Pain Neuroscience Education for Depression: A Pilot Study
A B S T R A C T
Objective: To determine if a brief, one-on-one pain neuroscience education (PNE) session delivered by a physical therapist (PT) can influence depression.
Methods: A convenience sample of patients with persistent low back pain (LBP) (n = 23) attending PT with moderate to severe depression (Patient Health Questionnaire-9 [PHQ-9]) participated in the study. Patients received a standardized, one-on-one 30-minute PNE session by a PT with pre- and post-intervention measures of low back and leg pain (Numeric Pain Rating Scale [NPRS]), pain catastrophization (Pain Catastrophization Scale [PCS]), pain knowledge (Revised Neurophysiology of Pain Questionnaire [rNPQ] and depression (PHQ-9).
Results: Immediately following PNE, all measures improved, with low back and leg pain not being significant (pback = 0.345 and pleg = 0.633), while pain catastrophization (p = 0.047), pain knowledge (p = 0.001) and depression (p = 0.004) reaching significant improvements. The PNE session shifted various patients to lower levels of depression, with 21.8% of the patients’ improvement in depression meeting or exceeding the minimal clinical important difference.
Conclusion: PNE may be a safe, clinically effective way to help a subgroup of patients attending PT with depression. More studies are needed to further explore the results from this pilot study.
Keywords
Pain neuroscience education, depression, physical therapy, mental and behavioural health
Introduction
According to the National Institute of Health it is estimated approximately one in five people in the United States (US) suffer from a mental, behavioural or emotional disorder and account for an annual spending in excess of $80 billion [1]. Within this data, it is estimated approximately six percent of Americans suffer from major depression, with the life-time prevalence of depression estimated at 21.3% in women and 12.7% in males [1, 2]. Unfortunately, depression has been shown to also be a leading cause of suicide, thus showcasing the importance for healthcare providers to screen for depression and treat or refer accordingly [2].
Pain and depression have been shown to be interrelated, especially persistent pain [3-5]. Within this coexistence is an important clinical mandate for physical therapists (PTs): The need and ability to screen for depression [6]. It is proposed that PTs would use validated tools to screen for depression and refer to a mental health provider as needed [4, 7]. For example, the Patient Health Questionnaire-9 (PHQ-9) has been shown to be highly sensitive and could be used to rule out significant levels of depression [7]. The PHQ-9 validates the current belief that depression is seen as a continuum, anchored with lower levels of depression on the one side and anchored by major depression on the other side [7, 8]. By having a cut-off score the decision is made to refer patients on the higher end of the scale to a mental health provider [8]. The clinical question is then what to do with patients who don’t meet the cut-off score for referral to a mental health provider?
In lieu of the coexistence of depression and persistent pain, it is not surprising that current best evidence for depression and persistent pain shows significant overlap which includes primarily some type of cognitive intervention, aerobic exercise and skilled delivery of medication including selective-serotonin-reuptake-inhibitors and/or membrane stabilizers [9-12]. In PT, a cognitive treatment specifically aimed at helping people with persistent pain has emerged in the last 20 years, referred to as pain neuroscience education (PNE) [13, 14]. PNE is an educational strategy that focuses on teaching people more about the neurobiological and neurophysiological processes involved in their pain experience [13-16]. Current best evidence regarding musculoskeletal pain provides strong support for PNE to positively influence pain ratings, dysfunction, and limitations in movement, pain knowledge and healthcare utilization [17, 18]. Additionally, PNE has shown to powerfully influence psychosocial issues that powerfully influence pain and depression: fear-avoidance and pain catastrophization [17, 18]. In light of the emerging PNE evidence, need to screen for depression and need to find treatments to help patients on the lower-end scales of depression, this study aimed to examine if PNE could positively influence depression in patients attending PT for persistent low back pain (LBP).
Methods
I Study Design
Pre-approval was obtained at three PT clinics for this study where three orthopaedic residents were providing care. Institutional review board approval was obtained from St. Ambrose University. The study is a case series consisting of pre- and post-intervention measures with no follow-up.
II Participants
A convenience sample of patients attending outpatient PT for persistent LBP was used for the study. Patients were screened against the inclusion and exclusion criteria and if eligible, asked to participate in the study and provide written informed consent (parents for patients under 18). Upon consent, demographic data was collected (no personal identifiable information), including age, gender, ethnicity, duration and location of pain including body chart, education level, work status, past personal and family history of LBP and surgical interventions for LBP. Inclusion criteria included presenting at PT for a primary complaint of persistent LBP, LBP of more than 6 months, fluent in writing and treading the English language and willing to participate. Exclusion criteria were patients with a PHQ9 score of less than 10 points (no or mild depression) and presenting with any cognitive deficits rendering them unsuitable for PNE (i.e., stroke, traumatic brain injury, etc.).
III Intervention
The PNE session lasted 30 minutes and was delivered in a one-on-one educational format with a PT using prepared images, drawings and metaphors [17]. The 30-minute PNE session was chosen to reflect a clinically meaningful intervention in a typical allocated time frame in clinical practice. The content of the PNE is described in detail elsewhere, using metaphors to explain various aspects of pain including sensitization of the peripheral and central nervous system (sensitive alarm system metaphor); spreading pain (nosy neighbours metaphor); increasing problems with focus and concentration (brain meeting metaphor) and difficulty with fatigue and sleep (lion metaphor) [19].
IV Outcome Measures
Following the completion of the demographic intake forms, patients completed a series of standardized and validated instruments. The disability questionnaire was only completed before the intervention, while patients’ satisfaction was only assessed after the intervention.
i Disability (Oswestry Disability Index – ODI)
The ODI is a 10-item questionnaire used to assess different aspects of physical function [20]. Each item is scored from 0 to 5, with higher values representing greater disability. The total score is multiplied by 2 and expressed as a percentage. The ODI has been shown to be a valid and reliable measure of disability related to LBP [20-22].
ii Global Rate of Change Scale
The GROC scale is global rating of improvement and satisfaction over the course of treatment [23]. It does not measure a specific dimension such as pain or function but allows the patient to decide what they consider important. The GROC is a commonly used outcomes tool in clinical research, especially as it relates to musculoskeletal care including LBP [24, 25]. The most common formats of the GROC is typically a 7, 11, or 15 point scale on a number line with 0 in the middle and moving out one integer in the positive and negative numerical direction. The end anchors also contain the negative and positive words of “very much worse” and “very much improved” or “completely better” with “no change” being in the middle at zero [26]. For purposes of this study the recommended 15 -point scale will be used (-7 = very much worse, 0 = unchanged, 5 = completely recovered). The MCID for the GROC for musculoskeletal pain has been reported as a positive shift of 3 points or more (+3) [26, 27].
The following measurements were completed before and immediately following the PNE intervention:
i Low Back and Leg Pain (Numeric Pain Rating Scale – NPRS)
LBP and leg pain was measured with the use of a NPRS, as has been used in various studies on LBP and PNE [13, 14, 28, 29]. The minimal clinical important difference (MCID) for the NPRS for LBP is reported to be 2.0 [30].
ii Pain Catastrophization (Pain Catastrophization Scale – PCS)
The PCS is a self-report questionnaire that assesses inappropriate coping strategies and catastrophic thinking about pain and injury. The PCS has been used in previous PNE studies for LBP and demonstrated strong construct validity, reliability and stability [31-33]. The PCS utilizes a 13-item, 5-point Likert scale with higher scores indicating elevated levels of catastrophizing. Previous studies utilizing the PCS have shown a median score of 18 that of healthy individuals and in patients with pain the PCS is generally higher, with a score over 30 reported as a high level of pain catastrophization [33]. The minimal detectable change (MDC) for the PCS is reported to be 9.1 [34].
iii Pain Knowledge (Revised Pain Neurophysiology Questionnaire – rNPQ)
The NPQ is based on a current pain science text and was used in a previous study measuring the neurophysiology knowledge of patients and healthcare personnel [35, 36]. The original NPQ is a 19-item questionnaire requesting ‘true’; ‘false’; or ‘not sure’ answers to statements, with higher scores indicating more correct answers. Since the development of the NPQ a statistical analysis of the NPQ has led to the development of an abbreviated revised NPQ (rNPQ) with 13 questions which removed ambiguous questions [37]. The revised 13-question rNPQ was used in this study. No information is available on what constitutes a meaningful shift in NPQ/rNPQ scores, but studies using the NPQ and rNPQ have shown positive changes for patients, healthcare providers and students after PNE with mean increases in NPQ/rNPQ scores of 27% [19].
iv Depression (Patient Health Questionnaire – PHQ-9)
The PHQ-9 is the nine-item depression scale and one of the most validated tools in mental health assisting clinicians with diagnosing depression and monitoring treatment response [38-40]. The nine items of the PHQ-9 are based directly on the nine diagnostic criteria for major depressive disorder in the Diagnostic and Statistical Manual of Mental Disorders-IV. Total PHQ-9 scores are classified as 0-4 (none to minimal depression); 5-9 (mild depression); 10-14 (moderate depression); 15-19 (moderately severe depression and 20-27 (severe depression) [41]. In regard to MCID, it is suggested that the PHQ9 responds differently, based on the extent of the starting depression score (i.e., mild versus severe depression), with recent updates reporting a 20% reduction of scores as a useful guide for clinical impact [42, 43].
Immediately following the intervention, changes were be assessed using the NPRS, PCS, rNPQ, PHQ-9 and GROC. Patients were then done with the study portion of their visit and then continued PT as usual, directed by the attending therapist.
V Statistical Analysis
This was an exploratory study to investigate the feasibility and possible immediate impact of the PNE intervention on depression in patients with persistent LBP. Descriptive statistics were used to describe the demographic variables and patient-reported outcome measures of the patients in the study using Microsoft Excel™ version 16.0 (Table 1), including means, ranking, percentages, standard deviation (SD), etc. To compare pre- and post-intervention measures of NPRS for back and leg pain, PCS, rNPQ and PHQ9, paired-sample t-tests were conducted.
Results
31 patients were originally selected for the pilot study. Eight patients scored below 10 on the PHQ9 and were eliminated, leaving 23 subjects in the pilot study. The demographic information on the subjects can be found in (Table 1).
Table 1: Demographic information.
|
Measure |
Subjects (n = 23) |
|
Female |
13
(56.5%) |
|
Mean
age in years (range) |
50
(15-79) |
|
Ethnic: ● White,
non-Hispanic ● Hispanic ● African American ● Other |
19
(82.6%) 2
(8.8%) 1
(4.3% 1
(4.3%) |
|
Education: ● High School ● Other ● Graduate school ● Post-graduate |
8
(34.8%) 8
(34.8%) 4
(17.4%) 3
(13%) |
|
Mean
duration of pain in years (range) |
13.83
(0.8 – 36.3) |
|
Currently
employed |
13
(56.5%) |
|
Have
undergone surgery for their condition (% of total) |
4
(17.4%) |
|
Family
history of pain |
11
(47.8%) |
|
Mean
low back pain (NPRS) (SD) |
5.2
(2.43) |
|
Mean
leg pain (NPRS) (SD) |
3.2
(2.97) |
|
Mean
disability (ODI) (%) |
17.6
(35.2%) |
|
Depression
rating on PHQ-9 (Mean) (SD) ● Moderate (10-14) ● Moderately severe
(15-19) ● Severe (20-27) |
15.35
(3.65) 10
(43.5%) 10
(43.5%) 3
(13%) |
I Low Back and Leg Pain
Both low back and leg pain failed to be reduced after PNE in a statistically significant manner (pback = 0.345 and pleg = 0.633). On an individual level for LBP, 5 patients (21.7%) had a reduction in pain after PNE meeting or exceeding MCID of 2 points, while 2 patients (8.8%) exhibited the same results for leg pain.
II Pain Catastrophization
Prior to PNE, mean PCS score (31.6) exceeded the threshold for a high PCS score and following PNE, the mean PCS score moved below the high threshold (µ = 28.3), with a statistically significant improvement overall (p = 0.047).
III Pain Knowledge
Pain knowledge shifted positively in a statistically significant manner (p = 0.001) from 39.8% to 52.5%.
IV Depression
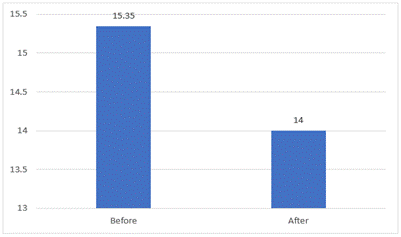
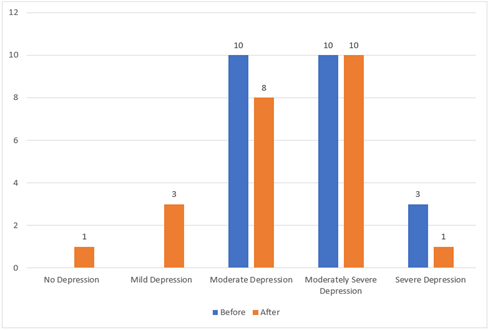
Immediately following PNE, depression improved in a statistically significant manner (p = 0.04) (Figure 1). Overall PHQ-9 scores were reduced by 8.8%, not meeting the MCID. Five patients (21.8%) met or exceeded the MCID reduction in depression, with four of the five being moderately severe or severely depressed prior to PNE. Changes in levels of depression had a weak, positive correlation with pain knowledge improvement (r = 0.24). Figure 2 Showcases a decrease in overall levels of depression when compared to levels of depression prior to PNE. Two of the three patients with severe depression moved down to moderately severe depression.
Figure 1: Mean PHQ-9 scores before and immediately following PNE.
Figure 2: Shift in PHQ-9 scores per category after PNE.
V Patient Experience
Following the PNE session, patient experience as measured by the GROC scale showed a mean score of +1.38, with seven patients (30.4%) meeting or exceeding the MCID of +3. Depression scores had a moderate, positive correlation with rate of satisfaction with the patient experience of the PNE intervention (r = 0.61).
Discussion
This is the first exploratory study assessing the potential benefit of PNE for patients attending PT with depression. Results from this study show that a brief, one-on-one, PT-led PNE session has a positive effect on a subgroup of patients with depression. Concerns over mental health, including depression, is mounting, especially in light of the coronavirus disease of 2019 (COVID-19) [44, 45]. The sudden acute respiratory syndrome (SARS) that started in 2002 showed significant long-term changes in mental health with up to 65% of survivors developing major depression [46, 47]. Data from the COVID-19 pandemic shows similar impacts on mental health [44, 45]. Furthermore, it is well-documented that there’s a significant shortage of mental health providers globally, including for the treatment of depression [48, 49]. Persistent pain and depression often coexist, yet treatment for pain and depression often involve different healthcare providers and disciplines. PT is not seen as an avenue for the treatment of depression, yet it’s estimated that 45-50 million Americans annually seek PT for the care of their LBP, of which approximately 10-15 million suffer with chronic LBP [50]. The results of this study, albeit a small pilot, is important since it may indicate that PT may be able to play a bigger role in the screening, triage and even treatment of depression. In this study, a sub-group of patients with depression had significant changes and patients at higher levels of depression were shifted to lower, safer levels.
Depression is a serious condition with significant potential for risk and harm and patients on the higher end of depression will no doubt need more comprehensive and multidisciplinary care [51]. On the flipside, results such as these may indicate that a subgroup of patients can be helped by a PT, potentially helping with early-intervention and potentially alleviating pressure on the significant need to mental health providers. This conclusion is further enhanced by the fact that emerging psychosocial approaches such as motivational interviewing, acceptance and commitment therapy, trauma-informed care and more, is finding its way into PT literature and curricula [52-54].
The positive shifts in pain, pain catastrophization, pain knowledge and patient satisfaction concur with current PNE evidence[17, 55]. The question that should be answered is why PNE may have benefitted this sample of patients with moderate to severe depression? Pain catastrophization is often correlated with higher levels of depression [56, 57] and in this sample, initial PCS scores overall exceeded the cut-off value of a high PCS score indicative of protracted recovery from treatment [33]. Following PNE, PCS scores improved significantly, which is important since reduction of PCS scores after PNE has been shown to be one of the biggest predictors of success in PNE [58]. Additionally, it is well-established that following PNE, pain knowledge improves, with this study similarly showing the increase in pain knowledge [14, 17]. The key aspect, however, is that increased pain knowledge has some positive correlation with positive shifts in depression. These preliminary results may indicate that reduction in pain catastrophization and improved knowledge of pain may be a start in trying to understand if and how PNE may be a beneficial treatment for patients attending PT with LBP and comorbid depression.
The results from this study should be seen as what it is – a pilot study. It contains various limitations. First, the study contains no control subjects, thus not allowing for a true test of the efficacy of PNE for depression. Future designs should explore randomized clinical trials with control groups. Second, there was no long-term follow-up, which does not allow a true indication of the efficacy of PNE over time. Third, the intervention used in this study was modeled on previous studies on LBP and it can be argued that a more specific PNE-depression protocol should be developed with the inclusion of patients and their needs. Another limitation is that the patient sample only consisted of patients with LBP and depression and cannot be extrapolated to comorbid depression for other medical diagnoses. The final limitation, which may actually highlight the importance of these findings, is the lack of a PNE plus (PNE+) approach, which is currently seen as the gold-standard for PNE-delivery [17, 58]. In this study, patients only received PNE, whereas current best evidence showcase that PNE plus other behavioural strategies, including exercise, mindfulness, relaxation, etc., is superior to PNE-only [17, 59]. It is thus recommended that follow-up studies study the effect of PNE plus exercise, or PNE plus relaxation, which is also closer to the current best evidence approach for chronic pain and depression.
Conclusion
A brief, one-on-one, PT-led PNE session has a positive effect on a subgroup of patients with depression. PNE may be a safe, clinically effective way to help a subgroup of patients attending PT with depression. More studies are needed to further explore the results from this pilot study.
Article Info
Article Type
Research ArticlePublication history
Received: Wed 13, Oct 2021Accepted: Tue 26, Oct 2021
Published: Wed 10, Nov 2021
Copyright
© 2023 Adriaan Louw. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.PDR.2021.02.01
Author Info
Adriaan Louw Ellen Wendling Dustin Hawk Nicole Sturdevant Hailey Louw Kevin Farrell
Corresponding Author
Adriaan LouwEvidence in Motion, Story City, Iowa, USA
Figures & Tables
Table 1: Demographic information.
|
Measure |
Subjects (n = 23) |
|
Female |
13
(56.5%) |
|
Mean
age in years (range) |
50
(15-79) |
|
Ethnic: ● White,
non-Hispanic ● Hispanic ● African American ● Other |
19
(82.6%) 2
(8.8%) 1
(4.3% 1
(4.3%) |
|
Education: ● High School ● Other ● Graduate school ● Post-graduate |
8
(34.8%) 8
(34.8%) 4
(17.4%) 3
(13%) |
|
Mean
duration of pain in years (range) |
13.83
(0.8 – 36.3) |
|
Currently
employed |
13
(56.5%) |
|
Have
undergone surgery for their condition (% of total) |
4
(17.4%) |
|
Family
history of pain |
11
(47.8%) |
|
Mean
low back pain (NPRS) (SD) |
5.2
(2.43) |
|
Mean
leg pain (NPRS) (SD) |
3.2
(2.97) |
|
Mean
disability (ODI) (%) |
17.6
(35.2%) |
|
Depression
rating on PHQ-9 (Mean) (SD) ● Moderate (10-14) ● Moderately severe
(15-19) ● Severe (20-27) |
15.35
(3.65) 10
(43.5%) 10
(43.5%) 3
(13%) |
References
1.
Health N.I.O. (2015) Prevalence data for any mental
illness and major depression prevalence in the US.
2.
Kessler RC, Borges G, Walters EE (1999) Prevalence
of and risk factors for lifetime suicide attempts in the National Comorbidity
Survey. Arch Gen Psychiatry 56: 617-626. [Crossref]
3.
Vlaeyen JWS, Linton SJ (2000) Fear-avoidance and
its consequences in chronic musculoskeletal pain: a state of the art. Pain
85: 317-322. [Crossref]
4.
Pincus T, Burton AK, Vogel S, Field AP (2002) A
systematic review of psychological factors as predictors of
chronicity/disability in prospective cohorts of low back pain. Spine (Phila
Pa 1976) 27: E109-E120. [Crossref]
5.
Krause SJ, Wiener RL, Tait RC (1994) Depression and
pain behaviour in patients with chronic pain. Clin J Pain 10: 122-127. [Crossref]
6.
Boissonnault WG, Bass C (1991) Medical screening
examination: not optional for physical therapists. J Orthop Sports Phys Ther
14: 241-242. [Crossref]
7.
Delitto A, George SZ, Dillen LV, Whitman JM, Sowa G
et al. (2012) Low back pain. J Orthop Sports Phys Ther 42: A1-A57. [Crossref]
8.
Arroll B, Khin N, Kerse N (2003) Screening for
depression in primary care with two verbally asked questions: cross sectional
study. BMJ 327: 1144-1146. [Crossref]
9.
Bisson JI, Roberts NP, Andrew M, Cooper R, Lewis C
(2013) Psychological therapies for chronic post-traumatic stress disorder
(PTSD) in adults. Cochrane database Syst Rev 2013: CD003388. [Crossref]
10. Edmonds M, McGuire H, Price J (2004) Exercise therapy for chronic
fatigue syndrome. Cochrane Database Syst Rev CD003200. [Crossref]
11. Larun L, Brurberg KG, Jensen JO, Price JR et al. (2015) Exercise
therapy for chronic fatigue syndrome. Cochrane Database Syst Rev
CD003200. [Crossref]
12. Wiffen PJ, Derry S, Bell RF, Rice AS, Tölle TR et al. (2017) Gabapentin
for chronic neuropathic pain in adults. Cochrane Database Syst Rev 6:
CD007938. [Crossref]
13. Moseley L (2002) Combined physiotherapy and education is efficacious
for chronic low back pain. Aust J Physiother 48: 297-302. [Crossref]
14. Moseley L (2003) Joining Forces – Combining Cognition – Targeted Motor
Control Training with Group or Individual Pain Physiology Education: A
Successful Treatment For Chronic Low Back Pain. J Man Manip Ther 11:
88-94.
15. Meeus M, Nijs J, Oosterwijck JV, Alsenoy VV, Truijen S (2010) Pain
physiology education improves pain beliefs in patients with chronic fatigue
syndrome compared with pacing and self-management education: a double-blind
randomized controlled trial. Arch Phys Med Rehabil 91: 1153-1159. [Crossref]
16. Louw A, Zimney K, Puentedura EJ, Diener I (2016) The efficacy of pain
neuroscience education on musculoskeletal pain: A systematic review of the
literature. Physiother Theory Pract 32: 332-355. [Crossref]
17. Louw A, Diener I, Butler DS, Puentedura EL (2011) The effect of
neuroscience education on pain, disability, anxiety, and stress in chronic
musculoskeletal pain. Arch Phys Med Rehabil 92: 2041-2056. [Crossref]
18. Louw A, Puentedura E, Schmidt S, Zimney K (2018) Pain Neuroscience
Education. 2 Minneapolis, MN: OPTP.
19. Hakkinen A, Kautiainen H, Järvenpää S, Kautiainen MA, Ylinen J (2007)
Changes in the total Oswestry Index and its ten items in females and males pre-
and post-surgery for lumbar disc herniation: a 1-year follow-up. Eur Spine J
16: 347-352. [Crossref]
20. Deyo RA, Battie M, Beurskens AJ, Bombardier C,
Croft P et al. (1998) Outcome measures for low back pain research.
A proposal for standardized use. Spine (Phila Pa 1976) 23: 2003-2013. [Crossref]
21. Fritz JM, Irrgang JJ (2001) A comparison of a modified Oswestry Low
Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys
Ther 81: 776-788. [Crossref]
22. Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP et al.
(2005) Core outcome measures for chronic pain clinical trials: IMMPACT
recommendations. Pain 113: 9-19. [Crossref]
23. Pengel LHM, Refshauge KM, Maher CG, Nicholas MK, Herbert RD et al.
(2007) Physiotherapist- directed exercise, advice, or both for subacute low
back pain: a randomized trial. Ann Intern Med 146: 787-796. [Crossref]
24. Hancock MJ, Maher CG, Latimer J, McLachlan AJ, Cooper CW et al. (2007)
Assessment of diclofenac or spinal manipulative therapy, or both, in addition
to recommended first-line treatment for acute low back pain: a randomised
controlled trial. Lancet 370: 1638-1643. [Crossref]
25. Kamper SJ, Maher CG, Mackay G (2009) Global rating of change scales: a
review of strengths and weaknesses and considerations for design. J Man
Manip Ther 17: 163-170. [Crossref]
26. Puentedura EJ, Cleland JA, Landers MR, Mintken PE, Louw A et al. (2012)
Development of a clinical prediction rule to identify patients with neck pain
likely to benefit from thrust joint manipulation to the cervical spine. J
Orthop Sports Phys Ther 42: 577-592. [Crossref]
27. Moseley GL (2005) Widespread brain activity during an abdominal task
markedly reduced after pain physiology education: fMRI evaluation of a single
patient with chronic low back pain. Aust J Physiother 51: 49-52. [Crossref]
28. Cleland JA, Childs JD, Whitman JM (2008) Psychometric properties of the
Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical
neck pain. Arch Phys Med Rehabil 89: 69-74. [Crossref]
29. Childs JD, Piva SR, Fritz JM (2005) Responsiveness of the numeric pain
rating scale in patients with low back pain. Spine (Phila Pa 1976) 30:
1331-1334. [Crossref]
30. Moseley GL, Nicholas MK, Hodges PW (2004) A randomized controlled trial
of intensive neurophysiology education in chronic low back pain. Clin J Pain
20: 324-330. [Crossref]
31. Moseley GL (2004) Evidence for a direct relationship between cognitive
and physical change during an education intervention in people with chronic low
back pain. Eur J Pain 8: 39-45. [Crossref]
32. Sullivan MJL, Bishop SR, Pivik J (1995) The Pain Catastrophizing Scale:
Development and validation. Psychol Assess 7: 524-532.
33. George SZ, C Valencia, Beneciuk JM (2010) A psychometric investigation
of fear-avoidance model measures in patients with chronic low back pain. J
Orthop Sports Phys Ther 40: 197-205. [Crossref]
34. Wall PD, Melzack R (2005) Textbook of Pain. 5th edn ed., London:
Elsevier.
35. Moseley L (2003) Unravelling the barriers to reconceptualisation of the
problem in chronic pain: the actual and perceived ability of patients and
health professionals to understand the neurophysiology. J Pain 4:
184-189. [Crossref]
36. Catley MJ, O'Connell NE, Moseley GL (2013) How good is the
neurophysiology of pain questionnaire? A Rasch analysis of psychometric
properties. J Pain 14: 818-827. [Crossref]
37. Han C, Jo SA, Kwak JH, Pae CU, Steffens D et al. (2008) Validation of
the Patient Health Questionnaire-9 Korean version in the elderly population:
the Ansan Geriatric study. Compr Psychiatry 49: 218-223. [Crossref]
38. Dejesus RS, Vickers KS, Melin GJ, Williams MD (2007) A system-based
approach to depression management in primary care using the Patient Health
Questionnaire-9. Mayo Clin Proc 82: 1395-1402. [Crossref]
39. Wittkampf K, Ravesteijn HV, Baas K, Hoogen HVD, Schene A et al. (2009)
The accuracy of Patient Health Questionnaire-9 in detecting depression and
measuring depression severity in high-risk groups in primary care. Gen Hosp
Psychiatry 31: 451-459. [Crossref]
40. Kroenke K, Spitzer RL, Williams JBW (2002) The PHQ-15: validity of a
new measure for evaluating the severity of somatic symptoms. Psychosom Med
64: 258-266. [Crossref]
41. Lowe B, Unützer J, Callahan CM, Perkins AJ, Kroenke K (2004) Monitoring
depression treatment outcomes with the patient health questionnaire-9. Med
Care 42: 1194-1201. [Crossref]
42. Kounali D, Button KS, Lewis G, Gilbody S, Kessler D et al. (2020) How
much change is enough? Evidence from a longitudinal study on depression in UK
primary care. Psychol Med 1-8. [Crossref]
43. Stein MB (2020) EDITORIAL: COVID-19 and Anxiety and Depression in 2020.
Depress Anxiety 37: 302. [Crossref]
44. Rajkumar RP (2020) COVID-19 and mental health: A review of the existing
literature. Asian J Psychiatr 52: 102066. [Crossref]
45. Mak IWC, Chu CM, Pan PC, You MGC, Chan VL (2009) Long-term psychiatric
morbidities among SARS survivors. Gen Hosp Psychiatry 31: 318-326. [Crossref]
46. Lee AM, Wong JGWS, McAlonan GM, Cheung V, Cheung C et al. (2007) Stress
and psychological distress among SARS survivors 1 year after the outbreak. Can
J Psychiatry 52: 233-240. [Crossref]
47. Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, Larson EH (2018)
Geographic Variation in the Supply of Selected Behavioral Health Providers. Am
J Prev Med 54: S199-S207. [Crossref]
48. Chaiyachati KH, Livesey C, Liao JM (2020) Going Beyond Cost-Sharing
Parity to Improve Behavioral Health Access. JAMA Netw Open 3: e2020232.
[Crossref]
49. Zheng P, Kao MC, Karayannis NV, Smuck M et al. (2017) Stagnant Physical
Therapy Referral Rates Alongside Rising Opioid Prescription Rates in Patients
With Low Back Pain in the United States 1997-2010. Spine (Phila Pa 1976)
42: 670-674. [Crossref]
50. Gallagher KC, Taylor CE (2021) Gatekeeper Training and the Medical
Community's Fight Against Depression and Suicide-A Shared Burden. JAMA Surg
156: 215-216. [Crossref]
51. Nijs J, Wijma AJ, Willaert W, Huysmans E, Mintken P et al. (2020)
Integrating Motivational Interviewing in Pain Neuroscience Education for People
With Chronic Pain: A Practical Guide for Clinicians. Phys Ther 100:
846-859. [Crossref]
52. Barker KL, L Heelas, F Toye (2016) Introducing Acceptance and
Commitment Therapy to a physiotherapy-led pain rehabilitation programme: an
Action Research study. Br J Pain 10: 22-28. [Crossref]
53. Guerrero AVS, Maujean A, Campbell L, Sterling M (2018) A Systematic
Review and Meta-Analysis of the Effectiveness of Psychological Interventions
Delivered by Physiotherapists on Pain, Disability and Psychological Outcomes in
Musculoskeletal Pain Conditions. Clin J Pain 34: 838-857. [Crossref]
54. Malfliet A, Kregel J, Coppieters I, Pauw RD, Meeus M et al. (2018)
Effect of Pain Neuroscience Education Combined With Cognition-Targeted Motor
Control Training on Chronic Spinal Pain: A Randomized Clinical Trial. JAMA
Neurol 75: 808-817. [Crossref]
55. Edwards RR, Cahalan C, Mensing G, Smith M, Haythornthwaite JA (2011)
Pain, catastrophizing, and depression in the rheumatic diseases. Nat Rev
Rheumatol 7: 216-224. [Crossref]
56. Bergbom S, Boersma K, Overmeer T, Linton SJ (2011) Relationship among
pain catastrophizing, depressed mood, and outcomes across physical therapy
treatments. Phys Ther 91: 754-764. [Crossref]
57. Louw A, Nijs J, Puentedura EJ (2017) A clinical perspective on a pain
neuroscience education approach to manual therapy. J Man Manip Ther 25:
160-168. [Crossref]
58. Louw A et al. (2020) Revisiting the Provision of Pain Neuroscience Education: An Adjunct Intervention for Patients, but a Primary Focus for Clinician Education. J Orthro Sports Phys Ther 1-12.
59. Wood L, Hendrick PA (2019) A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur J Pain 23: 234-249. [Crossref]
