings upon opening the abdomen during the second-stage. Note the hypertrophied left lateral section and the hepatotomy line previously created, guiding the line of transection; 3C-3D) Operative specimen (right trisectionectomy) after complete resection.
The patient recovered well and was discharged on postoperative day 4 [day 5]. During the postoperative visit a new CT with 3D-liver volumetry was performed which confirmed the adequate hepatotomy plane (Figure 2C) and revealed a FLR hypertrophy to 42% (degree of hypertrophy =14%; relative hypertrophy = 51%; kinetic growth rate = 11%/week) (Figure 2D) [day 10]. The second-stage operation was performed: extended right hepatectomy [day 15] (Figures 3B- 3D). The patient recovered well and was discharged on postoperative day 4 [day 19]. Pathology confirmed diagnosis of ACC, low grade, with margin-negative resection (pT3N0M1) of both the primary and liver metastasis. The patient is now 24 months after initial diagnosis and image reveals no evidence of disease (Figure 4).
Figure 4: Surveillance CT scan, 6 months following complete resection of the tumors. Note significant hypertrophy of the left lateral liver and no evidence of disease in the liver nor the left adrenal resection bed.
Discussion
Adrenocortical carcinoma is an extremely aggressive tumor when presenting with metastatic disease, with 5-year overall survival (OS) <10% [1]. The novelty of the case presented herein includes the critical role of systemic therapy and the use of a modified Mini-ALPPS approach, which played a key role in accomplishing adequate hypertrophy and ultimately leading to resection in a safe and expeditious manner.
A number of studies have reported improved survival following surgical treatment of metastatic ACC. [8, 9] Although some have reported no prognostic significance of preoperative treatment, we feel that systemic chemotherapy is the first-line of treatment, and that response to therapy helps select patients with a more favorable biology and who may benefit from complete resection [9]. One trial demonstrated survival benefit for patients with borderline resectable tumors; 15 patients received preoperative chemotherapy and 13 (86%) underwent surgical resection and experienced a trend towards improved median disease-free survival (28.0 months vs. 13 months; p=ns) when compared to the surgery alone group [10]. Further, although studies evaluating the benefit of immunotherapy for ACC have been somewhat disappointing, some have reported modest responses in patients with metastatic ACC [11, 12]. Preoperative chemotherapy and possibly the addition of nivolumab in this patient’s treatment were pivotal to induce response to therapy, resulting in the potential for resection.
Although liver resection is rarely possible, the benefit of hepatectomy for patients with ACC and liver metastasis has been well documented [3, 13]. Results from a study using the German ACC registry found that median overall survival (OS) was significantly higher for patients having resection as compared to those not resected (76.1 months versus 10.1 months; p<0.001). Despite inherent selection bias, others have published similar results for the same population [13]. Importantly, margin-positive (R1-2) resections are common, ranging from 30-40%. In this case, complete resection was facilitated by inducing hypertrophy of the FLR which allowed transection away from the tumors while still preserving enough liver parenchyma. By using a Mini-ALPPS approach, in which only a linear hepatotomy rather than a complete liver partition is performed, the safety of the procedure is enhanced, and the risk of postoperative complications significantly reduced [14].
Further, our modified technique starts with preoperative percutaneous portal vein embolization, replacing portal ligation and hilar dissection during the first stage, and as such further increasing the safety of the procedure, as well as efficacy; multiple studies have shown better hypertrophy with embolization over portal vein ligation approaches [15]. Notably, our modified Mini-ALPPS approach was considered with the specific goal to induce faster/higher hypertrophy and to reduce the period of time with active disease and without systemic therapy (completed resection and discharged home in 19 days). Lastly, although our modified Mini-ALPPS approach was not used for staged hepatectomy, it allowed us to stage two large and complex operations while inducing the necessary hypertrophy at the same time. This represents an important concept of the ALPPS technique when staged resections of primary and metastatic tumors may be more appropriate than combined procedures. Critical to this approach, however, is the context within high-volume centers where not only the surgical expertise is available, but also the multidisciplinary approach for medical treatment of cancer and perioperative care, both being optimized through systematic standardized protocols that can still allow for individualized approaches, as needed.
Conclusions
Despite poor prognosis in patients with ACC and liver metastasis, treatment with novel systemic agents including EDB-based regimens, mitotane and immunotherapy can result in meaningful responses and help select patients with a more favorable biology who may benefit from complete resection. The extent of surgery is often significant and further limited by small future liver remnant after hepatectomy. The modified Mini-ALPPS approach, described in this manuscript, is a reasonable alternative that provides a way to stage two complex resections, induce fast and significant liver hypertrophy, reduce risk of complications and ultimately result in an overall safer and efficient approach for complete curative-intent resection of aggressive malignancies.
Conflicts of Interest
None.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Acknowledgements
The authors would like to thank Diana Castillo for assistance in manuscript preparation and formatting.
Funding
None.
Highlights
• Well-selected patients with ACC liver metastasis can benefit from surgery.
• Chemotherapy prior to surgery contributes to improved patient selection.
• Bilobar liver metastasis can be resected using staged approaches.
• ALPPS is a feasible surgical approach to initially unresectable liver tumors.
• Modified Mini-ALPPS is safe and effective for bilobar liver metastasis.
Article Info
Article Type
Case ReportPublication history
Received: Mon 24, Feb 2020Accepted: Mon 16, Mar 2020
Published: Mon 23, Mar 2020
Copyright
© 2023 Daniel Anaya. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2020.01.06
Author Info
Bela Kis Daniel Anaya Jasmina Ehab Julie E. Hallanger Johnson Pilar Suz Ricardo Gonzalez
Corresponding Author
Daniel AnayaSection of Hepatobiliary Tumors, Department of Gastrointestinal Oncology, H. Lee Moffitt Cancer Center & Research Institute, Tampa, Florida, USA
Figures & Tables


2A) 3D-liver volumetry (CT) pre-PVE;2B) Fluoroscopic image after completion of PVE of the right portal branches (horizontal arrow) and left segment 4A and 4B portal branches (vertical arrow); 2C) CT scan after first-stage procedure, depicting the hepatotomy plane along the left lateral fissure and deep to the area of the segment 4 PVE coils; 2D) 3D-liver volumetry (CT) 10 days after PVE, illustrating the growth in the FLR.
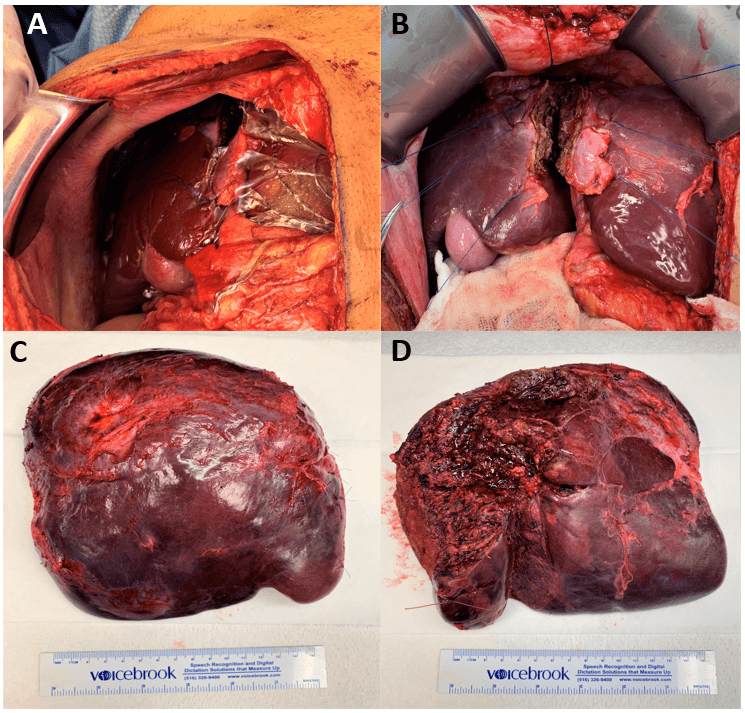
3A) First-stage operation , illustrating the linear hepatotomy and antiadhesive barrier placement. Note the right liver is avoided and the area of future resection left with virgin planes for the second-stage procedure; 3B) Findings upon opening the abdomen during the second-stage. Note the hypertrophied left lateral section and the hepatotomy line previously created, guiding the line of transection; 3C-3D) Operative specimen (right trisectionectomy) after complete resection.
References
- Bilimoria KY, Shen WT, Elaraj D, Bentrem DJ, Winchester DJ et al. (2008) Adrenocortical carcinoma in the United States: treatment utilization and prognostic factors. Cancer 113: 3130-3136. [Crossref]
- National Comprehensive Cancer Network. (2020) Neuroendocrine and Adrenal Tumors.
- Gaujoux S, Al Ahmadie H, Allen PJ, Gonen M, Shia J, D'Angelica M et al. (2012) Resection of adrenocortical carcinoma liver metastasis: is it justified? Ann Surg Oncol 19: 2643-2651. [Crossref]
- Orcutt ST, Kobayashi K, Sultenfuss M, Hailey BS, Sparks A et al. (2016) Portal Vein Embolization as an Oncosurgical Strategy Prior to Major Hepatic Resection: Anatomic, Surgical, and Technical Considerations. Front Surg 3: 14. [Crossref]
- Brouquet A, Abdalla EK, Kopetz S, Garrett CR, Overman MJ et al. (2011) High survival rate after two-stage resection of advanced colorectal liver metastases: response-based selection and complete resection define outcome. J Clin Oncol 29: 1083-1090. [Crossref]
- Narita M, Oussoultzoglou E, Ikai I, Bachellier P, Jaeck D (2012) Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 256: e7-e8. [Crossref]
- Agha RA, Borrelli MR, Farwana R, Koshy K, Fowler AJet al. (2018) The SCARE 2018 statement: Updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg 60: 132-136. [Crossref]
- Dy BM, Strajina V, Cayo AK, Richards ML, Farley DR et al. (2015) Surgical resection of synchronously metastatic adrenocortical cancer. Ann Surg Oncol 22: 146-151. [Crossref]
- Datrice NM, Langan RC, Ripley RT, Kemp CD, Steinberg SM et al. (2012) Operative management for recurrent and metastatic adrenocortical carcinoma. J Surg Oncol 105: 709-713. [Crossref]
- Bednarski BK, Habra MA, Phan A, Milton DR, Wood C et al. (2014) Borderline resectable adrenal cortical carcinoma: a potential role for preoperative chemotherapy. World J Surg 38: 1318-1327. [Crossref]
- Head L, Kiseljak Vassiliades K, Clark TJ, Somerset H, King J et al. (2019) Response to Immunotherapy in Combination With Mitotane in Patients With Metastatic Adrenocortical Cancer. J Endocr Soc 3: 2295-2304. [Crossref]
- Carneiro BA, Konda B, Costa RLB, Sagar V, Gursel DB et al. (2019) Nivolumab in Metastatic Adrenocortical Carcinoma: Results of a Phase 2 Trial. J Clin Endocrinol Metab 104: 6193-6200. [Crossref]
- Baur J, Buntemeyer TO, Megerle F, Deutschbein T, Spitzweg C et al. (2017) Outcome after resection of Adrenocortical Carcinoma liver metastases: a retrospective study. BMC cancer 17: 522. [Crossref]
- de Santibanes E, Alvarez FA, Ardiles V, Pekolj J, de Santibanes M (2016) Inverting the ALPPS paradigm by minimizing first stage impact: the Mini-ALPPS technique. Langenbecks Arch Surg 401: 557-563. [Crossref]
- Robles R, Marin C, Lopez Conesa A, Capel A, Perez Flores D et al. (2012) Comparative study of right portal vein ligation versus embolisation for induction of hypertrophy in two-stage hepatectomy for multiple bilateral colorectal liver metastases. Eur J Surg Oncol 38: 586-593. [Crossref]
