Regulation of Bone’s Metabolic Process under Dental Implantation Procedure
A B S T R A C T
Aim: increase of efficiency of dental implantation in patients with imbalance of bone remodeling processes.
Material and Methods: under observation were men with osteoporosis, who applied for restoration of defects of the dentition with dental implants. Correction of bone remodeling imbalance was performed with bisphosphonates, calcium and vitamin D preparations. Before dental implantation, the state of microarchitectonics of the lower jaw was studied using cone-beam computed tomography, histomorphometry, and the state of mineral metabolism in the blood.
Results and Conclusions: the success of osseointegration dental implantation in patients with bone remodeling imbalance is determined by the qualitative parameters of the bone tissue, of the receiving bed, reflecting metabolic and reparative processes. Complex antiosteoporetic therapy with bisphosphonates and calcium preparations with vitamin D helps to restore the qualitative parameters of the alveolar part and helps to optimize the processes of osteointegration.
Keywords
Osteoporosis, dental implantation, bone remodeling, osseointegration, bisphosphonates, vitamin D
Introduction
Improving the effectiveness of implantological treatment of patients with osteoporosis remains an urgent problem of modern dentistry. The basis of the pathogenesis of this pathology is determined by the imbalance of bone remodeling processes, in which osteointegration is suppressed with a high frequency of early and late postoperative complications from 10 to 44% [1, 2]. To date, a correlation between systemic osteoporosis and bone loss of the alveolar part (processes) of the jaws has been established [3, 4]. It was established that long-term survival of dental implants in patients with this pathology is only 66% [5].
It's noted that every third man with an imbalance of bone remodeling processes has a low level of testosterone [6]. In androgen deficiency the phase of bone resorption prevails over its synthesis, which leads to the presence of defects in the dentition with atrophy of the alveolar process (part) of the jaws and a decrease in reparative processes in the surgical intervention zone [3, 7]. Testosterone deficiency is widespread in older men, which is characterized by the development of atrophic and proliferative processes in the prostate gland. Although there is currently no conclusive evidence that hormone replacement therapy in men increases the risk of prostate cancer it is necessary to consider that it has hormonal regulation mechanisms. Drug correction of androgen deficiency with testosterone can lead to functional and structural reorganization of the gland, and in the presence of metaplastic processes can provoke the occurrence of cancer [8]. In addition, men in the presence of hypogonadism associated with obesity often suffer from episodes of sleep apnea, and testosterone treatment can exacerbate this condition [9].
The success of the osseointegration processes largely determines the perceived bony, therefore, important to study bone micro-zone planning of dental implantation, as it is a reflection of what is happening in it of metabolic processes. The state of bone remodeling plays a significant role in maintaining optimal quantitative and qualitative characteristics of the jaw bones and serves as a prognosis for the development of complications at different stages of the postoperative period [10]. To date, the gold standard in the evaluation of bone microarchitectonics is histology with histomorphometric study.
Bone dysregeneration and inhibition of osteoarthritis may be due to, among other things, an increased content of parathyroid hormone (PTH), secreted by the main cells of the parathyroid glands, with a decrease in the level of ionized calcium (Ca2+) in the blood. In bone, this hormone stimulates the mobilization and release of Ca2+ into the blood, by activating the activity of osteoclasts (CA). The launch of osteoclastogenesis in hypersynthesis of PTH causes activation and prolongation of the resorption phase, demineralization of the bone matrix and decrease in BMD [6, 10, 11]. Increased concentration parathyrin inhibits the production of calcitonin (CAT), an important biological impact which protects the skeleton from decalcification (inhibits differentiation and activity of OK, and promotes their apoptosis), hence the importance of determining the concentrations of PTH and CAT in the blood to control the state of bone metabolism and successful dental implantation [11].
In modern pathogenetic therapy of osteoporosis, the leading role of bisphosphonates is recognized, the main pharmacological effect of which is to reduce the rate of bone remodeling with inhibition of the resorption phase [8]. Calcium and vitamin D preparations are an obligatory component of treatment [6, 11, 12]. The aim of the study was to increase the efficiency of dental implantation in patients with an imbalance of bone remodeling processes.
Materials and Methods
The examination and treatment included 80 men over 50 years of age who applied for restoration of defects of the dentition with the help of dental implantation. Criteria for inclusion of patients of the main groups: men with unilateral terminal defects of the dentition on the lower jaw without atrophy of the alveolar part with diagnosed osteoporosis in the presence of age-related hypogonadism (with densitometric study of the lumbar spine and proximal femur, the T-criterion was minus 2.5 SD and below.
To identify the criteria of norm formed I (control) group of 30 men without violation of the processes of bone remodeling (densitometric study of the axial and proximal parts of the skeleton Ttotal criterion was within normal values and was minus 0.8 ± 0.2 and minus 0.7 ± 0.1, respectively, blood counts on bone metabolism and androgenic status were within the reference values). Depending on the reception antiosteoporotic therapy patients with osteoporosis were divided into groups:
II 30 people without antiresorptive therapy (not taking bisphosphonates with calcium and vitamin D preparations).
III 30 men taking ibandronate 1 tablet (150 mg) 1 time per month with calcium and vitamin D preparations (1000 mg / 800 IU) daily.
The purpose antirezorbtivei therapy was conducted by Doctor of Medical Sciences, honored doctor of Russia, head of the department of endocrinology and diabetology of the medical faculty of MSMSU named after A. I. Evdokimov, Professor A. M. Mkrtumyan. Taking into account possible complications of hormone therapy in men over 50 years in the form of functional and structural adjustment of the prostate gland, the presence of episodes of sleep apnea, as well as motivated refusal to use testosterone drugs, HRT was not carried out. Clinical dental examination of patients with partial absence of teeth included examination, palpation, x-ray examination-cone-beam computed tomography performed on a dental tomograph ProMax 3D ("Planmeca", Finland).
At the planning stage of dental implantation, mineral metabolism was studied by indicators in the blood: 1) total calcium by arsenazo-111 on the analyzer "Flexor" (Vital Scientific, Netherlands) by the calibrator BIOCON 2003 (Biocon Limited, India); 2) ionized calcium by the jonselective method on the analyzer "EASYLYTE" (Medica Corporation, USA); 3) calcium hormones: parathyrine (PTH) by the reagent LKPP, calibrators LPHL, lphh; calcitonin reagent lkcl, lcll calibrators, Lclh by solid-phase chemiluminescent immunoassay on autoanalyzer "IMMULITE" (DPC Cirrus Inc., USA); 4) marker of osteocalcin bone formation by solid-phase chemiluminescent immunoassay on "Immulite" autoanalyzer with lkon1 reagent, lonl calibrators, LONH (DPC Cirrus Inc. 5) marker of bone resorption, collagen degradation product β-CrossLaps by electrochemiluminescent immunoassay on autoanalyzer "Elecsys" reagent and calibrators 11972308122 (Roche Diagnostics, Switzerland). Reference values: total calcium-2.1-2.6 mmol / l, ionized calcium-1.06-1.31 mmol/l, PTH-7-53 PG / ml, CAT-3-13 ng/l, osteocalcin-3.1-13.7 ng / ml, β-CrossLaps-0.01-0.6 ng / ml.
Dental implantation was performed according to the standard protocol, in the postoperative period, anti-inflammatory (nimesulide 50 mg 1 tablet 2 times a day for 5 days) and antibiotic therapy (amoxicillin 875 mg with clavulanic acid 125 mg 1 tablet 2 times a day for 7 days) were prescribed. During the surgery, a 3x3 mm trepan biopsy of bone samples with cortical and spongy structures was performed using a hollow cutter. Tissue samples were fixed in 10% neutral formalin solution (pH 7.0-7.2), then decalcified using the reagent Biodec R ("BioOptica", Italy). Then, according to the generally accepted method, they were poured into paraffin blocks, made sections with a thickness of 3-4 microns, stained with hematoxylin and eosin, the preparations were studied using a microscope Leica DM 1000 LED and a digital camera Leica EC 3 (Leica Microsystems, Germany).
Histomorphometric analysis was carried out in a semi-automatic specialized computer program T-denta with the calculation of the volume of the spongy bone-TBV (%), the width of bone trabeculae - Tb. Th (microns) and the total resorbed surface of the spongy bone-ES/BS (%) [13].
Results
In the clinical examination and analysis of CBCT in all patients in the area of missing teeth, the bone volume was sufficient for dental implantation, the width of the alveolar part > 5 mm, the height-10 mm or more. Indicators of mineral metabolism of patients of the I (control) group without osteoporosis before dental implantation were within the reference values (Table 1).
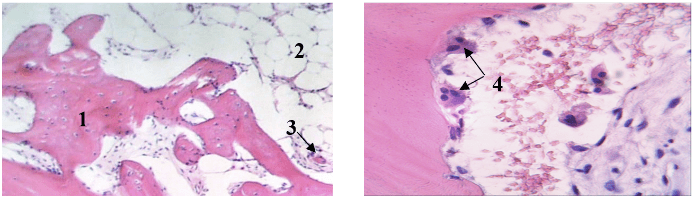
Histological preparations were used to determine anastomosing bone trabeculae with the presence of red bone marrow between them, in the endoossal layer − multiple flattened inactive osteogenic cells. Trabeculae had a smooth medullary surface, osteocytes were visualized in the thickness of bone structures, the lines of adhesion were clearly contoured, which indicates active metabolic processes (Figure 1).
Table 1: Indicators of mineral metabolism of men of the studied groups.
|
Blood counts |
Group I (test) |
Group II (without anti-osteoporetic therapy) |
Group III (before taking antiosteoporotic therapy) |
|
Total calcium (mmol / l) |
2,46 ± 0,12 |
2,45 ± 0,15 |
2,43 ± 0,14 |
|
Ionized calcium (mmol / l) |
1,2 ± 0,1 |
1,13 ± 0,07 |
1,21 ± 0,09 |
|
PTH (PG / ml) |
45,7 ± 5,95 |
59,8 ± 7,2* |
72,5 ± 8,12** |
|
CAT (ng/l) |
3,8 ± 0,7 |
2,5 ± 0,4** |
1,2 ± 0,8*** |
|
Osteocalcin (ng/ml) |
6,25 ± 1,25 |
3,75 ± 0,85*** |
2,4 ± 0,76*** |
|
ß-CrossLaps (нг/мл) |
0,45 ± 0,13 |
0,69 ± 0,1* |
0,73 ± 0,04* |
Note: * - p <0.05, * * - p <0.01, * * * - p <0.001
Figure 1: Histological preparations of group I (control) patients, a-patient G., 65 years (increase 200x), b-patient X., 56 years, (increase 400x), color: hematoxylin-eosin. 1-bone trabeculae, 2-red bone marrow, 3-bonding lines, 4-inactive flattened osteogenic cells.
Histomorphometric indicators: TBV 64.28 ± 3.84, Tb.Th 317.03 ± 10.44, ES/BS 14.66 ± 0.9.
After dental implantation and 3 months, gum shapers were installed, followed by orthopedic treatment. Pathological changes on the part of the bone and soft tissue components were not observed. In group II of men who do not take complex antiosteoporetic therapy, the analysis of bone metabolism indicators revealed at normal values of total and ionized calcium hypersecretion of PTH by 30.8% above the control level, a decrease in the concentration of CAT and osteocalcin by 34.2% and 40%, respectively, an excess of 1.5 times the marker of bone resorption β-Cross laps, which indicates a high rate of bone metabolism with a predominance of the resorption phase (Table 1).
Histological examination of preparations of this group of men showed thinned, pitted bone beams with a large number of osteoclasts in resorptive lacunae, the phenomenon of free trabeculae, single inactive flattened osteogenic cell elements in the endoossal layer. Replacement of red bone marrow with adipose tissue was detected in the interbalance space. The trabeculae contoured sparse bonding lines, far apart (Figure 2).
Figure 2: Histological preparations of group II patients, a-patient J., 61 years (increase 200x), b-patient V., 59 years, (increase 400x), color: hematoxylin−eosin. 1-bone trabeculae, 2-adipose tissue, 3-phenomenon of free trabeculae, 4-osteoclasts in lacunae of resorption.
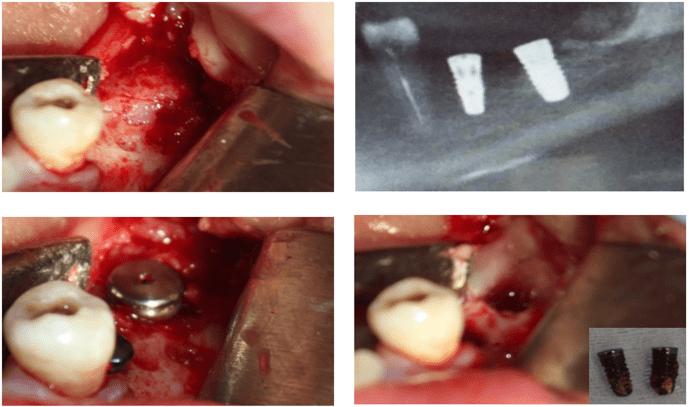
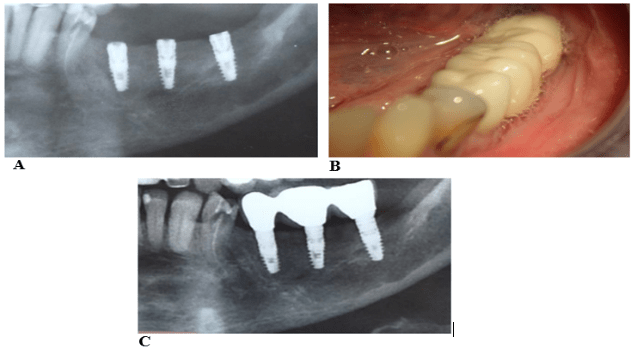
Analysis of histomorphometric parameters of group II men demonstrated qualitative changes in the alveolar part of the mandible. Thus, TBV was 2 times smaller compared to the control group (p <0.05). Loss of bone density was accompanied by a decrease Tb.Th by 45.6% (p <0.01), increasing ES/BS by 2.6 times (p <0.01). After dental implantation, these patients developed periimplantitis, implants were removed in 7 people after 1 month, in 13-the absence of osseointegration was determined after 3 months at the stage of installation of the gum shaper (Figure 3).
Figure 3: Clinical example of patient G., 56 years old, a-exfoliated Muco-periosteal flap, b-dental implants were installed in the area of missing 3.6, 3.7, C-CLCT of the lower jaw on the right, panoramic reformed after the installation of dental implants, d-implants were removed after 3 months.
Indicators of bone metabolism of group III men before receiving antiresorptive therapy indicated the development of secondary hyperparathyroidism associated with hypersecretion of PTH by 1.5 times with normal total and ionized calcium in the blood, a low concentration of CAT (68.4% lower than the control group) and osteocalcin (a decrease of 61.6%), excess of β-Cross laps by 1.6 times (Table 1) was determined. After 3 months of treatment with ibandronate, 1 tablet (150 mg) 1 time per month with calcium and vitamin D preparations (1000 mg / 800 IU) daily, bone metabolism in the blood was within the reference values.
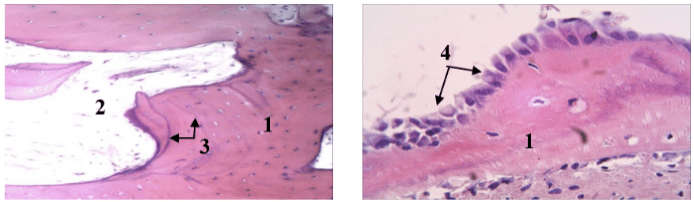
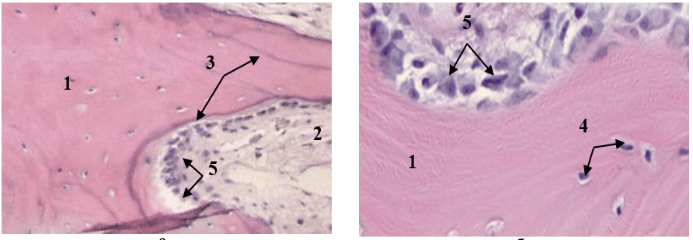
On biopsy preparations in this group of men, interconnected trabeculae were traced, along the periphery of which a large number of activated osteoblasts and a newly formed osteoid were visualized in the presence of resorptive lacunae and single osteoclasts. Rare elements of adipose tissue in the peritrabecular space, numerous lines of adhesion in the bone beams indicate the activation of bone remodeling processes (Figure 4, 5).
Figure 4: Histological preparations of group III patients after 3 months of antiosteoporetic correction, a-patient D., 64 years (increase 200x), b-patient G., 62 years (increase 400x), color: hematoxylin−eosin. 1-bone trabeculae, 2-red bone marrow, 3-bonding lines, 4-active osteoblasts.
Figure 5: Histological preparations of group III patients after 3 months of antiosteoporetic correction, a-patient K., 68 years (200x increase), b-patient O., 57 years (400x increase), hematoxylin−eosin staining; 1-bone trabeculae, 2-red bone marrow, 3-bonding lines, 4-osteocytes, 5-osteoblasts.
Before prescribing antiresorptive drugs, the following histomorphometric values were recorded in group III patients: TBV-32.11 ± 10.44, Tb.Th – 172,22 ± 9,81, ES/BS-38,15 ± 0,7, on the background of antiosteoporetic correction the studied parameters of histomorphometry corresponded to control values. After 3 months after dental implantation, gum shapers were installed with subsequent orthopedic treatment. Dynamic control, after 1, 3 years, did not reveal pathological changes in the bone tissue of the alveolar part of the lower jaw and surrounding soft tissues (Figure 6).
Figure 6: Clinical example of patient K., 63 years old, a-mandibular CLCT on the left after dental implantation, b-cermet crowns on implants in the oral cavity, C-mandibular CLCT on the left 1 year after dental implants.
Discussion
For successful osseointegration during dental implantation in patients with an imbalance of bone remodeling processes, the qualitative parameters of the bone tissue of the receiving bed, reflecting metabolic and reparative processes, are of great importance. Histological analysis of biopsy material of the alveolar part of the lower jaw in the area of missing teeth of patients with osteoporosis and evaluation of histomorphometric parameters revealed quantitative and morphofunctional changes in bone tissue.
Patients with risk factors for metabolic osteopathies before dental implantation should study the state of mineral metabolism (total and ionized calcium, PTH, CAT, markers of bone resorption and bone formation), in case of its violation should be referred to an endocrinologist. Complex antiosteoporetic therapy with ibandronate 150 mg per month with calcium and vitamin D preparations (1000mg / 800 IU) according to CLCT and histomorphometric study contributes to the restoration of alveolar microarchitectonics.
Article Info
Article Type
Research ArticlePublication history
Received: Thu 19, Dec 2019Accepted: Tue 31, Dec 2019
Published: Sat 04, Jan 2020
Copyright
© 2023 A.S. Belyakova. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.ORD.2019.01.06
Author Info
A.M. Mkrtumyan A.S. Belyakova L.S. Dzikovitskaya M.V. Kozlova
Corresponding Author
A.S. BelyakovaCentral State Medical Academy of the Department of Presidential Affairs, Moscow, Russia
Figures & Tables
Table 1: Indicators of mineral metabolism of men of the studied groups.
|
Blood counts |
Group I (test) |
Group II (without anti-osteoporetic therapy) |
Group III (before taking antiosteoporotic therapy) |
|
Total calcium (mmol / l) |
2,46 ± 0,12 |
2,45 ± 0,15 |
2,43 ± 0,14 |
|
Ionized calcium (mmol / l) |
1,2 ± 0,1 |
1,13 ± 0,07 |
1,21 ± 0,09 |
|
PTH (PG / ml) |
45,7 ± 5,95 |
59,8 ± 7,2* |
72,5 ± 8,12** |
|
CAT (ng/l) |
3,8 ± 0,7 |
2,5 ± 0,4** |
1,2 ± 0,8*** |
|
Osteocalcin (ng/ml) |
6,25 ± 1,25 |
3,75 ± 0,85*** |
2,4 ± 0,76*** |
|
ß-CrossLaps (нг/мл) |
0,45 ± 0,13 |
0,69 ± 0,1* |
0,73 ± 0,04* |
Note: * - p <0.05, * * - p <0.01, * * * - p <0.001

Histomorphometric indicators: TBV 64.28 ± 3.84, Tb.Th 317.03 ± 10.44, ES/BS 14.66 ± 0.9.
References
- Musheev IU, Olesova VN, Frumovich OZ (2000) Practical dental implantology. Moscow: Nemchinskaya printing house.
- Mombelli A, Müller N, Cionca N (2012) The epidemiology of peri-implantitis. Clin Oral Implants Res 23: 67-76. [Crossref]
- Kozlova MV, Mkrtumyan AM, Panin AM (2015) Dental implantation in patients with endocrine pathology (features of bone remodeling, diagnosis and correction of metabolic disorders). Moscow: Medforum
- Namkhanov VV, Pisarevsky YL, Plekhanov AN (2014) The role (influence) of osteoporosis on the condition of the facial skeleton and dentoalveolar system. Bulletin Buryat State University 12: 90-93.
- Gun'ko MV (2009) Osteoporosis and dental implantation. Dentistry 88: 73-78.
- Benevolenskaya LI (2005) Osteoporosis Diagnosis, prevention and treatment. Moscow: GEOTAR.
- Smetnik VP, Burduli AG (2011) Androgens and bone tissue. Problems reproduction 5: 110-115.
- Tyuzikov IA (2012) Effect of obesity and androgen deficiency on the blood circulation of the prostate gland. Bulletin Siberian Medicine 2: 80-83.
- Bhasin S, Cunningham GR, Hayes FJ et al. (2006) Testosterone therapy in adult men with androgen deficiency syndromes: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 91: 1995-2010.
- Yanushevich OO, Kozlova MV, Mkrtumyan AM et al. (2014) Qualitative assessment of jawbones in patients with complex anti-osteoporherapeutic therapy. Russian Dentistry 4: 34-40.
- Kotelnikov GP, Bulgakov SV (2010) Osteoporosis: a guide. Moscow: GEOTAR-Media.
- Rudenko EV, Buglova AE, Rudenko EV, Samohovets OY (2011) Medicamentous treatment of osteoporosis in adults: uch.-method. allowance. Minsk: BelMAPO.
- Kozlova MV, Panin AM, Zayratyants OV (2011) The method of histomorphometric evaluation of the jawbones. Certificate of state. registration of the computer program № 2011610399 of 11.01.2011.
