Physiotherapy Management of a Middle-Aged Adult Male with Severe Symptoms of Coronavirus Disease-19: A Case Report
A B S T R A C T
Coronavirus disease-19 (COVID-19) has affected people of various age groups with symptoms ranging from asymptomatic or mild to severe respiratory failure, with mild symptoms requiring little or no medical intervention whereas severe symptoms requiring hospitalisation and prompt medical management. The following case report illustrates about recovery of a patient with severe symptoms of COVID-19 in a COVID dedicated tertiary care hospital run by the Municipal Corporation of Greater Mumbai. Physiotherapy has long been a part of multidisciplinary team in management of patients with severe respiratory illnesses. The report mainly presents about the Physiotherapy management undertaken for the above-mentioned patient parallelly to the Medical management aiding in recovery of the patient.
Keywords
Coronavirus, COVID-19, symptoms, physiotherapy, case report
Introduction
Severe Acute Respiratory Syndrome coronavirus 2 (SARS-CoV-2) causes the novel Coronavirus disease- 2019 (COVID-19), first case of which was reported in December 2019 in Wuhan city, China. SARS-CoV-2 seems to be highly contagious as it is transmitted human to human even when the infected person is asymptomatic and thus has spread quickly all over the world [1, 2]. Person to person transmission is mainly through respiratory secretions in the form of aerosols generated during coughing, sneezing and speaking. These aerosols may remain suspended in the air upto 3 hours and inhaled by nearby person or deposit on the mucosal membranes of the eyes, or land within 2 meters and contaminate surfaces which become fomites and infect a person if the person touches his/her eyes, mouth and nose after touching such surfaces [2].
Typical presentations in individuals with COVID-19 after 2-14 days of exposure to the virus may present with variety of symptoms including fever/chills (89%), cough (68%), fatigue (38%), sputum production (34%), dyspnea (19%), muscle/ body aches, headache, new loss of taste or smell, sore throat, congestion/runny nose, nausea/vomiting, diarrhoea. Also, there may be renal, gastrointestinal, liver, cardiac, neurological and hematological dysfunctions/abnormalities present. The severity of COVID-19 disease ranges from asymptomatic individuals and mild upper respiratory tract infection to severe viral infection causing pneumonia leading to respiratory failure and/or death [2-4]. Government of India Ministry of Health & Family Welfare Directorate General of Health Services (EMR Division): Revised Guidelines on Clinical Management of COVID-19 dated 31st March 2020 mentions an individual as a severe case who has pneumonia with hypoxaemia (SpO2< 92%) [5].
Physiotherapy is an integral part of the ICU team supporting the holistic treatment of patients with non-invasive treatment modalities mainly involving postural changes, breathing exercises, limb mobilization, relaxation exercises, ambulation of patients and weaning off ventilator support trials [6].
Case Presentation
A 45-year-old male, General store shopkeeper by occupation, with no known history of exposure to COVID-19 patient, came with complains of fever, breathlessness (mMRC Grade 4), dry cough, palpitations, fatigue and giddiness on standing since 2 days [7]. On general examination, he was afebrile, with pulse rate 120/min and blood pressure 130/80 mm Hg. On auscultation, air entry was bilaterally equal with no foreign sounds. Physical examination revealed tachypnoea (30 breaths/minute) and increased work of breathing (use of accessory inspiratory muscles). His RT-PCR test for COVID-19 came out positive on 10th June 2020 after which he was hospitalized in COVID dedicated Tertiary Care Hospital in Mumbai. At the time of admission his SPO2 was 45% on room air which improved to 80% on giving O2 (8L/min). He was admitted in the COVID dedicated High Dependency Unit established beside the ICU and was put on BiPAP ventilator mode with Fi02 100%. Investigations performed are mentioned in (Table 1). ABG reports are presented in (Table 2).
Table 1: Investigations.
|
Investigations |
Values/Findings |
Interpretation |
|
Haemoglobin |
12.0 g/dl |
Borderline normal |
|
ECG |
Heart rate: 87 beats per minute, Premature Ventricular Contractions observed in V5, V6 and was suggestive of Left Axis Deviation. |
Suggestive of Left Axis Deviation. |
|
Ferritin |
1265 ng/ml |
Increased |
|
Interleukin-6 |
210 pg/ml |
Increased |
|
D-Dimer |
11.1 μg/ml |
Increased |
|
RT-PCR(10/06/2020) (Before hospitalisation) |
Positive |
COVID positive |
|
RT-PCR(15/06/2020) (3 days of hospitalisation) |
Positive |
COVID positive |
|
RT-PCR(29/06/2020) (2 weeks after hospitalisation) |
Negative |
COVID negative |
Table 2: Laboratory reports of ABG Analysis from the date of admission.
|
Date |
13/06/2020 |
16/06/2020 |
17/06/2020 |
18/06/2020 |
21/06/2020 |
|
Day of admission |
1st day |
4th day |
5th day |
6th day |
9th day |
|
O2 status |
BiPAP 100% |
BMV 15L/min |
BMV 15L/min |
BMV 15L/min |
BMV 15L/min |
|
pH |
7.497 |
7.467 |
7.314 |
7.389 |
7.384 |
|
PCO2 (mmHg) |
28.1 |
25.4 |
27 |
34.6 |
44.9 |
|
HCO3 (mmol/L) |
23.2 |
21.2 |
15.3 |
21.3 |
24.8 |
|
PO2 (mmHg) |
45.8 |
53.9 |
55.8 |
71.1 |
117 |
|
SPO2 (%) |
85.7 |
89.5 |
84.3 |
93.7 |
98 |
|
PaO2/FiO2 |
45.8 |
81.67 |
84.55 |
107.73 |
177 |
|
Date |
22/06/2020 |
23/06/2020 |
24/06/2020 |
27/06/2020 |
30/06/2020 |
|
Day of admission |
10th day |
11th day |
12th day |
15th day |
18th day |
|
O2 status |
BMV 15L/min |
BMV 15L/min |
BMV 10L/min |
BMV 8L/min |
BMV 10L/min |
|
pH |
7.411 |
7.417 |
7.436 |
7.443 |
7.434 |
|
PCO2 (mmHg) |
44.4 |
44.6 |
42 |
33 |
38.5 |
|
HCO3 (mmol/L) |
26.3 |
28 |
27.8 |
22.1 |
25.2 |
|
PO2 (mmHg) |
140.1 |
141.1 |
191 |
115.2 |
122 |
|
SPO2 (%) |
99.2 |
99.2 |
99.3 |
98.4 |
98.9 |
|
PaO2/FiO2 |
212 |
213.79 |
374.51 |
256 |
239.22 |
The patient was referred for Physiotherapy on 17th June 2020 (5th day after admission) complaining of breathlessness and dry cough and was on Bag Mask Ventilation (BMV) 15 L/min with ongoing weaning trials. Patient was conscious, co-operative and well oriented to time, place and person. Patient was on medical management as prescribed by the treating doctor which included revival with BiPAP support followed by Bag and Mask ventilation (O2 status in (Table 3)) and medications mainly including Inj. Piptaz (Broad spectrum antibiotics), Inj. Low Molecular Weight Heparin (anticoagulant), Inj. Methylprednisolone (immunosuppressant) and Inj. Tocilizumab (IL-6 inhibitor: immunosuppressant). Prior to Physiotherapy treatment, patient’s vitals were checked mainly temperature, blood pressure, pulse rate and oxygen saturation on supplemental oxygen support. When all vital parameters were in normal range only then physiotherapy treatment was given presented in (Table 3). Our expected outcome was early weaning from oxygen support, early recovery and independence in Activities of daily living which was achieved during the hospitalization period.
Table 3: Change in vital parameters with inpatient supervised physiotherapy management.
|
Date |
17th June |
18th June |
19th June |
20th June |
22nd June |
23rd June |
24th June |
|||||||||
|
Physiotherapy treatment day |
Day 1 |
Day 2 |
Day 3 |
Day 4 |
Day 5 |
Day 6 |
Day 7 |
|||||||||
|
O2 Supply(L/min) |
BiPAP; FiO2: 100% |
BMV 15L |
BMV 15L |
BMV 15L |
BMV 15L |
BMV 15L |
BMV 10L |
|||||||||
|
Pulse Rate (bpm) |
Pre |
85 |
85 |
87 |
85 |
90 |
90 |
103 |
||||||||
|
Post |
88 |
90 |
88 |
113 |
110 |
112 |
110 |
|||||||||
|
SPO2 (%) |
Pre |
96 |
95 |
97 |
99 |
97 |
100 |
99 |
||||||||
|
Post |
97 |
99 |
97 |
98 |
100 |
100 |
96 |
|||||||||
|
Positioning (side lying) |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Prone lying |
|
|
|
|
Y |
Y |
Y |
|||||||||
|
Breathing Exercises |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
In bed exercise |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Sitting exercises |
|
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Standing |
|
|
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Balance exercises in Standing |
|
|
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Spot Marching |
|
|
|
Y |
Y |
Y |
Y |
|||||||||
|
Walking |
|
|
|
|
Y |
Y |
Y |
|||||||||
|
Date |
25th June |
26th June |
27th June |
29th June |
30th June |
1st July |
2nd July |
|||||||||
|
Physiotherapy treatment day |
Day 8 |
Day 9 |
Day 10 |
Day 11 |
Day 12 |
Day 13 |
Day 14 |
|||||||||
|
O2 Supply(L/min) |
BMV 10L |
BMV 10L |
BMV 8L |
BMV 6L |
BMV 6L |
Nasal prongs 2L |
Nasal prongs 2L |
|||||||||
|
Pulse Rate (bpm) |
Pre |
98 |
96 |
88 |
112 |
108 |
102 |
112 |
||||||||
|
Post |
105 |
102 |
102 |
120 |
116 |
112 |
120 |
|||||||||
|
SPO2 (%) |
Pre |
100 |
100 |
100 |
99 |
98 |
97 |
98 |
||||||||
|
Post |
95 |
99 |
100 |
98 |
99 |
99 |
95 |
|||||||||
|
Positioning (side lying) |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Prone lying |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Breathing Exercises |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
In bed exercise |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Sitting exercises |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Standing |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Balance exercises in Standing |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Spot Marching |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Walking |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
Y: represents exercise was given on that day; BiPAP: Bilevel Positive Airway Pressure; BMV: Bag Mask Ventilation, L/min: litres/ minute, SPO2: Saturation of peripheral oxygen.
Discussion
COVID-19 caused by SARS-CoV-2 is a novel disease which had emerged in December 2019 in China has now spread rapidly all over the world infecting over 12 million people and has resulted in death of over half a million people (as on 8th July 2020). Since it is novel, literature on the disease and guidelines regarding its modes of transmission, safety precautions, management etc. are constantly being updated as more and more knowledge is being shared globally. There is no definitive treatment for COVID-19 yet, with management mainly focused on symptomatic treatment and development of vaccine seems far. Continuous bombardment with negative news regarding increasing rate of infections and deaths every day, also circulation of controversial messages and videos through various media regarding affected people being taken away forcefully to isolation centres or hospitals and showing lack of resources and pile up of dead bodies at those places has led to heightened anxiety, panic and fear among the common people. This has reduced the faith of common people in the health care system and has also developed social stigma and taboo against the people affected and even recovered with COVID-19.
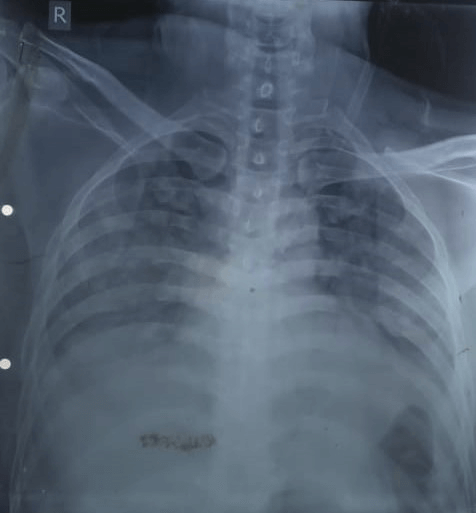
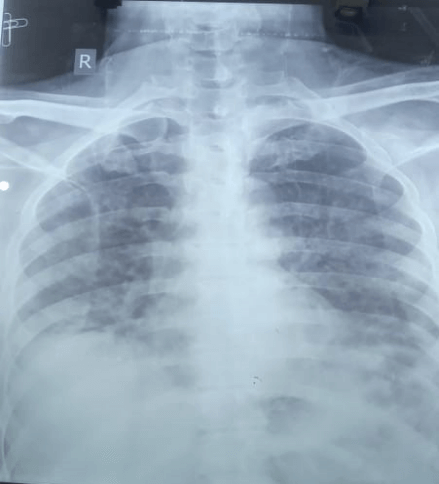
There are increased incidents of people not co-operating with the health care workers and hiding their mild symptoms to avoid going to isolation centres and hospitals for treatment. Only on aggravation of symptoms due to respiratory failure, do they report and thereafter their recovery becomes difficult with medical management. The above case also highlights about patient presenting to the hospital on experiencing severe symptoms of COVID-19 [5]. The above case presents successful treatment of the patient through holistic approach mainly medical management including nutrition, physiotherapy management and psychological counselling of the patient. The successful treatment of the patient despite having severe symptoms will help restore faith and confidence of the common people in the health care system and would encourage people to co-operate and report early even with milder symptoms so can be effectively treated. Patient’s ABG report immediately after admission revealed hypoxaemia, hypocapnia with PaO2/ FiO2 ratio 45.85 indicating Type 1 respiratory failure and severe ARDS [8]. X-ray revealed ground glass opacities, reduction in the air entry, obliteration of cardiophrenic and costophrenic angles and some fibrotic changes bilaterally seen in (Figure 1 & 2).
Figure 1: A-P view Chest X-ray (1st day of Admission), bilateral patchy ground glass opacities right more than left.
Figure 2: A-P view Chest X-ray (5th day post admission), Ground glass opacities and fibrotic changes visible bilaterally.
The patient was properly counselled by the treating doctor regarding his health condition and medical treatment for the same to bring down anxiety and fear of the patient owing to severe symptoms of COVID-19. Patient was on medication regime as prescribed by the treating doctor and was provided a healthy nutritious diet by the hospital. Subsequent ABG reports revealed improvement in PaO2 levels on giving supplemental oxygen signifying the presence of ventilation perfusion mismatch, such patients are able to maintain satisfactory level of arterial oxygenation without requiring intubation and mechanical ventilation [9]. The patient was referred for Physiotherapy on the 5th day after admission. Physiotherapy treatment was given along with supplemental oxygen support according to the published guidelines for physiotherapy practice in COVID-19 [2, 6, 10]. Patient’s pulse rate and oxygen saturation were continuously monitored during each exercise using pulse oximeter and exercises were progressed depending on patient’s Rate of Perceived Exertion (RPE) and maintenance of normal ranges of vitals during the exercise with help of adequate rest between exercises. Exercises were progressed from gentle in-bed limb movements, relaxation and breathing exercises, to limb and breathing exercises with patient sitting bedside and progressed to spot marching and ambulation.
In-bed exercises mainly included ankle toe movements, heel slides, active range of motion exercises of wrist, elbow and shoulder joints and diaphragmatic breathing exercises for relaxation in propped up supine position (5-10 repetitions). These exercises ensured normal mobility of the joints and prevented complications due to immobility like deep vein thrombosis. Positioning was taught to the patient and was asked to perform every 2 hourly as per the COVID Awake Repositioning/ Proning Protocol (CARP protocol) to improve hypoxaemia which involved switching after every 10-15 minutes between left side-lying, right side lying and sitting upright 60 -90 degrees [11]. Prone positioning was started as per tolerance of the patient from 5 minutes and gradually increased to 30 minutes/session asking the patient to perform it 3 to 4 times a day. Positional changes also helped to prevent bed sores and its related complications. Further progression involved taking the patient into bed side sitting and performing active Upper limb and Lower limb range of motion exercises followed by breathing exercises (All 5-10 repetitions).
Breathing exercises involved diaphragmatic and segmental breathing along with thoracic expansion exercises. When patient started tolerating sitting position, progression was made to standing position. Initially the patient felt giddy which improved when patient spent more time sitting upright as advised. When the patient started tolerating standing position and maintaining normal vitals in standing, he was progressed with spot marching, rotation of head and trunk for balance training (5-10 repetitions) and walking sideways besides the bed (5 steps on each side). On subsequent days when the complaints of giddiness subsided, progression was made with patient made to walk around the bed (2 circles). As per the guidelines, drop of oxygen saturation of >3 percent and/or increase in the pulse rate above 120 beats per minute meant terminating the exercise and giving rest to the patient to restore the normal resting oxygen saturation and pulse rate and continuing thereafter if these vitals are stable [2, 6, 10]
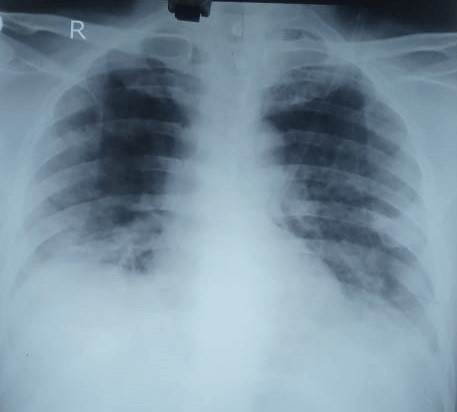
Figure 3: A-P view Chest X-ray (7th day post admission), an improvement in air entry bilaterally.
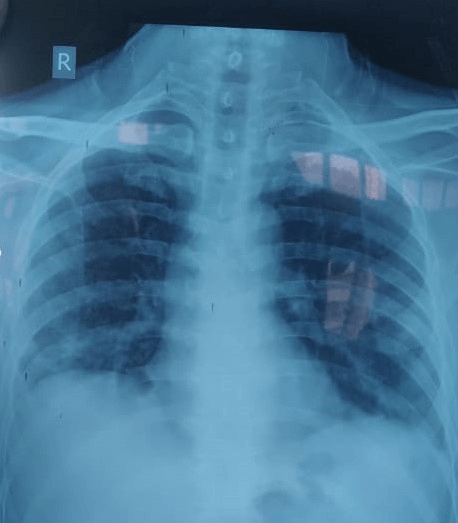
Physiotherapy intervention along with medical management helped in improving ventilation perfusion mismatch, alveolar ventilation by optimizing oxygen transport and in maintaining normal fluid distribution in the body [12]. It also helped to prevent complications of bed rest, deconditioning and muscle weakness [13]. The physiotherapy management in parallel with medical management, nutritional care and counselling of the patient ensured excellent recovery, objectively demonstrated by improvement in the latter ABG reports and X-rays (Figures 3 & 4).
Figure 4: A-P view Chest X-ray (15th day post admission), bilateral fluffy shadows seen indicative of resolving ARDS.
The patient was able to maintain normal oxygen saturation (98%) on 2L/min oxygen supplementation with normal vitals after 18 days of hospitalisation and 14 days of physiotherapy treatment parallelly with the medical management in the High Dependency Unit. He was later transferred to a general COVID ward (on maintaining normal oxygen saturation on 2L/min) where medical and physiotherapy treatment continued and was finally discharged when he started maintaining normal oxygen saturation on room air.
Conflicts of Interest
None.
Funding
None.
Acknowledgements
The authors acknowledge Dr. Mohan Joshi (Dean) for allowing us to carry out this study, Dr. Rachna Arora (Assistant Professor, Physiotherapy Department) for assistance in editing and reviewing, Dr. Rosemarie Desouza (Professor, Department of Internal Medicine), Patient whose information was used, All Postgraduate Students, faculty and Staff Members of Physiotherapy School & Centre, T.N.M.C & B.Y.L Ch Nair Hospital.
Ethical Approval
Our institution, Topiwala National Medical College and B. Y. L. Nair Ch. Hospital does not require ethical approval for reporting individual cases or case series.
Consent
Written informed consent was obtained from the patient for their anonymized information to be published in this article.
Abbreviations
SPO2: Saturation of Peripheral Oxygen
ICU: Intensive Care Unit
mMRC: Modified Medical Research Council
RT-PCR: Reverse Transcription Polymerase Chain Reaction
BiPAP: Bilevel Positive Airway Pressure
ECG: Electrocardiogram
ABG: Arterial Blood Gas
PaO2: Partial Pressure of Oxygen
FiO2: Fraction of Inspired Oxygen
ARDS: Acute Respiratory Distress Syndrome
RPE: Rate of Perceived Exertion
CARP: COVID Awake Repositioning Protocol
BMV: Bag Mask Ventilation
O2: Oxygen
PCO2: Partial Pressure of Carbon Dioxide
HCO3: Bicarbonate
L/min: Litres/min
Inj.: Injection
IL-6: Interleukin-6
g/dl: Gram/decilitre
ng/ml: Nanogram/millilitre
pg/ml: Picogram/millilitre
μg/ml: Microgram/millilitre
A-P: Anteroposterior
mmHg: Millimeters of mercury
mmol/L: millimoles/Litre
Article Info
Article Type
Case ReportPublication history
Received: Mon 20, Jul 2020Accepted: Thu 30, Jul 2020
Published: Thu 06, Aug 2020
Copyright
© 2023 Chhaya V. Verma. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.CEI.2020.02.07
Author Info
Chhaya V. Verma Suresh K. Patel Gayatri S. Jere Rakesh Bhadade
Corresponding Author
Chhaya V. VermaPhysiotherapy School & Centre, TN Medical College & BYL Nair Charitable Hospital, Maharashtra, India
Figures & Tables
Table 1: Investigations.
|
Investigations |
Values/Findings |
Interpretation |
|
Haemoglobin |
12.0 g/dl |
Borderline normal |
|
ECG |
Heart rate: 87 beats per minute, Premature Ventricular Contractions observed in V5, V6 and was suggestive of Left Axis Deviation. |
Suggestive of Left Axis Deviation. |
|
Ferritin |
1265 ng/ml |
Increased |
|
Interleukin-6 |
210 pg/ml |
Increased |
|
D-Dimer |
11.1 μg/ml |
Increased |
|
RT-PCR(10/06/2020) (Before hospitalisation) |
Positive |
COVID positive |
|
RT-PCR(15/06/2020) (3 days of hospitalisation) |
Positive |
COVID positive |
|
RT-PCR(29/06/2020) (2 weeks after hospitalisation) |
Negative |
COVID negative |
Table 2: Laboratory reports of ABG Analysis from the date of admission.
|
Date |
13/06/2020 |
16/06/2020 |
17/06/2020 |
18/06/2020 |
21/06/2020 |
|
Day of admission |
1st day |
4th day |
5th day |
6th day |
9th day |
|
O2 status |
BiPAP 100% |
BMV 15L/min |
BMV 15L/min |
BMV 15L/min |
BMV 15L/min |
|
pH |
7.497 |
7.467 |
7.314 |
7.389 |
7.384 |
|
PCO2 (mmHg) |
28.1 |
25.4 |
27 |
34.6 |
44.9 |
|
HCO3 (mmol/L) |
23.2 |
21.2 |
15.3 |
21.3 |
24.8 |
|
PO2 (mmHg) |
45.8 |
53.9 |
55.8 |
71.1 |
117 |
|
SPO2 (%) |
85.7 |
89.5 |
84.3 |
93.7 |
98 |
|
PaO2/FiO2 |
45.8 |
81.67 |
84.55 |
107.73 |
177 |
|
Date |
22/06/2020 |
23/06/2020 |
24/06/2020 |
27/06/2020 |
30/06/2020 |
|
Day of admission |
10th day |
11th day |
12th day |
15th day |
18th day |
|
O2 status |
BMV 15L/min |
BMV 15L/min |
BMV 10L/min |
BMV 8L/min |
BMV 10L/min |
|
pH |
7.411 |
7.417 |
7.436 |
7.443 |
7.434 |
|
PCO2 (mmHg) |
44.4 |
44.6 |
42 |
33 |
38.5 |
|
HCO3 (mmol/L) |
26.3 |
28 |
27.8 |
22.1 |
25.2 |
|
PO2 (mmHg) |
140.1 |
141.1 |
191 |
115.2 |
122 |
|
SPO2 (%) |
99.2 |
99.2 |
99.3 |
98.4 |
98.9 |
|
PaO2/FiO2 |
212 |
213.79 |
374.51 |
256 |
239.22 |
Table 3: Change in vital parameters with inpatient supervised physiotherapy management.
|
Date |
17th June |
18th June |
19th June |
20th June |
22nd June |
23rd June |
24th June |
|||||||||
|
Physiotherapy treatment day |
Day 1 |
Day 2 |
Day 3 |
Day 4 |
Day 5 |
Day 6 |
Day 7 |
|||||||||
|
O2 Supply(L/min) |
BiPAP; FiO2: 100% |
BMV 15L |
BMV 15L |
BMV 15L |
BMV 15L |
BMV 15L |
BMV 10L |
|||||||||
|
Pulse Rate (bpm) |
Pre |
85 |
85 |
87 |
85 |
90 |
90 |
103 |
||||||||
|
Post |
88 |
90 |
88 |
113 |
110 |
112 |
110 |
|||||||||
|
SPO2 (%) |
Pre |
96 |
95 |
97 |
99 |
97 |
100 |
99 |
||||||||
|
Post |
97 |
99 |
97 |
98 |
100 |
100 |
96 |
|||||||||
|
Positioning (side lying) |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Prone lying |
|
|
|
|
Y |
Y |
Y |
|||||||||
|
Breathing Exercises |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
In bed exercise |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Sitting exercises |
|
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Standing |
|
|
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Balance exercises in Standing |
|
|
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Spot Marching |
|
|
|
Y |
Y |
Y |
Y |
|||||||||
|
Walking |
|
|
|
|
Y |
Y |
Y |
|||||||||
|
Date |
25th June |
26th June |
27th June |
29th June |
30th June |
1st July |
2nd July |
|||||||||
|
Physiotherapy treatment day |
Day 8 |
Day 9 |
Day 10 |
Day 11 |
Day 12 |
Day 13 |
Day 14 |
|||||||||
|
O2 Supply(L/min) |
BMV 10L |
BMV 10L |
BMV 8L |
BMV 6L |
BMV 6L |
Nasal prongs 2L |
Nasal prongs 2L |
|||||||||
|
Pulse Rate (bpm) |
Pre |
98 |
96 |
88 |
112 |
108 |
102 |
112 |
||||||||
|
Post |
105 |
102 |
102 |
120 |
116 |
112 |
120 |
|||||||||
|
SPO2 (%) |
Pre |
100 |
100 |
100 |
99 |
98 |
97 |
98 |
||||||||
|
Post |
95 |
99 |
100 |
98 |
99 |
99 |
95 |
|||||||||
|
Positioning (side lying) |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Prone lying |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Breathing Exercises |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
In bed exercise |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Sitting exercises |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Standing |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Balance exercises in Standing |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Spot Marching |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
|
Walking |
Y |
Y |
Y |
Y |
Y |
Y |
Y |
|||||||||
Y: represents exercise was given on that day; BiPAP: Bilevel Positive Airway Pressure; BMV: Bag Mask Ventilation, L/min: litres/ minute, SPO2: Saturation of peripheral oxygen.
References
- Marco Cascella, Michael Rajnik, Arturo Cuomo, Scott C Dulebohn, Raffaela Di Napoli et al. (2020) Features, Evaluation and Treatment Coronavirus (COVID-19). StatPearls. [Crossref]
- Peter Thomas, Claire Baldwin, Bernie Bissett, Ianthe Boden, Rik Gosselink et al. (2020) Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother 66: 73-82. [Crossref]
- Symptoms of Coronavirus. Centers for Disease Control and Prevention.
- Shima Behzad, Leila Aghaghazvini, Amir Reza Radmard, Ali Gholamrezanezhad (2020) Extrapulmonary manifestations of COVID-19: Radiologic and clinical overview. Clin Imaging 66: 35-41. [Crossref]
- Revised Guidelines on Clinical Management of COVID- 19 (2020) Government of India Ministry of Health & Family Welfare Directorate General of Health Services (EMR Division).
- Chhaya V Verma, Rachna D Arora, Jaimala V Shetye, Niteen D Karnik, Pranali C Patil et al. (2020) Guidelines of physiotherapy management in acute care of COVID-19 at dedicated COVID center in Mumbai. J Indian Assoc Physiother 14: 55-60.
- mMRC (Modified Medical Research Council) Dyspnea Scale.
- Xu Li, Xiaochun Ma (2020) Acute respiratory failure in COVID-19: is it “typical” ARDS? Crit Care 24: 198. [Crossref]
- Martin J Tobin (2020) Basing respiratory management of COVID-19 on physiological principles. Am J Respir Crit Care Med 201: 1319-1320. [Crossref]
- Guidelines for Chest Physiotherapy management of COVID 19 in Indian Setup-MS OTPT Council (2020).
- COVID19 – Awake Pronation – A guest write-up by David Gordon (2020).
- Nim Pathmanathan, Nicola Beaumont, Andrew Gratrix (2015) Respiratory physiotherapy in the critical care unit. Continuing Education in Anaesthesia, Critical Care & Pain 15: 20-25.
- Juultje Sommers, Raoul H H Engelbert, Daniela Dettling Ihnenfeldt, Rik Gosselink, Peter E Spronk et al. (2015) Physiotherapy in the intensive care unit: an evidence-based, expert driven, practical statement and rehabilitation recommendations. Clin Rehabil 29: 1051-1063. [Crossref]
