Repeated Middle Meningeal Artery Embolization for Chronic Subdural Hematoma Management: Case Report
A B S T R A C T
Aim: Middle Meningeal Artery (MMA) embolization has emerged as a viable neuroendovascular technique for the management of chronic subdural hematoma (SDH). Comparative analysis of various endovascular techniques for embolization is lacking. Guidance on operative techniques in situations of prior embolization failure is rare.
Materials and Methods: In this case report, we present a patient with a chronic subdural hematoma that failed previous coil embolization of the MMA. Digital Subtraction Angiography showed the previously placed coil and continued distal flow to the dural membranes.
Results: Onyx liquid embolization was completed successfully, effectively halting both anterograde flow to the MMA and retrograde flow from external circulation collaterals.
Conclusion: This case report suggests that in situations of MMA embolization failure, follow-up angiography may be completed to determine if further embolization through other procedural techniques may be possible. The angiographic images contained here highlight the advantages of liquid embolization over coil embolization of the MMA in halting SDH angiogenesis.
Keywords
Meningeal arteries, chronic subdural hematoma, therapeutic embolization
Introduction
Middle Meningeal Artery (MMA) Embolization is a relatively new neuroendovascular intervention technique for addressing subdural hematoma (SDH), a notably tenacious pathology. By 2030, an estimated 17.4 per 100,000 individuals will develop a chronic subdural hematoma, becoming the most common neurosurgical emergency [1]. While the exact pathogenesis of chronic SDH is thought to be a complex interplay of multiple factors, the benefit of MMA embolization is thought to be derived from occlusion of blood supply to the outer subdural membranes, which are made up of neovasculature arising from distal branches of the MMA [2-4]. Multiple studies have demonstrated safety and efficacy of the technique, and it has become an increasingly popular modality both as an adjuvant therapy or standalone treatment, particularly in populations with significant surgical risk or contraindications to open evacuation [5, 6]. However, as a newer treatment strategy, there is no consensus for when and to whom to offer MMA embolization, and even less guidance for specific procedural technique.
Coil embolization has long been a staple of the endovascular field. Studies investigating the efficacy of MMA embolization in chronic SDH resolution have primarily focused on polyvinyl particle or liquid embolization [7-9]. Liquid embolization has several theoretical advantages, including increased distal penetration and more thorough angiographic visualization [10]. Comparative analysis of the various endovascular techniques has yet to occur. Guidance on procedural techniques in cases of embolization failure is rare in the literature.
Here we present a unique patient with a chronic SDH previously treated unsuccessfully via burr holes and MMA coil embolization. Successful occlusion was accomplished through liquid Onyx embolization. Angiographic figures included here display the failed coil embolization and efficacy of the Onyx alternative.
Case Presentation
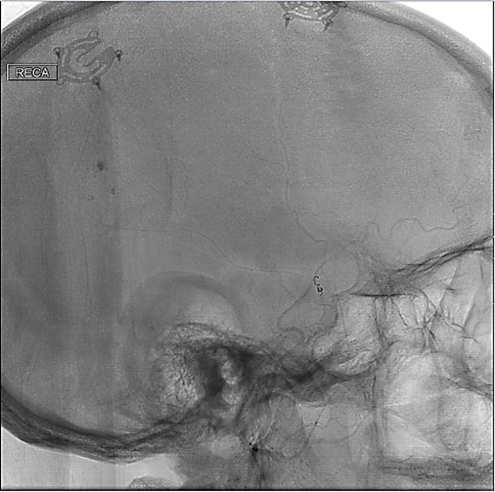
A patient in their 80’s with a history of coronary artery disease and previously treated SDH presented with progressive fatigue and mild confusion. The patient’s head CT demonstrated recurrent large right holohemispheric acute-on-chronic SDH (Figure 1). The patient had originally undergone right-sided burr hole placement one year prior, as well as coil embolization of the right MMA four months afterwards to address recurrence, both at another institution. Given the age, medical comorbidities, and prior unsuccessful surgical intervention, the patient was offered embolization of the MMA to prevent neovascularization and further right-sided subdural hematoma expansion.
Figure 1: Pre-Procedural Head CT: Large acute-on-chronic subdural hematoma after prior MMA coil embolization.
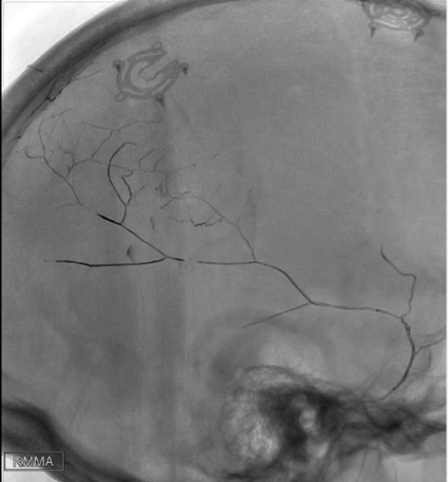
Figure 2: Digital Subtraction Angiography of the Right ECA: Distal flow past MMA coil as well as vascular filling of subdural membranes.
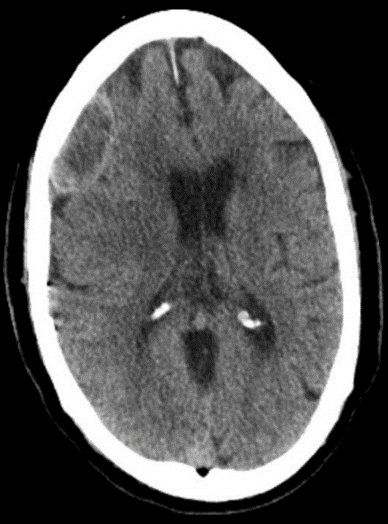
The patient was brought to the interventional radiology suite and prepared for cerebral angiography under general anaesthesia. On selective injection of the external carotid artery, hyperemia was noted at the ends of the distal branches of the middle meningeal artery, indicative of neovascularization contributing to right sided subdural hematoma expansion. The previously placed coil was visualized at the bifurcation of the right middle meningeal artery with delayed but present anterograde filling in the distal anterior and posterior divisions (Figure 2). An Echelon 0.014 microcatheter with a straight tip was advanced over a Synchro 2 standard microwire past the non-occlusive, previously placed coil and into the distal parietal branch of MMA, followed by DMSO then Onyx 18 until reflux along the microcatheter tip was seen. Post-embolization injections demonstrate that there is no residual supply to the dura via the posterior or anterior divisions of the MMA (Figure 3). The patient tolerated the procedure well and was discharged within several days of embolization. The patient’s head CT at 3 months after the procedure showed marked reduction in SDH volume (Figure 4).
Figure 3: Post-Embolization Digital Subtraction Angiography of the Right ECA: Total occlusion of the MMA with no filling of the subdural membranes.
Figure 4: Follow-up head CT: 3-month follow-up head CT shows decreased volume and mass effect of SDH.
Discussion
Pathogenesis and propagation of subdural hematoma is complex and incompletely understood. Current evidence suggests an interplay of inflammation, angiogenesis, local coagulopathy, recurrent microbleeds, and exudates [2-4]. Growing evidence has established a definitive role of the middle meningeal artery both in pathogenesis and treatment [5, 6]. While recent literature has highlighted the efficacy of MMA embolization, comparative analysis of endovascular techniques and literature on management when embolization fails is rare. Onyx is a liquid non-adhesive embolysate of ethylene vinyl alcohol copolymers immersed in dimethyl sulfoxide. The present report highlights the advantages of the Onyx liquid embolysate over coil embolization in patients with chronic SDH. Figures 2 and 3 highlight the efficacy of liquid embolization over coil techniques in halting anterograde filling of the MMA. Additionally, liquid embolysate permeates distal branches to prevent retrograde filling from external circulation collaterals, a distinct advantage to coil embolization [10].
To the authors’ knowledge, only one other case report has discussed management of patients with chronic SDHs that have failed MMA embolization. Rutledge et al. reports the efficacy of contralateral MMA embolization in a patient with SDH expansion after coil embolization of the ipsilateral MMA [11]. We recommend that in situations of MMA embolization failure with incomplete distal embolysate penetration, repeat angiography should be considered to determine if more extensive embolization is possible. The patient presented here had residual filling of the MMA despite prior intervention, which guided our decision to attempt further embolization. Future studies should review angiography of larger cohorts of patients with chronic SDHs that have failed MMA embolization for more extensive endovascular recommendations.
Conclusion
Liquid embolization is more effective than coil embolization in halting anterograde filling of the MMA and retrograde filling from external circulation collaterals in patients with chronic SDHs. In situations of embolization failure, follow-up angiography may be indicated to determine whether more extensive embolization of the MMA can be accomplished.
Author Contributions
All authors contributed equally to the production of this manuscript.
Funding
None.
Conflicts of Interest
None.
Abbreviation
MMA: Middle Meningeal Artery
SDH: Subdural Hematoma
Article Info
Article Type
Case ReportPublication history
Received: Wed 11, Aug 2021Accepted: Wed 25, Aug 2021
Published: Fri 03, Sep 2021
Copyright
© 2023 Dimitri Sigounas. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CRSS.2021.02.02
Author Info
Kenneth Sack George Thomas Dimitri Sigounas
Corresponding Author
Dimitri SigounasDepartment of Neurosurgery, George Washington University, Washington, D.C., USA
Figures & Tables

References
1. Balser D, Farooq S,
Mehmood T, Reyes M, Samadani U (2015) Actual and projected incidence rates for
chronic subdural hematomas in United States Veterans Administration and
civilian populations. J Neurosurg 123: 1209-1215. [Crossref]
2. Weigel R,
Hohenstein A, Schilling L (2014) Vascular endothelial growth factor
concentration in chronic subdural hematoma fluid is related to computed
tomography appearance and exudation rate. J Neuotrauma 31: 670-673. [Crossref]
3. Stoodley M, Weir B
(2000) Contents of chronic subdural hematoma. Neurosurg Clin N Am 11:
425-434. [Crossref]
4. Wilberger JE (2000)
Pathophysiology of evolution and recurrence of chronic subdural hematoma. Neurosurg
Clin N Am 11: 435-438. [Crossref]
5. Ban SP, Hwang G,
Byoun HS, Kim T, Lee SU et al. (2018) Middle Meningeal Artery Embolization for
Chronic Subdural Hematoma. Radiology 286: 992-999. [Crossref]
6. Kim E (2017)
Embolization Therapy for Refractory Hemorrhage in Patients with Chronic
Subdural Hematomas. World Neurosurg 101: 520-527. [Crossref]
7. Link TW, Boddu S,
Paine SM, Kamel H, Knopman J (2019) Middle Meningeal Artery Embolization for
Chronic Subdural Hematoma: A Series of 60 Cases. Clin Neurosurg 85:
801-807. [Crossref]
8. Link TW, Rapoport
BI, Paine SM, Kamel H, Knopman J (2018) Middle meningeal artery embolization
for chronic subdural hematoma: Endovascular technique and radiographic
findings. Interv Neuroradiol 24: 455-462. [Crossref]
9. Catapano JS, Nguyen
CL, Wakim AA, Albuquerque FC, Ducruet AF (2020) Middle Meningeal Artery
Embolization for Chronic Subdural Hematoma. Front Neurol 11: 557233. [Crossref]
10. Fiorella D, Arthur AS (2019) Middle meningeal artery embolization for the management of chronic subdural hematoma. J Neurointerv Surg 11: 912-915. [Crossref]
11. Rutledge C, Baranoski JF, Catapano JS, Jadhav AP, Albuquerque FC et al. (2021) Resolution of an enlarging subdural haematoma after contralateral middle meningeal artery embolisation. BMJ Case Rep 14: e017530. [Crossref]
