Outcomes of Weight Loss, Diabetes, Hypertension and Obstructive Sleep Apnoea after Bariatric Surgery in Patients with Super Morbid Obesity
A B S T R A C T
Introduction: There is currently a high prevalence of obesity in the Arabian Gulf yet relatively little research on bariatric surgery. In this study we investigate the efficacy of bariatric surgery in patients with super morbid obesity, defined as a Body Mass Index (BMI) of ≥ 50 kg/m2.
Methods: All records of bariatric surgery at a single centre were examined. Outcomes measured include Body Mass Index (BMI), percentage Excess Weight Loss (%EWL), Obstructive Sleep Apnoea (OSA), Hypertension (HTN) and Type 2 Diabetes Mellitus (T2DM). Statistical relationships between %EWL against age, type of surgery and gender were analysed.
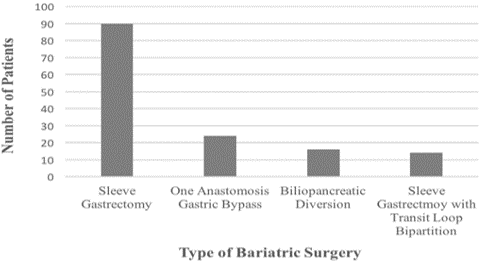
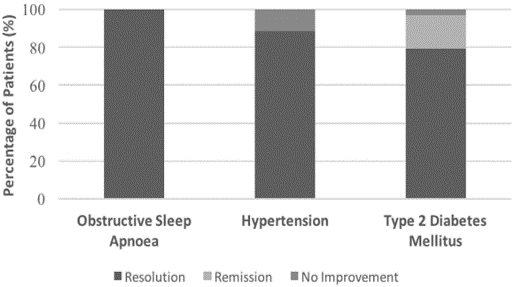
Results: 144 patients were found to meet the inclusion criteria. Mean pre-operative BMI was 56.9 ± 6.1 kg/m2. 90 (62.5%) patients underwent sleeve gastrectomy, 24 (16.7%) had one anastomosis gastric bypass, 16 (11.1%) had biliopancreatic diversion (Scopinaro’s procedure), and 14 (9.7%) had sleeve gastrectomy with transit loop bipartition. 12 months post-operatively, mean BMI was 37.7 ± 7.5 kg/m2, with a mean %EWL of 62.9% ± 17.9%. There was 100% OSA resolution, 95.3% HTN resolution, and 79.4% T2DM resolution. %EWL was found to decrease slightly with increased age, however no difference in %EWL was found between types of surgery or genders.
Conclusion: Bariatric surgery is effective and may be justified in patients with super morbid obesity, including the elderly population. However, there is a great need for larger, longitudinal studies. This would be made possible by hospitals employing more regular and systematic reporting of data, and encouragement of patients to follow up.
Keywords
Super morbid obesity, bariatric surgery, Arabian Gulf, sleeve gastrectomy, one anastomosis gastric bypass, biliopancreatic, diversion (scopinaro’s procedure), sleeve gastrectomy with transit loop, bipartition
Introduction
AlMarri et al. recently published a paper that brings to light the insufficient amount of research done on bariatric surgery in the Gulf. They found that the prevalence of adults with obesity in Bahrain (35.1%) is greater than that in the USA (33.7%), Australia (28.6%) and the UK (28.1%), yet there is less published research about bariatric surgery from Bahrain than from almost any other country. Just seven research articles were found regarding bariatric surgery in Bahrain, only two of which were found to measure health outcomes of patients post-bariatric surgery [1]. In Bahrain Defence Force (BDF) hospital, Al Khalifa et al. investigated 143 patients who underwent laparoscopic adjustable gastric banding. The patients had a mean Body Mass Index (BMI) of 45.8 kg/m2 in women and 45.3 kg/m2 in men [2]. The research at King Hamad University Hospital (KHUH) had involved 83 patients from 2012-2013 [3].
Our current investigation aims to expand on the research base so far, with a focus on patients with super morbid obesity. Super morbid obesity is defined as a BMI of ≥ 50 kg/m2 [4]. This super morbidly obese population appears to be growing faster than the population of people with a BMI < 50 kg/m2 [5]. However, bariatric surgery for this group tends to be high risk, with increased perioperative morbidity and mortality, insufficient post-operative weight loss, and higher recurrence rates of diabetes [4, 6]. In order to evaluate whether bariatric surgery is justified for patients in the Gulf, our study aims to investigate 12 month post-operative weight loss through BMI and percentage Excess Weight Loss (%EWL), resolution of obstructive sleep apnoea (OSA), hypertension (HTN) and type 2 diabetes mellitus (T2DM).
Methods
All hard files and electronic medical records of patients in KHUH from conception till September 2018 were retrospectively examined. Patients were included if they underwent bariatric surgery at KHUH, had a BMI of ≥ 50 kg/m2 at the time of surgery, and had follow up data at 12 months post-operatively. Patients were excluded if they had bariatric surgery done outside KHUH, had a BMI < 50 at the time of surgery, or did not have follow up data at 12 months. Weight, height, HbA1c, fasting blood glucose, blood pressure, and presence or absence of OSA was assessed in the outpatient clinic, both pre- and post-operatively, with a face-to-face survey as part of routine care. Before surgery, patients were assessed to be fit for surgery, and written informed consent was obtained from all participants. All surgeries were conducted by the same surgical team. Surgeries included sleeve gastrectomy, one anastomosis gastric bypass (OAGB), biliopancreatic diversion (Scopinaro’s procedure) (BPD), and sleeve gastrectomy with transit loop bipartition (SGTLB).
%EWL was calculated by the formula (initial BMI – final BMI) / (initial BMI – 25 kg/m2) * 100. %EWL was used in formal statistical analysis as it was considered the recommended parameter for reporting post-operative weight loss [7]. T2DM status was classified as remission, resolution, or no improvement. Remission was defined as an HbA1c of 6.0 - 6.5% and fasting blood sugar of 5.6-6.9 mmol/L, while resolution was defined as an HbA1c of < 6.0% and fasting blood sugar of < 5.6 mmol/L. The classification of both remission and resolution required that the patients be off oral hypoglycaemic agents or insulin [8]. Descriptive statistics for all parameters were performed. Data are expressed as mean ± one standard deviation. Relationships between % EWL against age, type of surgery and gender were investigated. The impact of age on % EWL was determined using Pearson product-moment correlation coefficient. % EWL differences between different types of bariatric surgery were investigated using one way between groups Analysis of Variance (ANOVA). % EWL differences between gender were investigated using an independent samples t-test. All analyses were performed using the Statistical Package for Social Sciences (IBM SPSS Statistics Version 25).
Figure 1: Types of Bariatric Surgery.
Table 1: Patient Characteristics.
|
Age at time of surgery |
|
|
Mean |
35.2 ± 10.6 |
|
Range |
15 - 64 |
|
Gender |
|
|
Male |
65 (45.1%) |
|
Female |
79 (54.9%) |
|
Nationality |
|
|
Bahraini |
136 (94.4%) |
|
Non-Bahraini |
8 (5.6%) |
|
Pre-operative BMI (kg/m2) |
|
|
Mean |
56.9 ± 6.1 |
|
Range |
50.0 - 77.8 |
|
Incidence of obstructive sleep apnoea |
64 (44.4%) |
|
Incidence of hypertension |
43 (29.9%) |
|
Incidence of type 2 diabetes mellitus |
41 (28.5%) |
|
Type of bariatric surgery |
|
|
Sleeve gastrectomy |
90 (62.5%) |
|
One anastomosis gastric bypass |
24 (16.7%) |
|
Biliopancreatic diversion |
16 (11.1%) |
|
Sleeve gastrectomy with transit loop bipartition |
14 (9.7%) |
Results
Out of 1,202 patients who had undergone bariatric surgery at this centre, 144 patients were included in our study. Table 1 describes patient demographics and pre-operative parameters. There were 2 patients under the age of 18 at the time of surgery (15 years old). The majority of patients were Bahraini, while the 8 non-Bahraini patients originated from other countries in the Middle East, including Jordan, Saudi Arabia, Syria, Iraq and Egypt. There were 5 patients with a BMI > 70 kg/m2. The number of patients undergoing each type of bariatric surgery is illustrated in (Figure 1), showing sleeve gastrectomy to be the most common procedure (62.5%). At 12 months, there was missing follow up data for 3 patients’ weight (therefore BMI and %EWL) measurement and 7 patients’ HbA1c and fasting blood glucose (therefore T2DM) measurements. Table 2 contains the 12-month post-operative outcomes of BMI, %EWL, OSA, HTN and T2DM, illustrated in (Figure 2). The mean BMI decreased from 56.9 ± 6.1 kg/m2 to 37.7 ± 7.5 kg/m2, which equated to a mean %EWL of 62.9% ± 17.9%. All patients with OSA had complete resolution of symptoms, while most patients with HTN had resolution (88.4%). Only 1 patient with T2DM (2.9%) had no improvement at 12 months.
Figure 2: Outcomes 12 Months Post-Operatively.
Table 2: Outcomes 12 Months Post-Operatively.
|
Mean post-operative BMI (N = 141) |
37.7 ± 7.5 kg/m2 |
|
Percentage Excess Weight Loss |
|
|
Mean overall (N = 141) |
62.9% ± 17.9% |
|
Mean after sleeve gastrectomy (N = 89) |
63.3% ± 17.0% |
|
Mean after one anastomosis gastric bypass (N = 23) |
62.8% ± 22.4% |
|
Mean after biliopancreatic diversion with duodenal switch (N = 16) |
56.8% ± 14.1% |
|
Mean after sleeve gastrectomy with transit bipartition (N = 13) |
62.4% ± 15.3% |
|
Mean for males (N = 63) |
64.3% ± 20.9% |
|
Mean for females (N = 78) |
62.4% ± 14.5% |
|
OSA resolution (N = 64) |
61 (100%) |
|
HTN resolution (N = 43) |
38 (88.4%) |
|
T2DM status (N = 34) |
|
|
No improvement |
1 (2.9%) |
|
Remission |
6 (17.6%) |
|
Resolution |
27 (79.4%) |
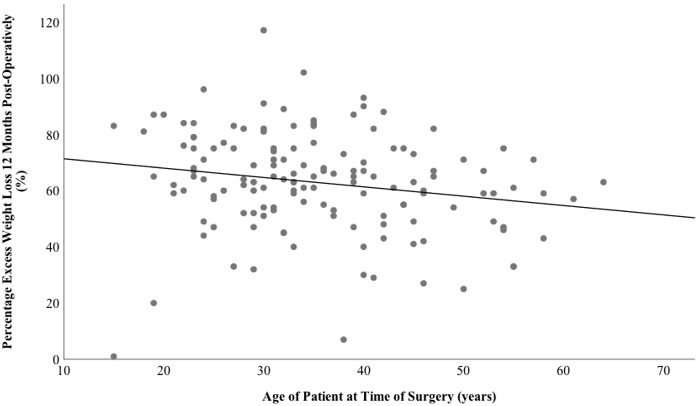
Pearson product-moment correlation coefficient was determined for age against %EWL. Preliminary analyses were performed to ensure no violation of the assumptions of normality, linearity and homoscedasticity. There was a statistically significant, but weak, negative correlation between the two variables: r = - 0.24, n = 141, p < 0.05. Increasing age was associated with decreased %EWL, also illustrated by the regression line of best fit in (Figure 3). A one-way between-groups analysis of variance was conducted to explore the impact of type of bariatric surgery on %EWL. There was no statistically significant difference at the p < 0.05 level in %EWL between types of surgery: F (3, 137) = 1.34, p = 0.26. An independent-samples t-test was conducted to compare %EWL between males and females. There was no significant difference between males (64.1% ± 21.0%) and females (61.9% ± 14.9%): t (139) = 0.74, p = 0.46, two-tailed. The magnitude of the differences in the means (mean difference = 2.24, 95% CI: -3.76 to 8.23) was very small (eta squared = 0.004).
Figure 3: Relationship Between Age and Percentage Excess Weight Loss.
Discussion
This study re-emphasises existing evidence that bariatric surgery in patients with super morbid obesity is indeed effective for weight loss and resolution of co-morbidities. Another study in a Middle Eastern population found a similar %EWL of 57.1%, recommending that bariatric surgery should be offered to patients with super morbid obesity [9]. A study in the USA paralleled similar improvement with patients decreasing from a pre-operative BMI of 56.8 kg/m2 to a 12 month post-operative BMI of 40.1 kg/m2 [10]. Studies also find good resolution of T2DM (73.3%), HTN (73.6%) and OSA (100%) [9, 11]. The relationship between increasing age and poorer weight loss has been seen in other research [12]. Despite this, poorer % EWL appears to be clinically insignificant, and studies overall emphasise good %EWL in the specific super-morbidly obese elderly populations, with 56.7% ± 22.0% at a mean follow up of 33 months and 52.2% ± 23.8% at a follow up of 42 months [13, 14]. It is therefore suggested that bariatric surgery in the super morbidly obese elderly is effective.
Current literature, as reviewed by Peterson K et al., runs contrary to this investigation’s finding of there being no difference in % EWL between different types of bariatric surgery in the super morbidly obese population [15]. This may indicate a difference in response to bariatric surgery for patients in Bahrain compared to other countries, however a more likely explanation may be an insufficient number of patients in each bariatric surgery group of our study, with only 23 in the OAGB group, 16 in BPD, and 13 in SGTLB. A larger, multicentre study would be required to gain sufficient statistical power for more certain conclusions in the Gulf population.
Strengths of this study include that a single surgical team operated on all patients, reducing potentially influencing factors. The entire hospital population was investigated rather than a sample, providing good internal validity for this centre. This population is also very representative of patients in the Middle East, allowing surgeons in this region to extrapolate findings for their own decisions. However, the number of patients were limited, in some groups (e.g. patients with T2DM and patients in different bariatric surgery groups) there may have been too few to come to confident conclusions. Furthermore, the short term follow up of 12 months does not address the existing gap in literature for longer follow up over at least 5 years [15].
In fact, this study initially aimed to assess long term (5 year) bariatric surgery outcomes for patients with super morbid obesity, however on inspection of data we found great loss to follow up making the long-term study unfeasible. Moreover, factors such as exercise and level of education could not be assessed due to infrequent reporting. Yet a recent study by Fontana et al. showed that patients with super morbid obesity who adhered to regular physical activity post-operatively benefited from a significant improvement in weight loss, activities of daily living, and quality of life [16]. Therefore, to truly meet the demand for more research in the Gulf, better reporting of such factors, and regular follow up over long term will be necessary.
Conclusion
This study supports many of the findings in current literature. There was a significant %EWL and good improvement in T2DM, HTN and OSA, justifying bariatric surgery for the super morbidly obese population in the Gulf. Although age appears to decrease weight loss outcomes, this is to a minor degree, and surgery is still relatively effective in the super morbidly obese elderly. Nonetheless, the need for more longitudinal research over 5 or more years continues to be echoed not only in the super morbidly obese population, but in all bariatric surgery literature [17]. It is also suggested that factors not yet fully investigated, such as adherence to exercise, may need to be considered for future research as potentially significant contributors to maximising the efficacy of surgery. However, these research goals can only be achieved by first ensuring regular and systematic reporting of key patient information, and encouragement for patients to engage in long term follow up.
Disclosure
This study has received no external funding. The authors declare that they have no conflicts of interest. This study is in accordance with the ethical standards of the Royal College of Surgeons in Ireland – Medical University of Bahrain and KHUH ethical committees, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of retrospective study, formal consent is not required. However informed consent regarding the use of patient information for research was obtained prior to surgery from all individual participants included. The authors would like to acknowledge Dr. Sally Doherty for providing advice and guidance during the course of this study.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 23, Dec 2019Accepted: Mon 06, Jan 2020
Published: Wed 05, Feb 2020
Copyright
© 2023 Abdulmenem Abualsel. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSCR.2019.01.06
Author Info
Abdulmenem Abualsel Ashish Mhatre Nalin Mathur Susan Dovey
Corresponding Author
Abdulmenem AbualselBariatric Surgery Unit, King Hamad University Hospital, Al Sayh, Kingdom of Bahrain
Figures & Tables
Table 1: Patient Characteristics.
|
Age at time of surgery |
|
|
Mean |
35.2 ± 10.6 |
|
Range |
15 - 64 |
|
Gender |
|
|
Male |
65 (45.1%) |
|
Female |
79 (54.9%) |
|
Nationality |
|
|
Bahraini |
136 (94.4%) |
|
Non-Bahraini |
8 (5.6%) |
|
Pre-operative BMI (kg/m2) |
|
|
Mean |
56.9 ± 6.1 |
|
Range |
50.0 - 77.8 |
|
Incidence of obstructive sleep apnoea |
64 (44.4%) |
|
Incidence of hypertension |
43 (29.9%) |
|
Incidence of type 2 diabetes mellitus |
41 (28.5%) |
|
Type of bariatric surgery |
|
|
Sleeve gastrectomy |
90 (62.5%) |
|
One anastomosis gastric bypass |
24 (16.7%) |
|
Biliopancreatic diversion |
16 (11.1%) |
|
Sleeve gastrectomy with transit loop bipartition |
14 (9.7%) |
Table 2: Outcomes 12 Months Post-Operatively.
|
Mean post-operative BMI (N = 141) |
37.7 ± 7.5 kg/m2 |
|
Percentage Excess Weight Loss |
|
|
Mean overall (N = 141) |
62.9% ± 17.9% |
|
Mean after sleeve gastrectomy (N = 89) |
63.3% ± 17.0% |
|
Mean after one anastomosis gastric bypass (N = 23) |
62.8% ± 22.4% |
|
Mean after biliopancreatic diversion with duodenal switch (N = 16) |
56.8% ± 14.1% |
|
Mean after sleeve gastrectomy with transit bipartition (N = 13) |
62.4% ± 15.3% |
|
Mean for males (N = 63) |
64.3% ± 20.9% |
|
Mean for females (N = 78) |
62.4% ± 14.5% |
|
OSA resolution (N = 64) |
61 (100%) |
|
HTN resolution (N = 43) |
38 (88.4%) |
|
T2DM status (N = 34) |
|
|
No improvement |
1 (2.9%) |
|
Remission |
6 (17.6%) |
|
Resolution |
27 (79.4%) |
References
- AlMarri F, Al Sabah S, Al Haddad E, Vaz JD (2017) A Call for More Research from the Arabian Gulf. Obes Surg 27: 2034-2043. [Crossref]
- Al Khalifa K, Violato C, Al Ansari A (2013) Reduction in weight and BMI and changes in Co-morbidities following laparoscopic adjustable gastric banding procedure for morbidly obese patients in Bahrain: a five year longitudinal study. Springerplus 2: 19. [Crossref]
- Saeed MF, Abualsel A, Sakrani NF (2015) Initial One Year Pioneering Experience in Advanced LaparoscopicBariatric Surgery. Bahrain Medical Bulletin 37: 226-229.
- Kakarla VR, Nandipati K, Lalla M, Castro A, Merola S (2011) Are laparoscopic bariatric procedures safe in superobese (BMI≥ 50 kg/m2) patients? An NSQIP data analysis. Surg Obes Relat Dis 7: 452-458. [Crossref]
- Sturm R, Hattori A (2013) Morbid obesity rates continue to rise rapidly in the United States. Int J Obes (Lond) 37: 889-891. [Crossref]
- Uno K, Seki Y, Kasama K, Wakamatsu K, Umezawa A et al. (2017) A comparison of the bariatric procedures that are performed in the treatment of super morbid obesity. Obes Surg 27: 2537-2545. [Crossref]
- Hatoum IJ, Kaplan LM (2013) Advantages of percent weight loss as a method of reporting weight loss after Roux‐en‐Y gastric bypass. Obesity 21: 1519-1525. [Crossref]
- Buse JB, Caprio S, Cefalu WT, Ceriello A, Del Prato S et al. (2009) How do we define cure of diabetes? Diabetes Care 32: 2133-2135. [Crossref]
- Al Falah HM, AlSalamah SM, Abdullah M, AlQahtani HH, Abbas GS et al. (2013) An experience of laparoscopic sleeve gastrectomy in obese, morbidly obese, and super morbid obese patients. Saudi Med J 34: 503-510. [Crossref]
- Onyewu SC, Ogundimu OO, Ortega G, Bauer ES, Emenari CC et al. (2017) Bariatric surgery outcomes in black patients with super morbid obesity: a 1-year postoperative review. Am J Surg 213: 64-68. [Crossref]
- Singla V, Aggarwal S, Garg H, Kashyap L, Shende DR et al. (2018) Outcomes in Super Obese Patients Undergoing Laparoscopic Sleeve Gastrectomy. J Laparoendosc Adv Surg Tech A 28: 256-262. [Crossref]
- Scozzari G, Passera R, Benvenga R, Toppino M, Morino M (2012) Age as a long-term prognostic factor in bariatric surgery. Ann Surg 256: 724-729. [Crossref]
- McGlone ER, Bond A, Reddy M, Khan OA, Wan AC (2015) Super-obesity in the elderly: is bariatric surgery justified? Obes Surg 25: 1750-1755. [Crossref]
- Elbahrawy A, Bougie A, Loiselle SE, Demyttenaere S, Court O et al. (2018) Medium to long-term outcomes of bariatric surgery in older adults with super obesity. Surg Obes Relat Dis 14: 470-476. [Crossref]
- Peterson K, Anderson J, Boundy E, Ferguson L, Erickson K (2017) Rapid evidence review of bariatric surgery in super obesity (BMI≥ 50 kg/m 2). J Gen Intern Med 32: 56-64. [Crossref]
- Fontana AD, Lopes AD, Lunardi AC (2019) Bariatric Surgery Associated with Practice of Moderate to Intense Physical Activity Related to Weight Loss, Activity Level in Daily Life, Dyspnea, and Quality of Life of Sedentary Individuals with Morbid Obesity: a Prospective Longitudinal Study. Obes Surg 29: 2442-2448. [Crossref]
- Colquitt JL, Pickett K, Loveman E, Frampton GK (2014) Surgery for weight loss in adults. Cochrane Database Syst Rev (8):CD003641. [Crossref]
