Journals
Penetrating Cervical Neck Injuries in Children: About a Case
A B S T R A C T
Penetrating wounds of the neck are rare traumas in children, providers of mortality and high morbidity due to the density of the vital structures of this region and the lack of protection. Their management, a real challenge for the surgeon, has evolved over the years, going from systematic exploration to more selective management. We report the case of an 8-year-old child, victim of a penetrating cervical trauma after falling on a stick to the partner, who was successfully treated at the Rabat Children's Hospital. We will also discuss the emergency management methods for these cervical injuries.
Keywords
Traumas, neck, penetrating, children
Introduction
Penetrating neck trauma is rare in children. Due to the presence of vital structures and the absence of protective means, these lesions can be a source of increased morbidity and even mortality. The main cause of death is massive bleeding due to damage to the vessels in the neck. The care must therefore be the most optimal. Here we report the case of an 8-year-old female child who suffered a penetrating cervical trauma from falling on a stick in the countryside. She was successfully taken care of by removing the piece of wood without any complications.
Case Description
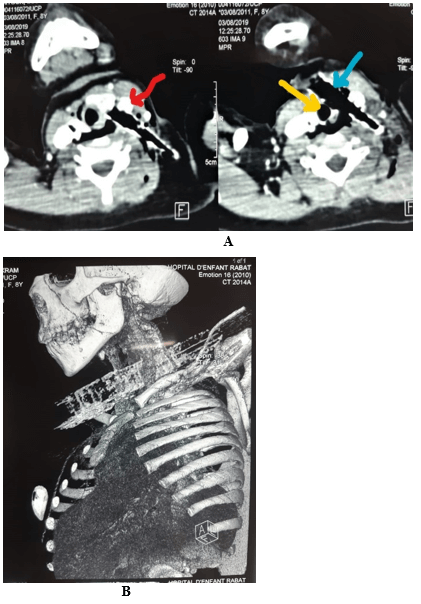
The case is of an 8-year-old girl, with no particular pathological history, schooled. The patient was victim of a cervical penetrating trauma in the countryside during holidays. She was running after a cow when she accidentally tripped over a stone and fell on a stick she was holding in her hand. The stick pierced her neck motivating her transport to the Provincial Hospital Center. After a summary assessment and first emergency care, the patient was referred to the pediatric surgical emergency department of the Rabat University Hospital. Received 4 hours after the trauma in the emergency room, the patient’s clinical examination found a conscious, anxious but calm girl, with stable hemodynamics and respiratory function. Her pulse was at 95 bpm, her blood pressure at 115/70 mmHg, and her SpO2 at 98 % to ambient air. Examination of the cervical region found a wooden stick piercing the neck, with an anterior entry point and moving diagonally to a left lateral exit point, thus occupying zones I and II of the neck (Figure 1). The presence of a carotid pulse and the absence of a cervical hematoma are noted. There also was no sign of stridor, nor dysphonia, nor subcutaneous emphysema. Vesicular murmurs were normally perceived and symmetrical to pulmonary auscultation.
Figure 1: When the child arrives, there is a wooden stick piercing the neck on both sides. The bar entered anteriorly and exited from the laterally.
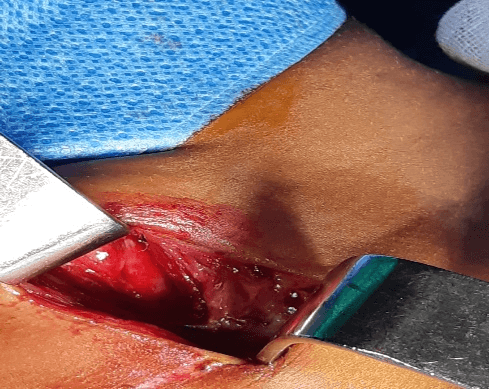
After monitoring and carrying out blood tests: blood count, ionogram and blood request, and given the stable condition of the patient in terms of hemodynamics and respiration, cervicothoracic computed tomography (CT) with injection of contrast product and 3D reconstruction was performed (Figures 2A & 2B). It showed a foreign body piercing the left lobe of the thyroid, brushing the posterior edge of the left common carotid and internal jugular which remain permeable, and brushing the anterior face of the trachea which keeps its sphericity, with subcutaneous emphysema. There was no extravasation of the contrast product. The 3D reconstruction of the images clearly showed the trace of the foreign body which is close to the blood vessels without individualization of a hematoma. The patient was admitted to the operating room under general anaesthesia, intubated and ventilated. The exploration found the foreign body crossing the cervical midline, brushing the trachea with an oblique course towards the latero-cervical part where it passes behind the jugulocarotid pedicle. After extension of the anterior wound for 2 cm, we performed a careful extraction of the foreign body. During extraction, the carotid pulse was closely monitored, we also watched closely for any bleeding in the jugulocarotid region, cervical hematoma, or tracheal murmur (Figure 3).
Figure 2: A) Computed tomography (CT) showing the foreign body (blue arrow) directed diagonally brushing the anterior surface of the trachea (yellow arrow) and passing behind the jugulocarotid pedicle (red arrow). B) 3D three-dimensional reconstruction of CT images of the patient's neck, showing the foreign body passing behind the jugulocarotid pedicle.
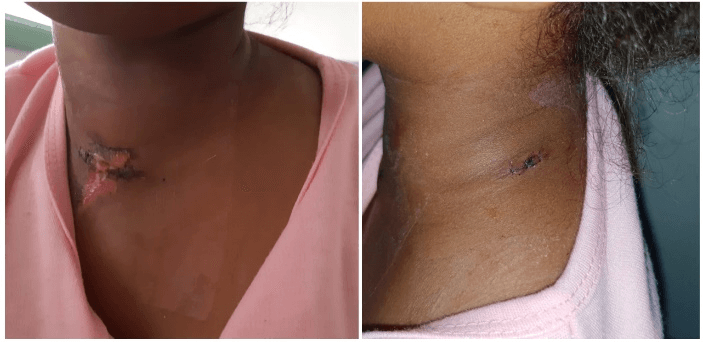
After irrigation and washing with physiological serum, the entry (anterior) and exit (lateral) wounds were sutured (Figure 4) and the patient left with intravenous Antibiotics for 05 days. Postoperatively, we monitored: hemodynamic constants (heart rate, blood pressure), respiratory functions (respiratory rate, oxygen saturation, pulmonary auscultation), neurological constants (GCS, focal neurological deficit), temperature as well as local appearance (monitoring for the installation of a hematoma, subcutaneous emphysema, wound infection). There were no complications. The child was discharged after 5 days of hospitalization. At 1-month follow-up (Figure 5), she is doing well with well-healed wounds. No anomalies have been identified. A Doppler ultrasound was performed and did not reveal a jugulocarotid pseudo-aneurysm.
Figure 3: The stick was successfully removed: the integrity of the jugulocarotid pedicle was noted after the extraction of the foreign body.
Figure 4: Final postoperative aspect on day 2 after extraction of the foreign body and suturing of the wounds.
Figure 5: Final postoperative appearance after 1 month.
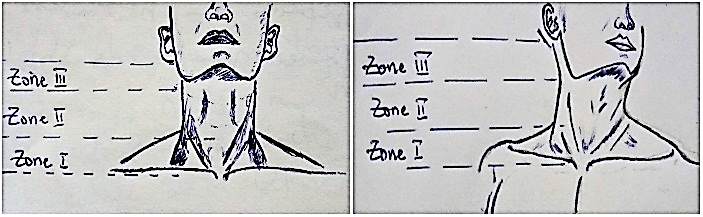
Figure 6: Lesional anatomy of the neck, visualization of the 3 zones.
Discussion
Penetrating neck traumas are defined as the invasion of the muscle in the neck. These are rare traumas in children [1].
In practice, the neck is divided into 3 distinct anatomical zones (Figure 6):
i. Zone I, between the clavicle and the cricoid cartilage.
ii. Zone II, between the cricoid cartilage and the angle of the mandible.
iii. Zone III, between the angle of the mandible and the base of the skull.
As in our patient, lesions in zone II are the most frequent in both adults and children (50% of cases) [2].
Penetrating cervical wounds in children are more serious compared to adults. Indeed, due to their size, vital cervical structures in children (in particular vascular, respiratory and neurological) are more likely to be damaged in the event of trauma than in adults; and the failures seen in penetrating wounds are thought to set in much more quickly than in adults [3]. These injuries have a reputation for being difficult to assess because they involve a very complex anatomical region containing blood vessels, the aerodigestive system, cervical vertebrae and spinal cord. This also explains the seriousness of the lesions likely to be caused in the event of a penetrating wound. Their management therefore represents a real challenge. It begins with the management of pain and anxiety-inducing factors that can act as a brake and potentially worsen the patient's condition. Careful clinical examination should be performed.
The notion of stability (hemodynamic, respiratory, neurological) is essential to establish. Indeed, an unstable patient will be admitted directly to the operating room for a surgical exploration while, on the other hand, a stable patient may benefit (depending on the clinical examination) from adapted investigations in order to optimize and rationalize the management. The management of penetrating cervical wounds has evolved. The « wait-and-see » attitude (associated with high mortality) prevailed before The Second war. Then came the systematic exploration of penetrating neck wounds which reduced mortality but was associated with no less negligible morbidity with white surgical explorations [1].
The current attitude, according to the recommendations concerning the management of penetrating cervical trauma in adults called the “No Zone approach”, in particular for lesions in zone II, consists of the selection of patients to operate based on the contribution provided by imaging in order to avoid abusive explorations [1, 2]. This attitude adopted in children has reduced the morbidity associated with systematic investigations (especially lesions of small nerve structures) [4]. It is clear that there are some cases where mandatory surgical exploration remains justified, especially in the following situations: extensive or pulsatile hematoma, shock or severe active bleeding, blood in the oropharynx, emphysema under cutaneous on standard radiograph, murmur, thrill, crepitations or dysphagia [4]. For hemodynamically stable patients with penetrating cervical trauma, CT angiography and three-dimensional image reconstruction is the ideal exam to explore penetrating cervical lesions. It is an accessible, non-invasive, non-operator dependent examination capable of providing information on the integrity of cervical blood vessels, bone, airway and digestive structures [4-8].
For our patient, performing this examination made it possible to identify the lesions and adapt the management without too much difficulty. The foreign body was removed, and no vascular, respiratory or digestive damage was found.
The attitude in the event of the absolute need for exploration varies depending on the type of lesion objectified. Bhatt et al. recommend that in the event of vascular lesions (carotid arteries, brachiocephalic etc.), vascular repair by performing bypass (in the event of complex lesions) rather than vascular ligation, which is a source of significant mortality (50% mortality in case of ligation against 17% in case of repair) [2]. Esophageal lesions must benefit from primary repair associated with drainage and more or less the use of a muscle flap (depending on the extent of the defect and the association of tracheal or vascular lesions) [2]. Isolated pharyngeal lesions can be managed without surgery with antibiotics and nasogastric tubes for a period of 2 weeks in cases of pharyngeal fistula. Finally, follow-up of all patients should be for at least 3 months to watch for the late appearance of a carotid pseudoaneurysm.
Conclusion
Penetrating cervical wounds are rare in children and can cause potentially fatal injuries. Their definitive management continues to be à subject of debate in the medical community. Some advocate systematic explorations of the neck while others are for a more selective management which is possible thanks to modern imaging techniques, enabling to reach immediate and precise diagnosis, provide an effective management, and prevent serious complications.
Nowadays, not every cervical wound is a formal indication for surgery. Indeed, with the exception of hemodynamic and respiratory instabilities which must admit the patient directly to the operating room, the performance of radiological examinations such as helical angiography-CT is necessary in order to avoid excessive surgeries and improve results by providing the right treatment for each patient.
Article Info
Article Type
Case ReportPublication history
Received: Fri 31, Jul 2020Accepted: Thu 13, Aug 2020
Published: Mon 24, Aug 2020
Copyright
© 2023 Toualouth Lafia. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2020.03.08
Author Info
Toualouth Lafia F Ettayebi H Zerhouni
Corresponding Author
Toualouth LafiaPediatric Surgical Emergency Department of the Rabat Children's Hospital, Faculty of Medicine and Pharmacy, Mohammed V University of Rabat, Morocco
Figures & Tables


References
- Monica Abdelmasih, Ahmed Kayssi, Graham Roche Nagle (2019) Penetrating paediatric neck trauma. BMJ Case Rep 12: e226436. [Crossref]
- Nikita R Bhatt, Morgan McMonagle (2015) Penetrating neck injury from a screwdriver: can the No Zone approach be applied to Zone I Injures. BMJ Case Rep 2015: bcr2015212666. [Crossref]
- Yan Wang, Yu Sun, Tao Zhou, Guo Hui Liu, Xiao Meng Zhang et al. (2018) Penetrating neck trauma caused by a rebar: A case report. Medicine (Baltimore) 97: e0468. [Crossref]
- Kathryn M Hewett, Larry Mellick (2012) A case of penetrating neck trauma in a child. Pediatr Emerg Care 28: 49-51. [Crossref]
- Carol A L Hanson, Jill Ann Smith (2007) Penetrating Neck Injuries in Children. J Trauma Nurs 14: 12-16. [Crossref]
- Scott D Steenburg, Clint W Sliker, Kathirkamanathan Shanmuganathan, Eliot L Siegel (2010) Imaging evaluation of penetrating neck injuries. Radiographics 30: 869-886. [Crossref]
- Karen Woo, David P Magner, Matthew T Wilson, Daniel R Margulies (2005) CT angiography in penetrating neck trauma reduces the need for operative neck exploration. Am Surg 71: 754-758. [Crossref]
- E Cesareo, Samia Draoua, Hugues Lefort, K Tazarourte (2012) Plaies pénétrantes du cou. Urgences 2012, Edition: SFMU et SAMU de France, Chapter: 48 (Traumatologie vitale), Publisher: SFMU et SAMU de France, Editors: Société Française de Médecine d'Urgence 1-11.
