Radiation-Related Hypopharynx-Stenosis with Spared Larynx Treated by a Novel-Shaped Silicone Stent
A B S T R A C T
Background: Radiation-related hypopharyngeal stenoses are considered as complications after larynx sparing therapy of hypopharyngeal or laryngeal tumors.
Methods: The reported patient suffered from chondronecrosis of the cricoid after radiation of a larynx carcinoma and was treated by removing the necrotic cartilage. To prevent emerging stenosis of the hypopharynx, a customized hypopharyngeal stent was constructed on the basis of CT scan data. The Y-shaped stent was placed dorsal to the larynx, caudal to the arytenoid cartilages and remained in place without dislocation or irritation of the larynx for 8 weeks. During that time, the hypopharynx was stented, and the mucosa grew around the stent covering the complete circumference of the hypopharynx again. 18 weeks after removal of the stent, the hypopharynx did not reveal any re-stenosis.
Conclusion: This customized hypopharyngeal stent is the first reported approach applied with spared larynx, which has been tolerated for a long period of time.
Keywords
Post-cricoid stenosis, hypopharyngeal stent, organ sparing, prosthesis, larynx
Introduction
Radiation-related stenoses of the hypopharynx are severe complications occurring in up to 20% of the cases [1, 2]. The placement of salivary bypass tubes has been reported for several weeks in laryngectomized patients [3]. The long-term placement of silicone stents in patients with a spared larynx has not been reported yet. Self-expanding covered and un-covered stents implicate the risk of dislocation and the development of pharyngocutaneuos fistulas even in laryngectomized patients and have also not been reported for larynx spared patients [4]. Herein, we present the first case of a patient with a stenosis of the hypopharynx and preserved larynx treated with a customized silicone stent.
Case Report
A male patient was treated for supraglottic laryngeal cancer (diagnosed April 2019, cT4cN1cM0, squamous cell carcinoma G3) by larynx sparing radiochemotherapy. The total radiation dose was 70 Gy at the tumor site, 65 Gy at the complete larynx, including the bilateral cervical regions II and III and 61 Gy at the bilateral cervical regions Ia/b, IV and V as well as the retropharyngeal region and II and III of the left side with a daily dose of 1.99 Gy accompanied by cisplatin (25mg/m2) and 5-FU (600mg/m2) at day 1-4 as well as 29-32. Towards the end of the radiation (June 2019), difficulties in swallowing solid nutrition occurred and remained present since that time. 6 months (November 2019) after the termination of the radiochemotherapy, the post-cricoid mucosa was edematous and tight. A residual carcinoma was ruled out by CT scan and biopsies. The stenosis was dilated by bougies up to 12 mm in diameter (Coloplast®, Humblebæk, Denmark), resulting in temporary relief and was repeated 2 months later. Due to recurrent swallowing restrictions, a surgical jejunostomy was performed in February 2020. Six months later (August 2020), a rigid endoscopy was conducted again due to the inability of swallowing fluids and saliva, including increasing aspiration.
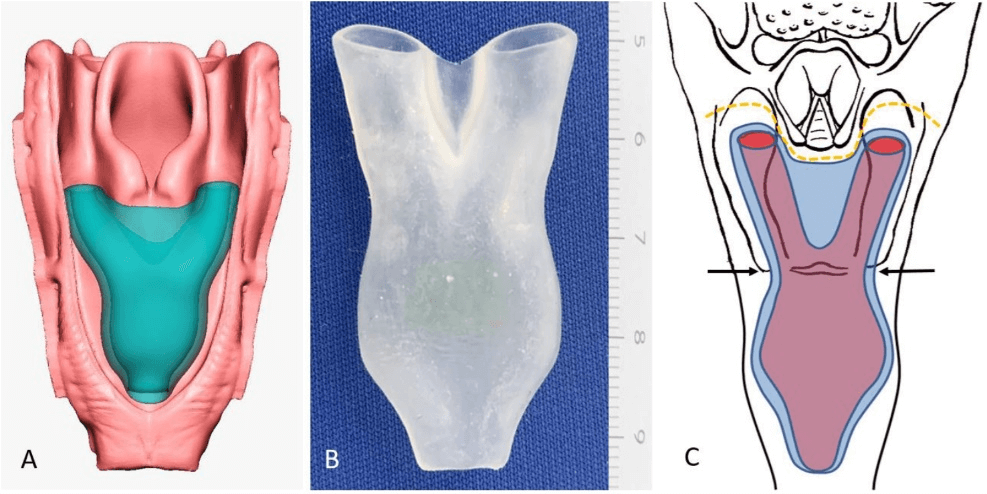
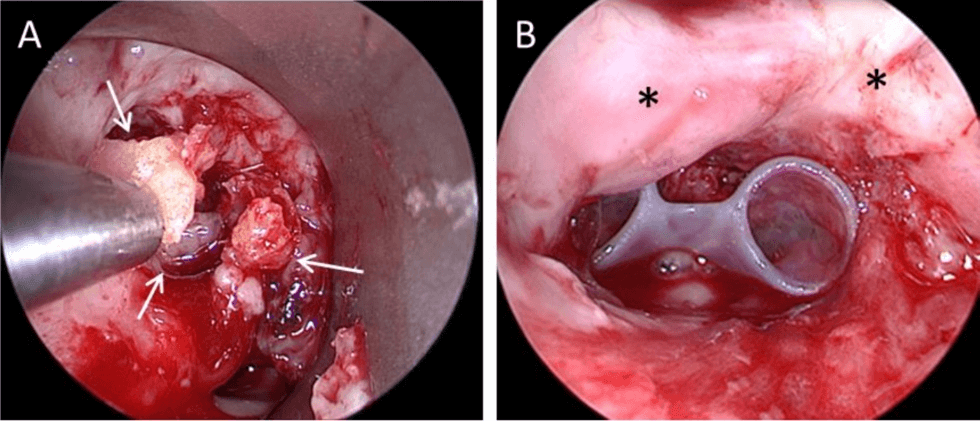
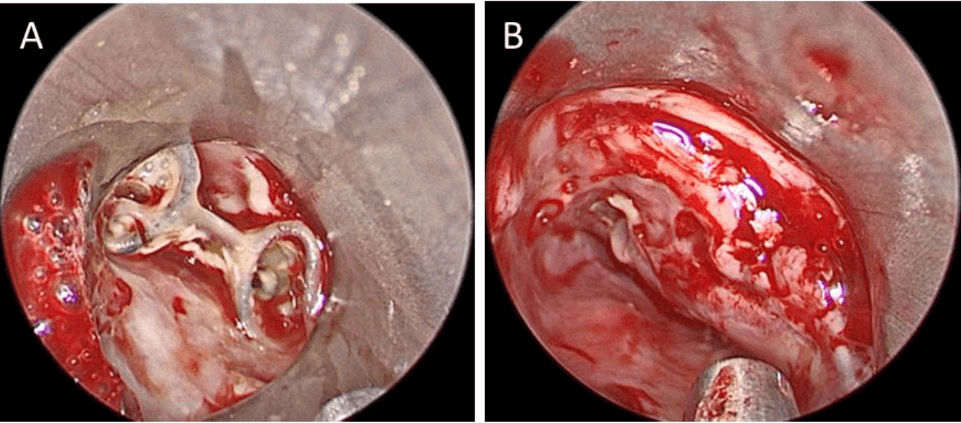
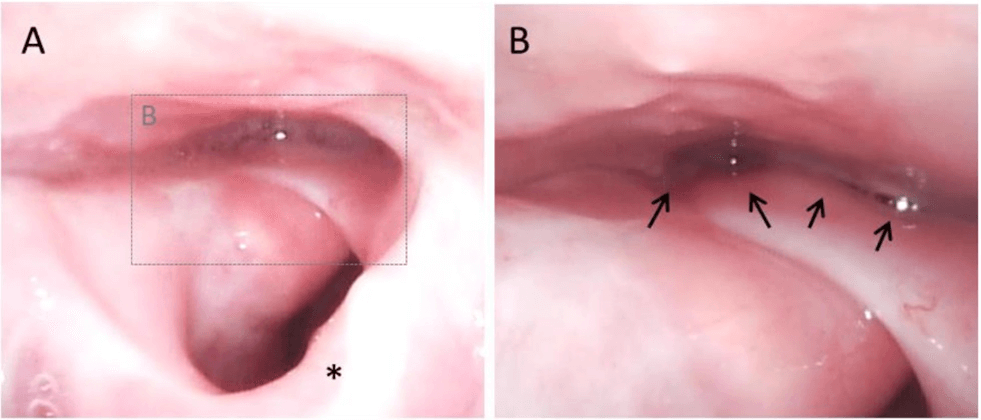
The endoscopy revealed a subtotal edematous hypopharyngeal stenosis and post-cricoidal ulceration. Pieces of necrotic cricoid cartilage were removed. A permanent tracheostomy was performed. The histopathological examination revealed a chondronecrosis of the cricoid cartilage (Figure 2A). A recurrent carcinoma was ruled out. An individual treatment approach was discussed with the patient and written consent was given. Prior to another endoscopy, a prototype of a novel hypopharyngeal silicone stent was constructed on the basis of CT scan data. (3D Slicer V4.10.2, Link) [5]. The construction of the stent was performed by Freeform Plus® (3D Systems/ Geomagic, Rock Hill, SC, USA), as well as the mold, which was printed on a Polyjet Printer (3D Systems Projet 2500Pro®, Rock Hill, SC, USA). The mold was filled with a medical grade2 silicone of a hardness of 50 shore (Odontosil 50, Dreve-Dentamid, Unna, Germany) (Figures 1A, 1B & 1C). The stent was inserted on September 4th, 2020 (Figure 2B) and removed 8 weeks later, on October 28th, 2020 (Figures 3A & 3B). During that time, the stent was tolerated well and did not dislocate. At follow-up checks 6, 23 (Figures 4A & 4B) and 40 weeks after stent removal, the post-cricoid passage was still open and soft oral nutrition was possible.
Figure 1: Customized hypopharyngeal stent. A) 3D-image of the constructed stent. B) Image of the manufactured silicone stent. C) Schematic drawing of the stent in situ. The outer shape is given in blue; the hollow inner tube is displayed in violet. The Y-shape of the stent prevents a caudal dislocation, while the flat balloon at the caudal end prevents a cranial dislocation. The narrowest part of the stent is located at the cricoid cartilage (arrows). The orange dotted line indicates the maximum cranial extension of the stent. The arytenoid cartilages above the line must not get into contact with the stent to avoid aspiration and coughing, which will result in a dislocation of the stent.
Figure 2: Endoscopic view of the retrolaryngeal region. A) Necrotic cartilage of the cricoid (white arrow) is removed (August 2020). B) Placed hypopharyngeal stent on September 4th, 2020. The arytenoid cartilages are marked with asterisks (interaytenoid fold between the asterisks) and are not in contact with the upper rim of the stent.
Figure 3: Endoscopic view on October 28th, 2020. A) The stent is still in place below the arytenoid cartilages. B) Hypopharynx after stent extraction. Some granulation tissue is visible dorsal to the arytenoid cartilages corresponding to the cranial rim of the stent.
Figure 4: Endoscopic view in the wake patient on April 7th, 2020 (23 weeks after stent extraction). A) View at the larynx. The deformed epiglottis is marked by an asterisk. The enlarged view at the hypopharynx is marked by grey dotted lines. B) Enlarged view of the hypopharynx, which is still wide without recurrent stenosis (arrows).
Discussion
The presented case report introduces a novel stent for the treatment of hypopharyngeal stenosis in a patient with a spared larynx. Remarkably, the stent was tolerated and did not dislocate over a long period of time. The major problems in long-term stenting of post-cricoid stenosis in a spared larynx are the risk of dislocation and the low tolerability of the stent. Custom salivary bypass tubes tend to dislocate cranially due to the cranial cone. Aspiration and heavy coughing urge an early removal of the stent. A potential long applicable hypopharyngeal stent needs to be shaped in a special way to keep itself in position even when swallowing and coughing.
The presented stent is manufactured in a sandglass shape with a Y-shaped cranial section and a flattened balloon at the caudal end. The wings of the Y are placed in the piriform recess without contact with the arytenoid cartilages. Cranial to the cricoid cartilage, the wings of the Y rejoin. The narrowest section of the stent reflects the cricoid. Below the cricoid, the stent expands as a flat balloon. Due to the wings of the Y and the balloon, a dislocation can be prevented in either cranial or caudal direction. It seems to be important that the upper rim between the wings of the Y remains below the arytenoid cartilages to avoid direct contact and prevent granulations as well as heavy coughing. The stent is hollow in a Y-shaped tube to enable the drainage of saliva, whereas oral nutrition is not intended to pass the tube.
Conclusion
The novel-shaped stent seems to have an adequate shape to be tolerated for a long time without coughing and dislocation in patients with spared larynx and hypopharyngeal stenosis. The application for several weeks most likely prevents the formation of recurrent stenoses and supports the reorganization of the mucosal layer of the hypopharynx. More research needs to be conducted to obtain detailed data on the dimensions of the hypopharynx in order to standardize the size of the novel-shaped stent.
Conflicts of Interest
None.
Funding
None.
Author Contributions
Manufacturers of the stent: Andreas Velten, Benjamin Velten.
Article Info
Article Type
Case ReportPublication history
Received: Thu 09, Sep 2021Accepted: Thu 23, Sep 2021
Published: Tue 12, Oct 2021
Copyright
© 2023 Michael Herzog. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CRSS.2021.02.04
Author Info
Michael Herzog Andreas Velten Benjamin Velten Vasyl Bogdanov Daniel Grafmans
Corresponding Author
Michael HerzogDeptartment of Otorhinolaryngology, Head and Neck Surgery, Carl-Thiem-Klinikum gGmbH, Cottbus, Germany
Figures & Tables
References
1. Gavriel H, Duong C,
Spillane J, Sizeland A (2013) Bidirectional esophageal dilatation in
pharyngoesophageal stenosis postradiotherapy. Head Neck 35: 733-737. [Crossref]
2. Nguyen NP, Smith
HJ, Moltz CC, Frank C, Millar C et al. (2008) Prevalence of pharyngeal and
esophageal stenosis following radiation for head and neck cancer. J
Otolaryngol Head Neck Surg 37: 219-224. [Crossref]
3. Tirelli G, Baruca
R, Nata FB (2017) Salivary bypass tube placement in esophageal stricture: A
technical note and report of three cases. Auris Nasus Larynx 44:
758-761. [Crossref]
4. Silva RA, Mesquita N, Nunes PP, Cardoso E, Pinto RM et al. (2012) Tracheobronchial Polyflex stents for the management of benign refractory hypopharyngeal strictures. World J Gastroenterol 18: 551-556. [Crossref]
5. Kapur T, Pieper S, Fedorov A, Robin JCF, Halle M et al. (2016) Increasing the impact of medical image computing using community-based open-access hackathons: The NA-MIC and 3D Slicer experience. Med Image Anal 33: 176-180. [Crossref]
