Pyogenic Hepatic Abscess Formation after Roux-En-Y Gastric Bypass: A Case Report and Literature Review of an Infrequently Encountered Postoperative Complication
A B S T R A C T
Introduction and Importance: Pyogenic liver abscess (PLA) is an uncommon postoperative complication of Roux-en-Y gastric bypass (RYGB). Radiological investigations such as abdominal ultrasonography (USG) and computed tomography (CT) are crucial to evaluate and diagnose intra-abdominal abscesses, especially hepatic collections.
Case Presentation: A 66-year-old female patient with multiple comorbidities, including urticaria requiring monoclonal antibody therapy (humera). She underwent an uneventful RYGB to treat her weight regain and reflux after a prior sleeve gastrectomy and presented with diffuse abdominal pain. This occurred on postoperative day 23 after the patient was discharged home. Patient evaluation was initiated by physical examination, laboratory investigations, and radiological diagnostic tools. Chest and abdominal X-rays together with abdominal ultrasonography were unremarkable. Then, abdominal computed tomography (CT) scans with IV contrast were done, and a liver abscess was detected. Image-guided percutaneous transhepatic liver abscess drainage through pigtail drain placement was performed. The patient’s response was evaluated by serial abdominal CT scans. The liver abscess was successfully treated by percutaneous drainage for 5 weeks and IV antibiotic therapy.
Clinical Discussion: PLA is a rare entity that might occur after gastro-intestinal surgery such as Roux-en-Y gastric bypass. Patients with a history of immunosuppressive therapy may be at increased risk of this complication. This life-threatening complication can be prevented by treating liver abscesses early on by utilizing imaging-guided drainage and intravenous antibiotics.
Conclusion: Due to the unusual etiologic origin of hepatic abscess post-RYGB, we report the case of a 66-year-old female with diffuse abdominal pain, which was found to be caused by PLA.
Keywords
Liver abscess, Roux-en-Y gastric bypass, percutaneous drainage, bariatric surgery, case report
Introduction
Bariatric surgeries, such as Roux-en-Y gastric bypass (RYGB), are widely used to treat morbid obesity. Besides its technical advantages, various post-operative complications were reported [1, 2]. Rarely, RYGB is complicated by abscesses of the liver postoperatively [1].
In spite of the fact that liver abscesses are the most common visceral abscess, only 5-15% of them are caused by surgical complications [1]. Laparoscopic Roux-en-Y bypass surgery entails a 1-6% incidence of leaks [2].
Here we report a 66-year-old female patient with multiple comorbidities, including urticaria, requiring monoclonal antibody therapy (humera), who presented with diffuse abdominal pain 23 days after RYGB that was found to be a pyogenic hepatic abscess. Our work has been reported in line with the SCARE Guidelines 2020 criteria [3].
Case Presentation
On her postoperative day 23 of Roux-en-Y gastric bypass, a 66-year-old female patient, with a background history of hypertension, bronchial asthma, and dyslipidemia, urticaria requiring monoclonal antibody therapy, last administered 2 weeks prior to surgery (humera), presenting with a day history of diffuse abdominal pain that is associated with nausea, fever, dark stool, and cough.
She had a surgical history of laparoscopic cholecystectomy and sleeve gastrectomy. On admission, she was vitally stable, abdominal examination revealed non-distended abdomen and right upper quadrant tenderness (Table 1).
Table 1: Patient’s vital
signs and laboratory investigations on admission
|
Patient’s vital signs |
Hematology |
Clinical Chemistry |
|
GCS 15/15 |
WBC 31.8 |
Amylase 16 |
|
BP
121/62 mmHg |
Hb 126 |
Lipase 14 |
|
HR 110 bpm |
Platelets 287 |
Total Bilirubin 27.4 |
|
RR 20 bpm |
Neutrophils 28.60 |
Direct Bilirubin 13.8 |
|
SPO2 99 % on room air |
Lymphocytes 1.79 |
Indirect Bilirubin 14 |
|
Body temperature 39.5 o C |
Monocytes 1.36 |
Albumin 26.4 |
|
|
Eosinophils 0.00 |
ALT 208 |
|
|
PT 27.3 |
AST 286 |
|
|
|
ALP 184 |
|
|
|
Creatinine 56 |
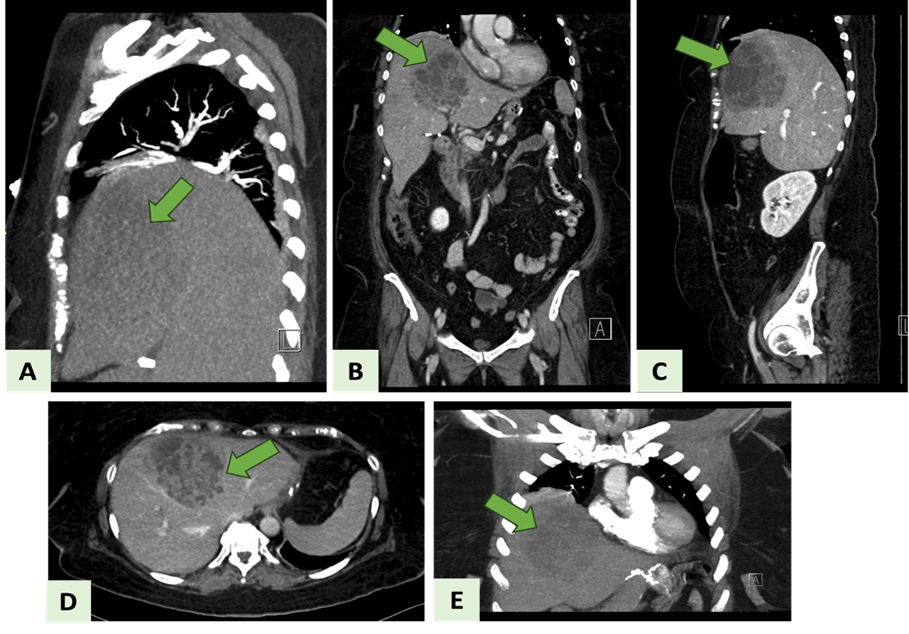
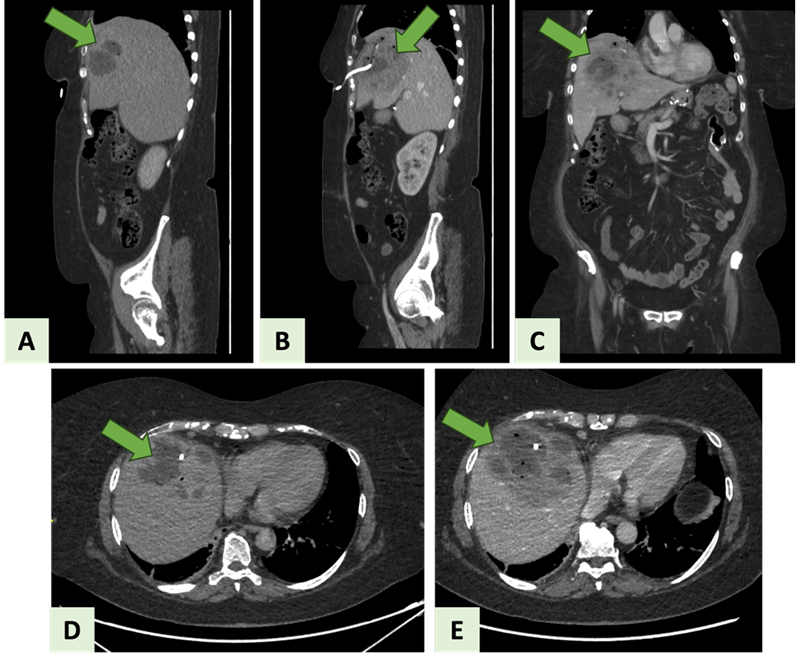
Chest and abdomen X-rays were performed on admission and illustrated in (Figure 1). Abdominal ultrasonography was unremarkable post-gastric bypass study (Figure 2). CT with IV contrast of the chest, abdomen, and pelvis, findings (Figure 3). The liver showed a large multiseptated hypodense lesion noted at segments IV, VIII, and less extent V measuring about 9 × 10 × 11 cm in diameter with peripheral wall and septal enhancement as well as surrounding fat stranding consistent with hepatic abscess. Evidence of gastric bypass with free oral contrast through the bowel loops till reaching the distal ileal loop. No evidence of oral contrast leakage or pneumoperitoneum was noted in the study.
Figure 1: Showing patient’s X-rays on admission. A) Chest X-ray. B) Abdominal X-ray.
Figure 2: A-D) Showing abdominal ultrasonography with normal findings.
Figure 3: CT with IV contrast of the chest, abdomen, and pelvis. The green arrow points to the hepatic abscess. A, C) Sagittal view. B, E) Coronal view. D) Axial view.
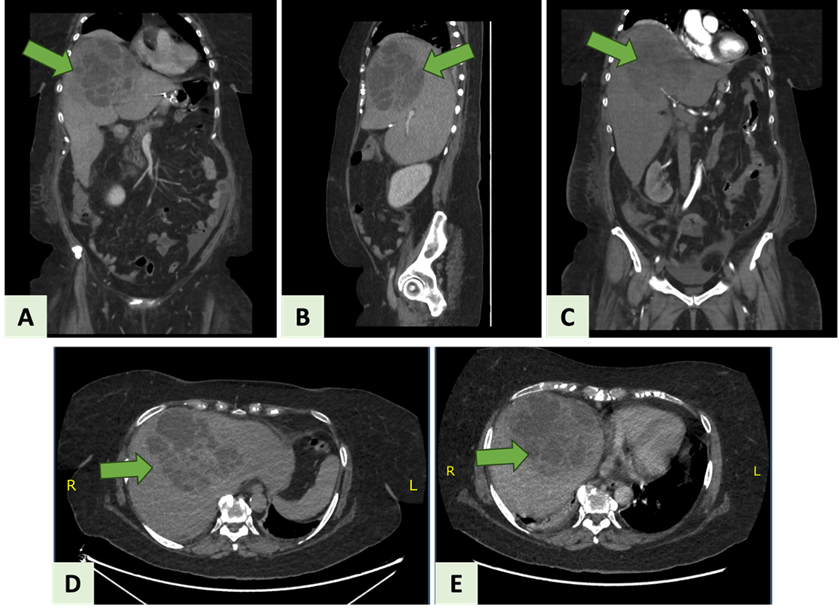
At this point, the hepatic abscess was confirmed, and ultrasound and fluoroscopic-guided percutaneous transhepatic liver abscess drainage through drain placement. During the procedure, an 8 Fr locking pigtail catheter was placed, and after being fixed to the skin it was connected to a collection bag. The pigtail was retained for a few weeks to allow maturation of the track. Subsequently, a new abdominal CT showed liver abscess cavity collapse (Figure 4).
Figure 4: The new abdominal CT. The green arrow points to the hepatic abscess. A, C) Coronal views. B) Sagittal view. D, E) Axial views.
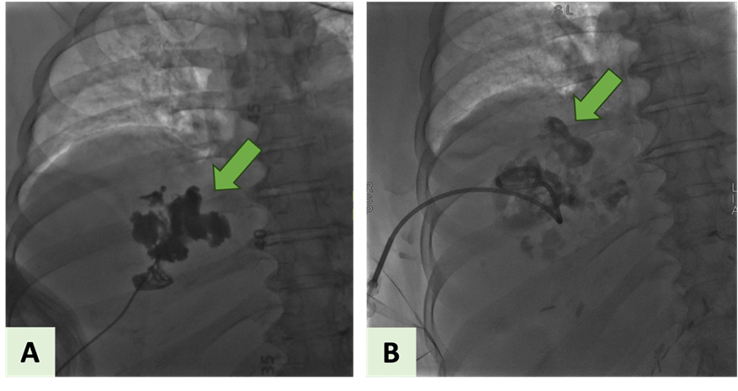
Then, the liver abscess was drained by interventional radiology technique and followed by CT with oral and IV contrast of the abdomen and pelvis done to evaluate the hepatic abscess prior to drainage. In comparison with the previously described large multiseptated lesions that were consistent with liver abscess, the new abdominal CT demonstrated a minimal to mild increase in size, measuring 10.3 × 12.3 × 13.5 cm (Figure 5). Upon follow-up, liver abscess drainage assessment was done by abdominal CT. The recent abdominal CT study showed mild regressive interval change of the hepatic abscess size, measuring about 9 × 9 × 9 cm (Figure 6).
Figure 5: Ultrasound and fluoroscopic-guided percutaneous transhepatic liver abscess drainage through drain placement. A) The first attempt of drainage with catheter/pigtail insertion. B) The first attempt of drainage percutaneously.
Figure 6: Abdominal CT for liver abscess drainage assessment. The green arrow points to the hepatic abscess. A, B) Sagittal views. C) Coronal view. D, E) Axial views.
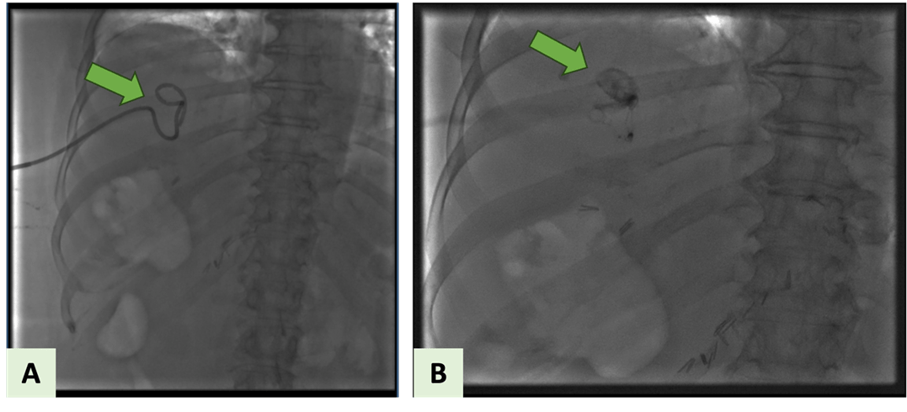
The patient was discharged home after the second ultrasound and fluoroscopic-guided percutaneous transhepatic liver abscess drainage procedure, on day 13 of the hospital stay. Upon her follow-up in the surgical outpatient clinic, the right hepatic drain that was placed for hepatic abscess was checked by an abscessogram weekly. The patient’s last follow-up visit showed no significant fluid drainage and drain removal was planned (Figure 7). As a result, the pigtail removal, resulted in an uneventful pull-back tractogram and right hepatic abscess lobe drain removal.
Figure 7: Image-guided drain removal.
Discussion
Globally, RYGB has rapidly become one of the bariatric interventions that patients with various levels of obesity undergo [1]. Gastric strictures, gastric hemorrhage, and/or leaks from the staple line represent three serious complications that might originate from RYGB [2]. Hepatic abscess formation is an extremely rare complication following bariatric surgeries such as RYGB operations [2]. The clinical manifestations of gastric leakage are abscesses, peritonitis, fistulas, sepsis, and organ failure. In splenic and liver abscesses, abdominal pain and fever are the common presenting features [2]. Our patient presented with diffuse abdominal pain on postoperative day 23 of RYGB.
Liver abscesses are classified mostly into pyogenic, or amoebic, and to a lesser extent into parasitic types [4]. The pyogenic type of liver abscess resulted from bacteria-related infections of the liver parenchyma that involve inflammation and pus formation. The typical sequence of abscess development involves intestinal leaking into the abdominal cavity and passage through the portal vein to the liver [4]. About 5% to 15% of these liver infections can be triggered by bacterial inoculation of the liver tissue via the hepatic artery or by direct drainage system of the portal vein [4, 5]. In 5%-10% and 1%-5% of instances, direct expansion from an adjacent site of infection and traumatic incidents, respectively, are thought to be the sources of infection [3, 6]. The pathogen can penetrate the liver either directly through proximity or via bile duct channels [4, 6, 7].
To diagnose pyogenic hepatic abscesses, radiological investigations are crucial [4, 6, 8]. These include contrast-enhanced CT scans and ultrasonography with a sensitivity level of 98% [4, 6]. The main contrast-enhanced CT radiological findings are identified as low-attenuation, circular masses with an augmenting peripheral rim [4]. In the presented case, numerous CTs with IV contrast of the chest, abdomen, and pelvis were carried out following admission, and each percutaneous drainage for assessment and the findings were previously mentioned in the case presentation section. The percutaneous image-guided drainage of the abscess is an effective safe alternative to surgical technique. This procedure involves percutaneous evacuation with or without catheter insertion [4, 8, 9]. Typically, the main treatment approach for a liver abscess is percutaneous drainage in conjunction with antimicrobial therapy [1, 4, 8]. The minimally invasive procedure in the current case was the ultrasound and fluoroscopic-guided percutaneous transhepatic liver abscess drainage through pigtail placement. The patient’s response was evaluated by clinical improvement and repeated abdominal CTs.
However, if percutaneous drainage is unsuccessful or therapy of a coexisting intra-abdominal condition is required, surgery may be indicated [4, 8, 9]. There are two possible explanations for the liver abscess formation [4]. The primary explanation includes the bacterial migration to the liver parenchyma through the staple line leakage [1, 4, 7]. Secondarily to leak-related accumulation, pylephlebitis of the porto-mesenteric veins results, triggering the ascending bacterial relocation from the portal venous system [4].
In the literature, one case reported an incidence of recurring perihepatic abscesses caused by a gastric fistula after a Roux-en-Y gastric bypass procedure [5]. To our knowledge, this is the first case to be reported of a pyogenic liver abscess following the RYGB procedure.
Conclusion
Despite the fatality and rarity of pyogenic liver abscesses post-RYGB, they should be considered in bariatric surgery complications. Radiological studies aid in the identification and diagnosis of intra-abdominal abscesses, especially pyogenic liver abscesses. To cure such cases, percutaneous image-guided drainage of the abscess is a viable treatment option. Our case highlights an extremely rare Roux-en-Y gastric bypass complication caused by a leaky and/or infectious hematoma that eventually led to peritonitis and hepatic abscess.
Conflicts of Interest
None.
Funding
None.
Ethical Approval
Not applicable.
Consent
Written informed consent was obtained from the patient to publish this case report and accompanying images. On request, a copy of the written consent is available for review by the Editor-in-Chief of this journal.
Author Contributions
Athary Saleem: Literature review, paper writing, and editing, picture editing, and manuscript drafting. Saqer Alenezi: Paper writing, and editing. Nimer Al-Shadidi: Performed surgery, and paper editing. Khaleel Mohammad: Performed surgery, critical review, supervision, and final approval.
Guarantor
Athary Saleem, D.Pharma., B.Med.Sc., M.D., General Surgery department, Al-Adan Hospital, Kuwait.
Research Registration
Not applicable.
Provenance and Peer Review
Not commissioned, externally peer-reviewed.
Article Info
Article Type
Case Report and Review of the LiteraturePublication history
Received: Mon 26, Feb 2024Accepted: Mon 18, Mar 2024
Published: Wed 03, Apr 2024
Copyright
© 2023 Athary Saleem. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.AJSCR.2024.01.03
Author Info
Athary Saleem Saqer Alenezi Nimer Al-Shadidi Khaleel Mohammad
Corresponding Author
Athary SaleemNeurosurgery Department, Jaber Al Ahmad Hospital, State of Kuwait
Figures & Tables
Table 1: Patient’s vital
signs and laboratory investigations on admission
|
Patient’s vital signs |
Hematology |
Clinical Chemistry |
|
GCS 15/15 |
WBC 31.8 |
Amylase 16 |
|
BP
121/62 mmHg |
Hb 126 |
Lipase 14 |
|
HR 110 bpm |
Platelets 287 |
Total Bilirubin 27.4 |
|
RR 20 bpm |
Neutrophils 28.60 |
Direct Bilirubin 13.8 |
|
SPO2 99 % on room air |
Lymphocytes 1.79 |
Indirect Bilirubin 14 |
|
Body temperature 39.5 o C |
Monocytes 1.36 |
Albumin 26.4 |
|
|
Eosinophils 0.00 |
ALT 208 |
|
|
PT 27.3 |
AST 286 |
|
|
|
ALP 184 |
|
|
|
Creatinine 56 |
References
1. Kaba A, Odufalu FD,
Ahmed Z, Prather C, Nazzal M (2021) Recurrent perihepatic abscesses arising
from a gastric remnant leak: delayed complication of a revision roux-en-Y
gastric bypass. Case Rep Surg 2021: 5510526. [Crossref]
2. Blachar A, Federle
MP (2002) Gastrointestinal complications of laparoscopic Roux-en-Y gastric
bypass surgery in patients who are morbidly obese: findings on radiography and
CT. AJR Am J Roentgenol 179: 1437-1442. [Crossref]
3. Sohrabi C, Mathew
G, Maria N, Kerwan A, Franchi T et al. (2023) The SCARE 2023 guideline:
updating consensus Surgical CAse REport (SCARE) guidelines. Int J Surg
109: 1136-1140. [Crossref]
4. Al Faris H, Al
Aqeel M, Hazza AO, Abou Yassine W, Al Qurashi A (2020) Pyogenic liver abscess
post sleeve gastrectomy complicated by leak: a case report and literature
review. Ann Clin Case Rep 5: 1798.
5. Chakhachiro D, Al
Armashi AR, Bawwab A, Alsallamin I, Homeida M et al. (2022) Pyogenic Hepatic
Abscess: A Case Report and Literature Review on a Rare Complication of Gastric
Sleeve Surgery. Cureus 14: e22650. [Crossref]
6. Tsai MS, Lin CL,
Jeng LB (2016) Gastrectomy is associated with an increased risk of pyogenic
liver abscess: a 13-year nationwide cohort study. Sci Rep 6: 33788. [Crossref]
7. Czerwonko ME,
Huespe P, Elizondo CM, Pekolj J, Gadano A et al. (2018) Risk factors and
outcomes of pyogenic liver abscess in adult liver recipients: a matched
case-control study. HPB (Oxford) 20: 583-590. [Crossref]
8. Serraino C, Elia C, Bracco C, Rinaldi G, Pomero F et al. (2018) Characteristics and management of pyogenic liver abscess: A European experience. Medicine (Baltimore) 97: e0628. [Crossref]
9. Garrido D, Bush LM (2013) Liver abscess as a complication of laparoscopic gastric banding bariatric surgery. Surg Infect (Larchmt) 14: 464-469. [Crossref]
