Primary Retroperitoneal Serous Cystadenoma Mimicking Rectal Duplication Cyst: A Case Report
A B S T R A C T
Background: Primary retroperitoneal serous cystadenomas (PRSCs) are extremely rare, and their pathogenesis is not well understood. Differentiating these tumors from other cystic or tumorigenic lesions can be challenging given the unusual retroperitoneal location and varied symptomatology.
Case Presentation: An 83-year-old female was evaluated for vaginal prolapse symptoms, fecal incontinence, and intermittent mixed urinary incontinence symptoms. Magnetic resonance imaging showed a large space-occupying cystic structure closely associated with the rectum. After exploratory laparotomy with excision of the retroperitoneal mass, biopsy showed a simple cyst filled with serous fluid and lined by a single layer of cuboidal epithelial cells consistent with serous cystadenoma. On follow up visit, she reported improvement in stress urinary incontinence, but continued to have difficulty with urinary and bowel urge incontinence.
Conclusion: PRSCs should be considered during evaluation of retroperitoneal space-occupying lesions despite the rarity of serous cystadenomas being found in this location. The pathophysiology of how PRSCs arise is still not well understood but establishing better techniques to distinguish these lesions from other cystic and tumorigenic lesions should be investigated.
Background
Benign serous cystadenomas account for approximately 25% of all benign ovarian tumors [1]. However, primary retroperitoneal serous cystadenomas (PRSCs) are extremely rare, and their pathogenesis is not well understood. Serous cystadenomas are typically large, unilocular, and contain a cyst wall comprised of a single layer of cuboid epithelium. The epithelial cells are composed of glycogen-rich epithelium that form small cysts containing serous fluid. They most likely arise from the invagination of the ovarian surface epithelium and are commonly seen in patients in the fourth or fifth decades of life. Cases with atypical presentations and features can mimic malignant neoplasms and pose a challenge diagnostically. Additionally, lesions with similar presentations that are usually benign have shown to undergo malignant transformation in some cases. These include developed large masses that compress and disfigure adjacent organs often cause mass-effect symptomatology which can vary greatly. Differentiating cystadenomas from other large, potentially malignant tumors is crucial. Definitive diagnoses require biopsy and pathologic evaluation to determine the cell type lining the cysts [1-3]. In our report, we describe a case of primary retroperitoneal serous cystadenoma that was mimicking rectal duplication cyst on imaging.
Case Report
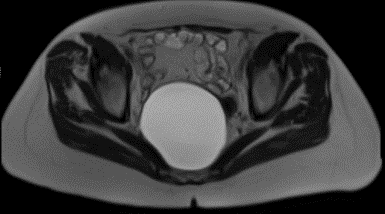
An 83-year-old female gravida 4 para 4 (all vaginal deliveries) with a history of breast cancer and a known pelvic mass status post ovary-sparing abdominal hysterectomy who presented to our clinic with symptoms of mixed urinary incontinence, vaginal prolapse, and fecal incontinence. On presentation, our patient reported that she was experiencing a sensation of vaginal bulging as well as symptoms of both urge and stress urinary incontinence multiple times weekly for the past several years. In terms of fecal incontinence, she reported a frequency of approximately one episode per month. She also endorsed chronic right-sided flank pain. The patient stated that she first learned of a 10 cm pelvic mass in 2010 when she was diagnosed with acute appendicitis, but it was never followed up. Her physical examination was remarkable for a grade 3 cystocele and grade 2 vaginal vault prolapse with no evidence of an associated rectocele. Bimanual examination revealed a mass in the right adnexal region. Initial workup included an MRI of the pelvis without contrast which revealed a 9.1 x 9.5 x 12.4 cm (previously 3.6 x 5.2 x 6.0 cm) lesion extending from S1 to the tip of the coccyx without soft tissue or enhancing components, and global pelvic floor instability including a moderate to severe cystocele, moderate vaginocele, and small rectocele.
The lesion appeared benign and there was no associated adenopathy. At this time, diagnostic considerations consisted of a rectal duplication cyst and a tailgut cyst as the mass clearly appeared cystic and well defined and did not seem to be invading the rectum. The patient subsequently underwent an open sacral colpopexy with mesh, transvaginal placement of urethral sling, and removal of the pelvic mass. Intraoperatively, the cyst was found in the retroperitoneum, displacing the distal sigmoid colon and rectum anteriorly.
Pathological evaluation revealed a simple cyst filled with serous fluid and lined by a single layer of cuboidal epithelial cells. The morphology of the epithelium and the size of the cyst were consistent with a serous cystadenoma. Her post-operative course was complicated by an episode of atrial fibrillation with a heart rate in the 140s and associated shortness of breath that responded to IV labetalol on post-operative day 3.
Due to high concern for pulmonary embolism, a spiral CT thorax with contrast was obtained and confirmed an acute pulmonary embolism in a segmental artery of the left upper lobe. She was started on therapeutic Lovenox and transitioned to Warfarin the following day. Additionally, the patient reported groin pain and difficulty raising her left leg for which neurosurgery and orthopedic surgery recommended outpatient physical therapy. Approximately one month following the surgery, the patient reported improvement in stress urinary incontinence, but continued to have difficulty with urinary and bowel urge incontinence.
Discussion
Several differential diagnoses should be considered in patients who present with retroperitoneal masses, including but not limited to soft tissue sarcoma, rectal duplication cyst, tailgut cyst, cystadenoma, retroperitoneal fibrosis, and lymphoma [4]. Diagnostic considerations for this patient’s mass primarily being considered at the time of excision included rectal duplication cyst and tailgut cyst. A rectal duplication cyst (RDC) was the leading diagnosis and is usually a rare developmental anomaly that makes up < 5% of all duplication cysts developing in the gastrointestinal tract. RDCs typically present in childhood, and fewer than 30% of all duplications are diagnosed in adults. Cases of adult RDC have been reported, primarily in middle-aged women with a 3:1 female to male ratio.
These typically present with symptoms of mass effect, local infection, bleeding, fistulization, or rarely malignant transformation. Diagnosis can be facilitated by criteria of Ladd including 1) cyst close to or in continuity with the rectum, 2) cyst having smooth muscle cover, 3) cyst covered by mucosa found in the gastrointestinal tract. MRI evidence of RDCs generally shows intracystic fluid with heterogeneous signal density on T1 weight images and homogenous high signal intensity on T2 weight imaging [5, 6]. History and physical exam alone in this case were unreliable for differentiating between PRSC and a space-occupying RDC. There are no history or physical exam findings specific for PRSCs, but nonspecific symptoms of abdominal fullness, pain, fatigue, weight loss are common. Our patient’s symptoms of urinary and fecal incontinence could have been attributed to either a PRSC or a RDC due to the mass effect the lesion had on surrounding anatomy. In conjunction with uncharacteristic demographics for RDC, imaging helped us to differentiate PRSC from RDC. This patient’s pre-operative MRI revealed a homogeneous cystic lesion in close proximity to the rectum, but the lack of smooth muscle lining suggested an alternative diagnosis.
Tailgut cysts (also known as retrorectal cystic hamartomas) are another uncommon type of congenital cysts that mainly occupy the presacral space. These most commonly occur in women in the 5th decade of life and are a source of chronic perirectal and perianal symptomatology including constipation, diarrhea, pain, urinary obstruction, back pain, lower limb neuropathy from compression of the sacral plexus, or urinary obstruction. Tailgut cysts were considered lower on the differential due to the absence of perirectal or perianal pain or lower limb neuropathy. Tailgut cyst MRI studies demonstrate unilocular or multilocular cystic appearances and usually have low signal intensity on T1-weighted images and high signal intensity on T2 weighted images. Frequently, the presence of small cysts clustered together adjacent to the main cyst can also be seen resulting in a honeycomb pattern. Therefore, the presence of a large unilocular cyst, as in this patient, makes a tailgate cyst less likely.
Figure 1: Magnetic Resonance Imaging showing 9.1 x 9.5 x 12.4 cm presacral cyst without soft tissue enhancing components in sagittal plane.
Figure 2: Axial View.
Similar to RDC, tailgut cysts have been reported to undergo malignant transformation to adenocarcinoma, carcinoid, and sarcoma, but only at a malignant rate of transformation of 2% in the largest literature study. Some reports have suggested malignant transformation rates of up to 40% but are limited by their small-scale. Pathologically, tailgut cysts must be lined with intestinal type epithelium and muscular or serosal coating based on their description by Peyron in 1928. Cysts may contain columnar, squamous, cuboidal or transitional epithelium with columnar epithelium making up the majority of histologic appearances [7]. Conflicting symptomatology and imaging studies suggested against the diagnosis of a tailgut cyst, and surgical resection allowed for the ultimate diagnosis of PRSC.
Regardless, management of PRSC, RDC, or tailgut cysts involves surgical excision and pathologic evaluation. Surgical excision is curative and prevents complications including malignant degeneration. While PRSCs have not been reported to undergo malignant transformation, their excision and pathologic evaluation should be performed due to the inability to differentiate these lesions from other space occupying lesions of the pelvis based on history, physical exam, laboratory, or imaging findings alone.
Conclusion
The diagnosis of PRSC requires surgical excision and evaluation of histologic features. A wide variety of benign and malignant space occupying lesions can present in the pelvic region and cause similar symptomatology seen in our patient. Despite the rarity of PRSCs, prompt evaluation and surgical intervention are warranted to minimize the risk of malignant transformation and invasion into adjacent structures. Better techniques to differentiate and classify these lesions should be investigated in order to better understand the pathophysiology of their formation and risk of transformation into invasive disease.
Acknowledgements
We would like to thank the patients without whom this work would not be possible.
Conflicts of Interest
None.
Funding
The authors have no financial or proprietary interest in the subject matter or materials discussed in the manuscript. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Article Info
Article Type
Case ReportPublication history
Received: Fri 03, Jan 2020Accepted: Sat 01, Feb 2020
Published: Mon 10, Feb 2020
Copyright
© 2023 Valentine Nfonsam. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.COR.2020.01.10
Author Info
Hunter Jecius Mary Junak Mohammad Hamidi Valentine Nfonsam
Corresponding Author
Valentine NfonsamDepartment of General Surgery, The University of Arizona, Tucson, Arizona, USA
Figures & Tables

References
- Boyle K, Torrealday S (2008) Benign Gynecologic Conditions. Surg Clin North Am 88: 245-264. [Crossref]
- LC Chu, AD Singhi, RR Haroun, RH Hruban, EK Fishman (2017) The many faces of pancreatic serous cystadenoma: Radiologic and pathologic correlation. Diagn Interv Imaging 98: 191-202. [Crossref]
- Mori A, Changela K, Alhankawi D, Itskovich A, Butt A et al. (2017) A Giant Primary Retroperitoneal Serous Cystadenoma: Case Report and Review of Retroperitoneal Cysts. Surg J (N Y) 3: e32-e37. [Crossref]
- Mota MMDS, Bezerra ROF, Garcia MRT (2018) Practical approach to primary retroperitoneal masses in adults. Radiol Bras 51: 391-400. [Crossref]
- Bashaer A, Faucheron JL (2015) Rectal duplication responsible for compressive symptoms is a very rare entity in adults. Tech Coloproctol 19: 561-562. [Crossref]
- Sharma S, Yadav A K, Mandal A K, Zaheer S, Yadav D K et al. (2015) Enteric Duplication Cysts in Children: A Clinicopathological Dilemma. J clin Diagn Res 9: EC08-EC11. [Crossref]
- Patsouras D, Pawa N, Osmani H, Phillips R K (2015) Management of tailgut cysts in a tertiary referral centre: a 10‐year experience. Colorectal Dis 17: 724-729. [Crossref]
