Pseudotumoral Calcinosis: A Soft Tissue Tumor in a 14-Year-Old Male
A B S T R A C T
Pseudotumoral calcinosis is a rare benign tumor, characterized by deep calcium deposition in peri-articular soft tissues. A numerous list of calcium deposit diseases exists making the calcinosis diagnosis very challenging. There are three principal forms or etiologies; primary or idiopathic forms followed by secondary forms due to chronic renal failure or hyperparathyroidism, then genetic forms such as Hyperphosphatemic Familial Tumoral Calcinosis (HFTC). We report a case of 14-year-old boy with primary tumoral calcinosis of the right hip. Total mass resection was performed without any recurrence at one-year follow-up.
Keywords
Primary tumoral calcinosis, soft tissue mass, child
Introduction
Pseudotumoral calcinosis is an uncommon and benign condition that generally occurs as a complication of microtrauma or renal dialysis, rarely as a genetic form occurring essentially in tropical and subtropical African regions. This periarticular tumor-like is frequently associated with hyperphosphatemia, that is manifested by the sedimentation of calcium particles around major joints. Surgical excision is the main treatment. The aim of this article is to describe this rare tumor in his epidemiologic, clinic, radiographic and histopathologic aspects.
Case Presentation
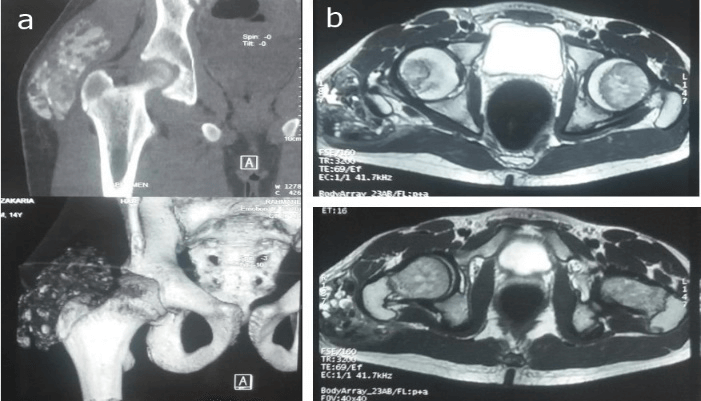
The case involved a 14-year-old male without any personal or familial diseases, was worried by swelling around his right hip progressing during one-year, clinical exam noted a painless masse measuring about 5 cm long and 3 cm wide movable without any inflammatory signs (Figure 1). Pelvis radiography and CT-scan displayed a huge popcorn-like calcified mass around the right hip, which was extraskeletal (Figure 2). MRI images showed a calcified lesion close to the right greater trochanter with a low intensity in T1, and heterogeneous characteristics in T2- weighted sequences (Figure 3). We have found a slight hyperphosphatemia with normal blood test levels of calcium, alkaline phosphatase, parathyroid hormone and renal function.
Therefore, surgical biopsy and resection was decided through direct longitudinal approach, it was a lesion containing granular and sandy constituents in a fluid milky-like substance which was completely aspirate for histopathologic study which confirmed a diagnosis of calcinosis without any malignancy, it was composed of large cystic areas with multiple calcified deposits surrounded by mononuclear and giant cells (Figure 4). Post-operative radiographs showed complete elimination of the calcified deposits with good clinical and esthetic results. Phosphate-restricted diet was prescribed, and patient was checked regularly clinically and by imaging without detection of any recurrence after one-year follow-up.
Figure 1: Clinical view showing the right hip swelling.
Figure 2: pelvis anteroposterior X-rays, showing a popcorn-like ossified lesion in the soft tissues of the right peritrochanteric region (arrow).
Figure 3: a) CT scan and b) Axial MRI of the pelvic, showing the calcified mass in the right peritrochanteric region.
Figure 4: Operative view of the lesion that was liquid with withe granulations (arrow).
Discussion
Pseudo-tumoral calcinosis is a rare benign tumor, it was first described by Inclan in 1943. It is characterized by calcium deposit in periarticular soft tissues, frequently located in the para-articular regions of the hip as in our case, followed by shoulder then elbow and ankle, it can be solitary or multiple. It affects young patients between the first and second decade without predominance of sex, furthermore, black race seems more exposed [1]. The exact mechanism is less clear, microtraumas seem to be a risk factors in primary or idiopathic forms via inadequate reparative response like sleeping on hard plan affecting gluteal region or elbow. Moreover, chronic renal failure or hyperparathyroidism are causes of secondary forms. However, familial or genetic forms are less frequent, they are characterized by genetic mutations affecting enzymatic and metabolic function, the most known disease is the Hyperphosphatemic Familial Tumoral Calcinosis (HFTC) [2].
Biologic investigation can show normal or frequently elevated phosphate and vitamin D, but normal calcium, renal function and parathormone blood levels [3, 4]. Plain radiographs reveal clearly the ossified mass also CT-scan are very helpful to detect calcifications even if they are not yet radiopaque. Whereas magnetic resonance imaging (MRI) is highly efficient, it shows ossification with a low signal intensity on T1 and T2-weighted sequences, otherwise it identifies anatomic extent of the lesion and eliminate any malignity [5, 6]. Most often preoperative finding is not always clear essentially if blood tests are normal, until the surgical biopsy and histopathologic analyze that confirm the diagnosis and exclude any malignancy, as calcifications occurs in various tumoral aspects, including benign lesions, such as myositis ossificans, calcinosis in juvenile dermatomyositis, osteolipoma and tophaceous, or malign tumors essentially osteosarcoma, chondrosarcoma or soft tissue sarcomas [7-9]. Complete surgical removal of the masses is the treatment of choice; however, other therapeutic option exists, they are common to other calcium deposits diseases involving low-calcium and low-phosphorus diet associated to oral doses of aluminum hydroxide [10].
Conclusion
Pseudotumoral calcinosis are rare benign lesions, usually located around trochanteric, shoulder and elbow region and have a slow growth asymptomatic evolution. Explorations are necessary to reduce numbers of differential diagnosis essentially sarcoma before the reassurance of histopathologic examination.
Conflicts of Interest
None.
Consent
Consent was obtained from the parents.
Funding
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 29, Apr 2020Accepted: Tue 12, May 2020
Published: Thu 14, May 2020
Copyright
© 2023 Abderr Rahim. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2020.02.11
Author Info
Abdelouahed Amrani Abderr Rahim Badr Rouijel Imane Zizi Mohammed Anouar Dendane Omar Dellero Tarik El Madhi Zakariya Aboulam Zouhir F El Alami
Corresponding Author
Abderr RahimResident at Department of Orthopaedic Surgery & Traumatology II, Mohamed V Military Hospital, Faculty of Medicine and pharmacy, Mohamed V University, Rabat, Morocco
Figures & Tables



References
- Inclan N, Leon P, Comejo MG (1945) Tumoral calcinosis. JAMA 121: 490-495.
- Topaz O, Shurman DL, Bergman R, Indelman M, Ratajczak P et al. (2004) Mutations in GALNT3, encoding a protein involved in O-linked glycosylation, cause familial tumoral calcinosis. Nat Genet 36: 579-581. [Crossref]
- Katsumi Suzuki, Sadao Takahashi, Kenzo Ito, Yoichi Tanaka & Yoshinori Sezai (1979) Tumoral Calcinosis in a Patient Undergoing Hemodialysis. Acta Orthopaedica Scandinavica 50: 27-31.
- Seyahi A, Atalar AC, Ergin HK (2006) Tumoral calcinosis: Clinical and biochemical aspects of a patient treated with vinpocetine. Eur J Intern Med 17: 436-438. [Crossref]
- Olsen KM, Chew FS (2006) Tumoral calcinosis: pearls, polemics, and alternative possibilities. Radiographics 26: 871-885. [Crossref]
- Ibrahim Fathi Mahmoud Sakr (2014) Review of tumoral calcinosis: A rare clinic-pathological entity. World J Clin Cases 2: 409-414. [Crossref]
- Sadiq M, Nayak M, Farheen A, Digge V (2019) An Unusual Case of Huge Tophaceous Pseudogout Mimicking as a Tumor-Like Lesion around the Ankle Joint: A Case Report and Literature Review. Case Rep Orthop 2019: 9617184. [Crossref]
- Pestcavage JM, Richardson ML (2009) Tumoral calcinosis mimicking recurrent osteosarcoma. Radiol Case Rep 4: 336. [Crossref]
- Slavin RE, Wen J, Barmada A (2012) Tumoral calcinosis - a pathogenetic overview: a histological and ultrastructural study with a report of two new cases, one in infancy. Int J Surg Pathol 20: 462-473. [Crossref]
- Dima A, Balanescu P, Baicus C (2014) Pharmacological treatment in calcinosis cutis associated with connective-tissue diseases. Rom J Intern Med 52: 55-67. [Crossref]
