Pathological Fracture of Femoral Neck Associated to Femoral Head Osteonecrosis: Case Report
A B S T R A C T
Introduction: The osteonecrosis of femoral head is a progressive and devastating condition for the prognosis of the coxofemoral joint, with an increase in its prevalence and an etiology of multifactorial nature, and with compromise specially in young or middle age (20 to 40 years of age) patients [1-3]. The fractures associated to femoral head osteonecrosis are very rare, being the subchondral portion the site with a higher compromise, and the junction between the necrotic bone and the bone under remodeling process another site of potential fracture [4-7]. The management of this condition can vary from a conservative management to a surgical management with total hip arthroplasty, depending on patient’s clinic and the extension of his necrotic lesion.
Discussion: This patient presents a sub-capital fracture of his femoral neck, associated to osteonecrosis of the femoral head. This patient was managed with decompression of the osteonecrosis nucleus plus bone graft and osteosynthesis with cannulate screws, in order to decrease bone hypertension and avoid femoral collapse.
Conclusion: Although femoral neck fractures, as a complication from femoral head osteonecrosis are rare, in our patient such association can be found due to the worsening of his painful clinical features and the absence of a previous traumatic event, which allows discarding femoral osteonecrosis as a fracture complication.
Keywords
Osteonecrosis, femoral head, spontaneous fractures, fracture internal fixation, complication
Introduction
The osteonecrosis of femoral head is a progressive and devastating condition for the prognosis of the coxofemoral joint, with an increase in its prevalence and an etiology of multifactorial nature, and with compromise, especially in young or middle age (20 to 40 years of age) patients [1-3]. The fractures associated to femoral head osteonecrosis are very rare, being the subchondral portion the site with higher compromise, and the junction between the necrotic bone and the bone under remodeling process another site of potential fracture [4-7]. The management of this condition can vary from a conservative management to a surgical management with total hip arthroplasty, depending on patient’s symptoms and the extension of his necrotic lesion. As this is a so rare pathology, the objective of this work is to release this clinical case, its evolution, management and the importance of differentiating femoral head osteonecrosis as the cause of fracture.
Clinical Case
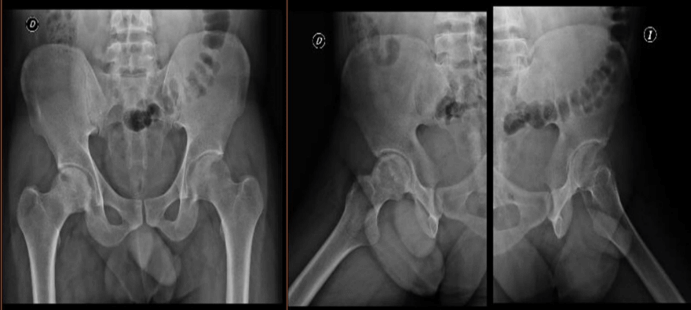
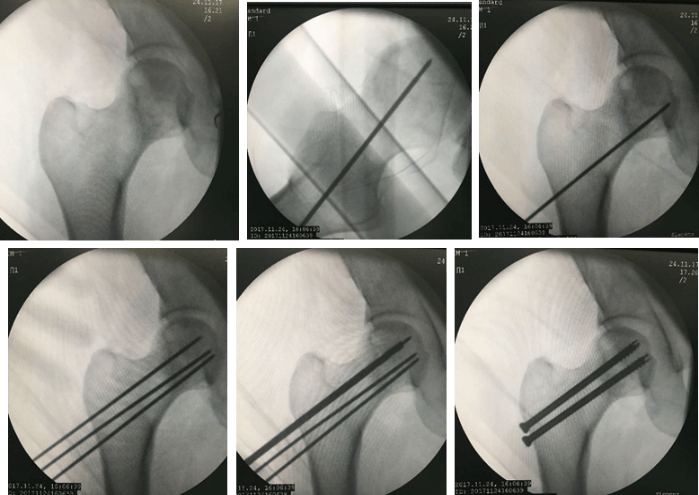
A 28 years old male patient, without pathological background, occasional consumer of alcohol, with a two weeks clinical pattern of evolution of right hip pain with an insidious inception that worsened the day before consultation, associated to limp, and without any background of trauma. At physical exam he showed good general conditions, without any septic aspect, antalgic limp of right lower member, sign of C+, without flexion contracture, painful rolling, 30° bending due to pain, without tolerance to gyration due to pain, no pain at light palpation of inguinal region, no hernias are felt. Comparative pelvis radiography (Figure 1), cystic image of femoral head on support surface and head sclerosis on AP and Lateral projection. Normal hem-leukogram and PCR 3.44. In front of a high suspicion of femoral head osteonecrosis, an urgent Magnetic Nuclear Resonance (MNR) is requested of right hip (Figure 2), which shows an image that suggests femoral head osteonecrosis, Ficat II-III, with associated synovitis, without collapse, but with cyst and associated and no displaced sub-capital fracture. The patient is taken to surgery and under vision guided by fluoroscopy (Figure 3), a decompression is performed through lateral tackling of subtrochanteric insertion of the necrotic nucleus and pass of bone substitute through trephine. Later, an osteosynthesis of the sub-capital fracture is performed using two (2) 6.5 mm cannulate screws, without complications (Figure 4). A satisfactory postoperative evolution, full mobility arches, without residual pain and a radiologic follow up at 8 and 10 weeks without evidence of collapse, fracture displacement or necrotic lesion increase.
Figure 1: AP and Lateral Hip Comparative Radiography, with evidence of cystic lesion on support zone. Date: November 16, 2017.
Figure 2: MNR of right hip in coronal, axial cut, T1 and T2 respectively. White arrow: femoral head osteonecrosis nucleus with associated cyst. Orange arrow: sub-capital fracture not displaced.
Figure 3: Fluoroscopic vision of decompression of the osteonecrosis nucleus and osteosynthesis with 6.5 mm cannulate screws. Date: November 24, 2017.
Figure 4: Postoperative Radiological Follow-up, without evidence of collapse, displacement or lesion increase. Date: January 16, 2018 - 3rd postoperative week (upper) and February 7, 2018 - 6th postoperative week (lower).
Discussion
The atraumatic osteonecrosis of femoral head is a progressive and devastating condition for the prognosis of the coxofemoral joint, with an increase of its prevalence and an etiology of multifactorial nature, and with compromise, especially in young or middle age (20 to 40 years of age) patients [1-3]. It has been demonstrated that in a large number of these cases, a genetic predisposition exists, as well as associated risk factors that favor the appearance of these lesions, among which we can mention alcohol heavy consumption and/or the intake of corticosteroids, which have been identified in 80% of the cases [1]. The main physiopathology of osteonecrosis is secondary to the restriction in blood flow, with a later limitation to oxygen and nutrients release, which leads to the appearance of necrosis, which in advanced phases can result in femoral head collapse and the consequent appearance of coxofemoral osteoarthrosis, representing 5 to 10% of the total number of hip full arthroplasties [3].
Multiple phasing systems for femoral osteonecrosis have been proposed, among which are the ARCO (Association Research Circulation Osseous) system, Ficat and Arlet System, the Steinberg System from the University of Pennsylvania and the JOA (Japanese Orthopedic Committee) [1]. Considering that this patient was classified under the Ficat and Arlet System, the different phases are herein explained, Phase I: normal radiography; Phase II: diffuse sclerosis or cystic lesions; Phase IIA: without signs of subchondral collapse; Phase IIB: subchondral fracture (increasing sign); Phase III: crushing of femoral head; Phase IV: osteoarthrosis with joint reduction, articular collapse or acetabular compromise [8].
From a clinical point of view, a patient can appear asymptomatic or symptomatic, and in the latter case, the pain, restriction for mobility arches and limp are the predominant symptoms. According to the literature, every small, asymptomatic and medial location lesion can be treated using a conservative management with observation; however, large lesions, although asymptomatic can progress to the collapse of femoral head in 25 to 50% of the cases, and this is why a conservative management should be avoided and surgical management will be preferred, as well as in the cases of symptomatic lesions, large lesions and lesions with collapse [1, 9-11]. The surgical management is based on joint preservation procedures, even when there is no collapse and total hip arthroplasty, once the collapse has been established.
As for the diagnostic aids, the blood analyses are normal, a reason why it is necessary to perform standard projections of the hip (AP and Lateral), ideally comparative, because an incidence of bilateral compromise of 42% to 72% of the cases has been evidenced [2]. However, once a suspicion exists of femoral head osteonecrosis, the Gold Standard is MNR of the hips. The typical change in T1 images is a unique density line that represents a separation of the normal bone from the necrotic area, and in the T2 images, a high-density line associated to granulate tissue with a higher vascularization degree is evidenced [12]. Additionally, the presence of edema of the bone medulla is a mark of disease progression.
The conservative management is based on oral drugs such as bisphosphonates, which allow a decrease of the osteoclastic activity, reducing in this way the risk of collapse [1]. The use of hyperbaric oxygen chambers has also been described, as well as shock wave therapy and electromagnetic pulses. However, no sufficient studies exist for demonstrating the effectiveness of these last management measures. The surgical management is based on multiple useful techniques that seek articular preservation, and in which the decompression of the osteonecrosis nucleus using percutaneous drills is an alternative in small symptomatic lesions, in order to reduce intraosseous hypertension, because as a result of cellular inflammation and infiltration during the necrosis process, an increase of intraosseous pressure occurs on a bone without distension capacity [1]. Multiple techniques have been described for achieving decompression, whether through a single orifice or multiple orifices, finding that the drilling of multiple orifices is better, without losing sight of the high risk of femoral neck fracture after the procedure, a risk that is directly related to the diameter of the drills used, the number of orifices and the technique (lateral with subtrochanteric entrance vs anterolateral entrance) [3].
Another surgical technique described is the femoral osteotomy, in which on the basis of transtrochanteric or intertrochanteric angular rotational osteotomies, the necrotic region of the femoral head is moved away from the load regions, allowing in this way the healing or delaying of the pathology’s progression [1]. However, this is a technique with very limited indications, and a high rate of complications [13]. Additionally, the use of bone matrix has been reported with the purpose of providing structural support and allowing the remodeling and healing of the necrotic area. This bone matrix can be no-vascularized, and implanted through a window on the base of the femoral neck or through a channel made as a result of nucleus decompression, as it is in the case of our patient; or, it can be vascularized on the basis of a graft of the calf bone or the iliac tricortical bone [14, 15]. Although this is a very useful technique, it is not very frequently used due to the high rate of technical difficulties and resources necessary for the procedure itself [16].
Finally, the hip total arthroplasty is the indicated management once the femoral head has collapsed and/or an acetabular compromise exists. As for the fractures associated to the femoral osteonecrosis, it is known that the subchondral portion is the site with a larger compromise, and the union between the necrotic bone and the bone under remodeling process is another site of potential fracture, generally located in the sub-capital area [4-7]. However, it should be considered that this kind of fractures are very rare during the progression of the femoral head osteonecrosis, and they are very rarely associated to a traumatic event. The sub-capital fractures associated to large osteonecrosis areas present a bad prognosis when they are managed with osteosynthesis, cases in which the performance of hip total arthroplasty is indicated. However, when they are associated to small necrosis lesions, the articular preservation measures, plus osteosynthesis with cannulate screws are useful, as in the case of our patient [1, 2, 17]. Ikemura et al. showed such usefulness in the differentiation of the clinical characteristics of sub-capital fracture for insufficiency of the associated osteonecrosis, in which the risk factors play a fundamental role in such differentiation, because although most of the femoral neck fractures occurs with a latter osteonecrosis as complication, the not displaced fractures of the femoral neck, as a complication of the femoral head osteonecrosis, are very rare [17-20].
Conclusion
Although the femoral neck fractures, as a complication of the femoral head osteonecrosis are rare, in our patient it is possible to find such association due to the worsening of his painful clinical features and the absence of a previous traumatic event, which allows discarding the femoral osteonecrosis as a complication of his fracture. The objective of the treatment allows complying with the purposes described in the literature, improving the related symptomatology, decreasing the intraosseous hypertension, avoiding the collapse of the femoral head, promoting the preservation of the coxofemoral joint, and in this way postposing as much as possible, the performance of a hip total arthroplasty.
Conflicts of Interest
The authors don’t have any conflict of interest.
Ethical Considerations
We obtained an informed consent from the patient and an authorization and approval from the Ethics Committee of El Rosario Clinic in Medellin.
Article Info
Article Type
Case ReportPublication history
Received: Tue 17, Dec 2019Accepted: Mon 30, Dec 2019
Published: Tue 31, Dec 2019
Copyright
© 2023 Victoria Eugenia Restrepo Noriega. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2019.01.05
Author Info
Mejía Luz A Montoya Beatriz E Victoria Eugenia Restrepo Noriega
Corresponding Author
Victoria Eugenia Restrepo NoriegaSurgeon Physician, Surgical Assistant, Orthopedics and Traumatology El Rosario Clinic, Downtown See, Medellin, Colombia
Figures & Tables


References
- Chughtai M, Piuzzi NS, Khlopas A, Jones LC, Goodman SB et al. (2017) An evidence-based guide to the Treatment of osteonecrosis of the femoral head. Bone Joint J 99-B: 1267-1279. [Crossref]
- Lee JS, Suh KT (2005) A pathological fracture of the femoral neck associated with osteonecrosis of the femoral head and a stress fracture of the contralateral femoral neck. J Arthroplasty 20: 807-810. [Crossref]
- Cilla M, Checa S, Preininger B, Winkler T, Perka C et al. (2017) Femoral head necrosis: A finite analysis of common and novel surgical techniques. Clin Biomech 48: 49-56. [Crossref]
- Kenzora JE, Glimcher MJ (1985) Pathogenesis of idiopathic osteonecrosis: the ubiquitous crescent sign. Orthop Clin North Am 16: 681-696. [Crossref]
- Merle d’Aubigne R, Postel M, Mazabraud A, Massias P, Gueguen J et al. (1965) Idiopathic necrosis of the femoral head in adults. J Bone Joint Surg Br 47: 612-633. [Crossref]
- Kim YM, Lee SH, Lee FY, Koo KH, Cho KH et al. (1991) Morphologic and biomechanical study of avascular necrosis of the femoral head. Orthopedics 14: 1111-1116. [Crossref]
- Usui M, Inoue H, Yukihiro S, Abe N (1996) Femoral neck fracture following avascular necrosis of the femoral head. Acta Med Okayama 50: 111-117. [Crossref]
- Ficat RP, Arlet J (1980) Necrosis of the femoral head. In: Hungerford DS, ed. Ischemia and necrosis of bone. Baltimore: Williams & Wilkins 171-182.
- Mont MA, Zywiel MG, Marker DR, McGrath MS, Delanois RE (2010) The natural history of untreated asymptomatic osteonecrosis of the femoral head: a systematic literature review. J Bone Joint Surg Am 92: 2165-2170. [Crossref]
- Ha YC, Jung WH, Kim JR, Seong NH, Kim SY et al. (2006) Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am 88 Suppl 3: 35-40. [Crossref]
- Nam KW, Kim YL, Yoo JJ, Koo KH, Yoon KS et al. (2008) Fate of untreated asymptomatic osteonecrosis of the femoral head. J Bone Joint Surg Am 90: 477-484. [Crossref]
- Liu LH, Zhang QY, Sun W, Li ZR, Gao FQ (2017) Corticosteroid-induced Osteonecrosis of the Femoral Head: Detection, Diagnosis, and Treatment in Earlier Stages. Chin Med J (Engl) 130: 2601-2607. [Crossref]
- Ha YC, Kim HJ, Kim SY, Kim KC, Lee YK et al. (2011) Effects of age and body mass index on the results of transtrochanteric rotational osteotomy for femoral head osteonecrosis: surgical technique. J Bone Joint Surg Am 93 Suppl 1: 314-321. [Crossref]
- Seyler TM, Marker DR, Ulrich SD, Fatscher T, Mont M (2008) No vascularized bone grafting defers joint arthroplasty in hip osteonecrosis. Clin Orthop Relat Res 466: 1125-1132. [Crossref]
- Zhao D, Zhang Y, Wang W, Liu Y, Li Z et al. (2013) Tantalum rod implantation and vascularized iliac grafting for osteonecrosis of the femoral head. Orthopedics 36: 789-795. [Crossref]
- Johnson AJ, Mont MA, Tsao AK, Jones LC (2014) Treatment of femoral head osteonecrosis in the United States: 16-year analysis of the Nationwide Inpatient Sample. Clin Orthop Relat Res 472: 617-623. [Crossref]
- Fukui K, Kaneuji A, Matsumoto T (2015) Occult fracture of the femoral neck associated with extensive osteonecrosis of the femoral head: A case report. Int J Surg Case Rep 14: 136-140. [Crossref]
- Ikemura S, Yamamoto T, Motomura G, Nakashima Y, Mawatari T et al. (2013) The utility of clinical features for distinguishing subchondral insufficiency fracture from osteonecrosis of the femoral head. Arch Orthop. Trauma Surg 133: 1623-1627. [Crossref]
- Johansson C, Ekenman I, Tornkvist H, Eriksson E (1990) Stress fractures of the femoral neck in athletes. The consequence of a delay in diagnosis. Am J Sports Med 18: 524-528. [Crossref]
- Blickenstaff LD, Morris JM (1966) Fatigue fracture of the femoral neck. J Bone Joint Surg Am 48: 1031-1047. [Crossref]
