Oral Methadone for Cancer Pain Management at the End of Life: A Forgotten Drug
A B S T R A C T
Background: Opioids are used for pain management in cancer patients. Morphine is considered the best option. For some patients with pain of difficult control management and adverse effects, an opioid rotation should be considered. Oral methadone is an opioid to which patients can be rotated safely and effectively and inexpensive for Mexico and Latin America. Our study describes the 9-year experience of opioid rotation to methadone, the population profile, efficacy of methadone in cancer patients of the palliative care service.
Methods: Retrospective study of cancer patients rotated to oral methadone for pain control. Tables of frequencies, median and interquartile ranges were made, as well as overall survival.
Results: 311 patients were rotated to methadone, predominantly males (58.5%), median age of 54 years with oncological diagnoses in cervix (10.3%), germinal tumors (8.4%), breast (8.0%), prostate (7.4%) and rectal (5.5%). These patients experienced visceral (17.6%) or other types of pain (68.6%), and a combination of different types of pain, the most prevalent pain was neuropathic (88.7%) and 50% received morphine, 21% buprenorphine or fentanyl 19% previously, with a median dose of 60 mg (30-120). The main reason for rotation was difficult pain control (54%), obtaining an efficacy of 70.0%.
Conclusion: In this cohort at advanced disease stage, 54% suffered from difficult pain control, thus rotation became necessary, reducing pain and manageable adverse events, without major changes of the initial and final dose. Should be promoted more widely in the management of pain of difficult control by cancer in first position prescription.
Keywords
Opioid rotation, difficult pain control, methadone, palliative care, cancer
Introduction
Strong opioids are the gold standard for severe cancer pain, at the present time several options are available; however, morphine is the recommended choice by the World Health Organization (WHO), particularly in Low- and Middle-income countries [1]. Nevertheless, as cancer progresses, pain control could be difficult, and adverse effect of high morphine doses can surpass the benefits of its use, therefore, opioid rotation using correct equianalgesic conversion techniques to achieve better analgesia and/ or fewer side effects [2]. Although there are several retrospective studies on opioid rotation few controlled trials have been reported; nevertheless, rotation is a commonly practiced intervention for managing opioid toxicity or resistant pain [3-5]. Methadone is a cost‐effective opioid when high doses of opioids are necessary, lack of known active metabolites, therefore, has been used for opioid rotation in some studies. Nevertheless, its long and unpredictable half‐life and a relatively unknown equianalgesic dose compared with other opioids have limited a more frequent use [6]. The purpose of this report is to describe our institution’s 9-year experience in the use of oral methadone in advanced cancer patients seen at the Palliative Care Service.
Materials and Methods
A retrospective study of patients seen at the palliative care service between January 2011 to December 2019 was conducted. Electronic charts of patients receiving oral methadone were reviewed. Sociodemographic characteristics, site of cancer, presence of pain, type and intensity of pain was documented with VAS (visual analogue scale) and ESAS (Edmonton Symptom Assessment System), initial opioid treatment and doses were recorded, reasons for rotation to methadone and responses were also documented. Pain score after one month of treatment and side effects, median doses of methadone were also recorded. All opioid doses were converted to oral morphine equivalent daily dose (MEDD) [7].
Statistical Analysis
Measures of central tendency and dispersion included median and interquartile range (IQR) while categorical data were described as percentages. Wilcoxon tests were performed to evaluate differences. Data analysis was carried out with Stata 12.1 software [8]. The protocol was approved by the Ethics and Research Committees of (Rev/92/16).
Results
A total of number of 9936 cancer patients were seen during the study period, 311 (3.1%) were rotated to oral methadone. Sociodemographic characteristics are shown in (Table 1). The median age of this group of patients was 54 years (38-61), a higher percentage of males were seen (58.5%). All patients had advanced cancer; however, some were receiving antineoplastic palliative treatments. The most frequent types of cancer were cervicouterine tumors, germinal tumors, breast, prostate, rectum. Most patients (90%) had low income, although anticancer treatment was included in the Social Protection Plan implemented by the Ministry of Health. Most patients had severe (6/10) pain syndrome in several locations. A neuropathic component was present in 88% of patients. Increasing doses of morphine were required in 155 (50%) patients; 21% (58 patients) were receiving buprenorphine because of renal dysfunction, and 20% had been rotated to fentanyl; substance abuse history was present in 5.2% of the patients. These multifactorial causes make pain difficult to control in this population. Ten patients were receiving more than 300 mg MEDD (Table 2).
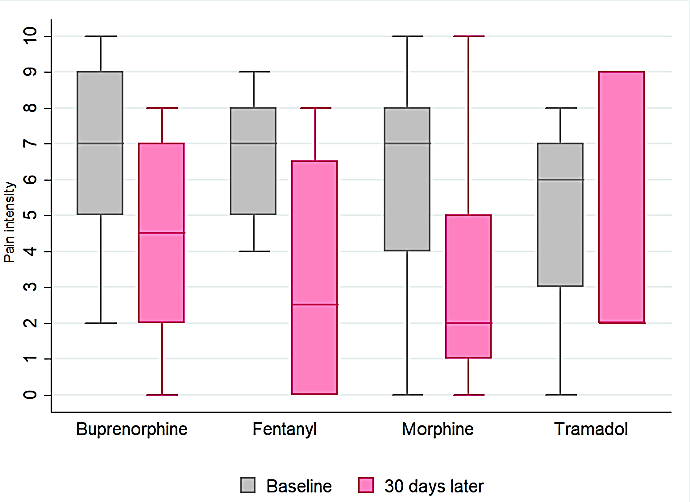
Figure 1: Change in pain intensity (VAS & ESAS) according to previous opioid, before and after methadone rotation in cancer patients.
Table 1: Demographic and clinical characteristics of patients rotated to methadone between 2011 and 2019 (n=311).
|
Characteristics |
Absolute frequency |
Relative frequency |
|
Sex |
||
|
Male |
182 |
58.5 |
|
Female |
129 |
41.5 |
|
Age |
||
|
Median (IQR) |
54 (38-61) |
|
|
Marital status |
||
|
Married |
180 |
58.8 |
|
Single |
126 |
41.2 |
|
Monthly income |
||
|
Median (IQR) |
145.8 (100-237.5) |
|
|
Place of Origin |
||
|
Mexico City |
109 |
35.6 |
|
Other** |
202 |
64.4 |
|
Cancer diagnoses |
|
|
|
Cervicouterine |
32 |
10.3 |
|
Germinal Tumors |
26 |
8.4 |
|
Breast |
25 |
8.0 |
|
Prostate |
23 |
7.4 |
|
Rectum |
17 |
5.5 |
|
Kidney |
12 |
3.9 |
|
Lung |
11 |
3.6 |
|
Other types |
165 |
53.0 |
|
Clinical stage ɣ |
|
|
|
I |
3 |
1.0 |
|
II |
18 |
5.9 |
|
III |
46 |
15.0 |
|
IV |
183 |
59.8 |
|
Type of pain ɣ |
|
|
|
Somatic |
28 |
9.1 |
|
Neuropathic |
14 |
4.6 |
|
Visceral |
54 |
17.6 |
|
combinations of different types of pain |
210 |
68.6 |
* Marital status (Other): unmarried couple, separated and divorced.
**Place of origin (Other): Oaxaca, Puebla, Guerrero, Hidalgo, Michoacán, Morelos, Nuevo León, Coahuila and Sinaloa.
ɣ In these variables figures do not match the total since not all information was available.
IQR: Interquartile range.
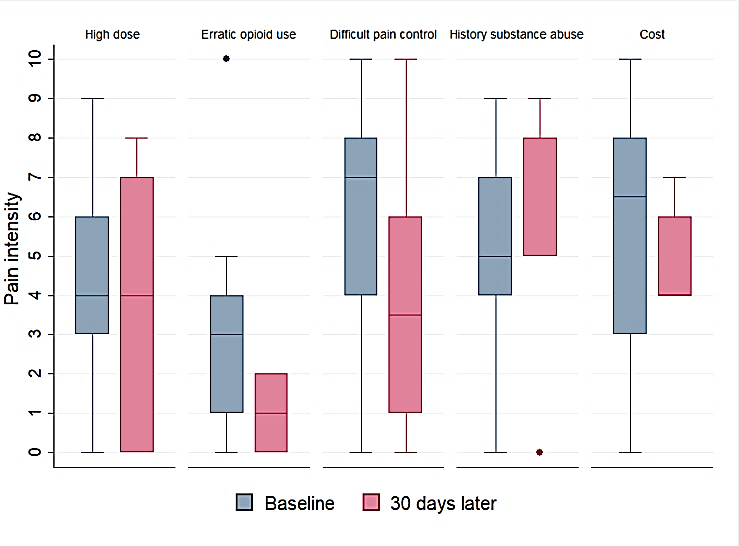
The median MEDD 60 mg (30-120), median initial methadone dose was 75 mg (50-100), titration was required in most of the patients up to 100 mg (75-150 mg). Cervicouterine cancer patients required the highest dosages by neuropathic pain (Table 3). Increased constipation, nausea and vomiting (compared with the previous opioid treatment), was present in 7 patients (2.2%). No severe adverse events or toxicities were documented. Improvement of pain was seen in 62% patients, (median 4) p = 0.00001. The intensity of pain in those patients decreased at least 50%. Pain worsened in 30% patients, in some of these, tumor progression was documented. Interestingly, no changes and increase of pain was reported in patients with history of substance abuse; finally, no improvement was seen in 8% patients (Figure 1). In patients with difficult pain control, the median pain decreased from 7.5 to 3.5, in erratic opioid use dropped 3 to 1, according to economic factor 6.5 to 4. Conversely, for history of substance abuse, pain intensity increased from 5 to 8 (Figure 2). Patients received oral methadone treatment after its rotation for 61 days (22-175) with a median of 126 days in Palliative care service.
Table 2: Major indications for opioid rotation in cancer patients
|
Indications |
Frequency (%) |
|
Difficult control pain |
135 (53.6) |
|
History of substance abuse |
13 (5.2) |
|
High dose (MEDD) |
10 (4.0) |
|
Clinical status
|
16 (6.3) |
|
Adverse effects |
5 (2.0) |
|
Practical considerations
|
26 (10.3) |
MEDD: Oral morphine equivalent daily dose.
Table 3: Opioid treatment prior to and at the beginning of rotation.
|
Diagnosis |
Prior opioid (MEDD) |
Initial Methadone (IQR) |
|
Cervicouterine |
127.5 [83.2-232.6] |
100 [75-150] |
|
Germinal tumors |
60 [22.5-120] |
75 [50-75] |
|
Breast |
75 [32.8-157.5] |
68.2 [36.5-75] |
|
Prostate |
64.9 [45-90] |
75 [66.5-100] |
|
Rectum |
90 [60-120] |
90 [75-100] |
|
Lung |
52.5 [30-83.2] |
75 [50-100] |
|
Tongue |
52.5 [27-60] |
75 [50-110] |
|
Penis |
45 [45-45] |
62.5 [33-75] |
|
Endometrium |
38.7 [30-83.2] |
43.7 [33-66] |
|
Renal |
71.6 [36.6-119.4] |
75 [50-90] |
MEDD: Oral morphine equivalent daily dose, IQR: Interquartile range.
Figure 2: Pain intensity according to Indications for opioid rotation before and after methadone rotation in cancer patients.
Discussion
Pain is experienced by over 80% of patients with advanced metastatic disease, the impact of this pain on the quality of life can be devastating, cancer patients with pain report significantly lower levels of performance status and higher levels of total mood disturbance. The complex, multidimensional nature of cancer pain presents challenges for its treatment [9]. Opioid rotation has been shown to be useful in opening the therapeutic window and establishing a more advantageous analgesia/toxicity relation [10]. Methadone has a unique characteristic as the sole long-acting opioid in liquid form. Its wide spectrum of absorption and formulations allows administration using oral formulation [11]. Although Methadone consumption in Mexico is high (2466 mg morphine/per capita); it is mostly prescribed in the Mexico-US border at the drug abuse control clinics [12]. Methadone use for pain control in advanced cancer patients most of the times is not considered and the use of expensive opioids is preferred all over the country [13, 14].
At our institution in the period studied, only 3% of the patients referred to palliative care received methadone, and its use was limited to those patients with pain of difficult control. As shown in this work, patients were young (54 years), the types of cancer and the advanced stage contributed to the complexity for the management as somatic visceral pain and neuropathic pain were often present. Another point we would like to highlight is the low cost of oral methadone, most patients seen have very low income (5 USD/day); therefore, the cost of some of the drugs available may be difficult, and therapeutic adherence is compromised favoring pain of difficult control [14]. Other studies have included similar patients, with similar gender distribution and diagnosis of gastrointestinal and head and neck cancers [15, 16]. The latter 5-year study in France by Rhondali et al., showed 3% of patients rotated to methadone, similar to our report (3.1%). We had 210 patients with mixed pain (up to three types of pain combined), while a retrospective analysis in France showed 17 patients. In their study with the “stop and go” strategy, patients were administered morphine, oxycodone and fentanyl with MEDD dose of 480 mg (100-1021) before being rotated, partially coinciding with our IQR of 60 mg (30-120) [16].
Cancer pain prevalence is high, reaching 75-90% in advanced stage. More than 50% of cases experience moderate to severe pain requiring continuous opioid treatment [17]. Only 20% fails to achieve optimal pain control following the WHO guidelines [18]. These patients with difficult pain control represent 53.6% of our cohort. They were treated with morphine, buprenorphine and fentanyl without achieving adequate analgesia and therefore opioid rotation was required. In a prospective study of 186 cancer patients receiving morphine, 25% did not achieve adequate pain relief [19]. According to safety protocols, patients living alone, with cognitive impairment, lacking a responsible caregiver are considered inappropriate for methadone prescription [20]. Reasons for opioid rotation in our study include difficult pain control, history of substance abuse/risk of erratic opioid use, high doses, clinical status, difficult administration and costs. Similar results were reported in cancer patients receiving opioids with unacceptable analgesia-AE balance. Rotation was prescribed for difficult pain control or uncontrolled pain and AE (50.8%), only AE (28.8%), only uncontrolled pain (15.2%) and patient convenience or preference (4.2%) [21].
In some studies, patients not only rotate to methadone but also to other opioids such as buprenorphine and fentanyl, while in our study all cases rotated to methadone [17]. In another trial conducted in a third level PCS with 200 effective admissions, 80/100 patients were rotated by AE, route, or poor pain management, like our results [15]. Comparing our results with a prospective study conducted in Polish patients, their final methadone dose increased from 48.1 ± 19.7 to 131.1 ± 104.3 while we report a 25% increment. In the same manner 19/21 (90%) Polish patients required increased dose, in contrast to 49/311 (15.7%) in our study [22].
We found low AE frequency after rotation (2.2%), in agreement with previous studies [5]. Constipation was the major AE, whereas reports from Leppert et al. highlight constipation as the second most common side effect [22]. Additionally, methadone rotation was successful in 62% of our patients considering pain reduction and AE, lower to a prospective study with 52 patients rotated to methadone and higher than results from Leppert et al., in a study with 21 patients [22, 23]. Occasionally, severe AE can compromise the therapeutic benefits, not achieving optimal analgesia and tolerance during pain treatment. The clinical challenge lies in not knowing in advance whether the balance between analgesia and AE will be achieved after rotation [5]. In those patients not achieving optimal pain relief after rotation, different reasons were detected, including disease progression. Therefore, the challenge will be to reassess multimodal analgesia and restructure a comprehensive approach.
Conclusion
In this cohort at advanced disease stage, 54% suffered from difficult pain control, thus rotation became necessary, reducing pain and manageable adverse events, without major changes of initial and final dose. It should be promoted more widely in the management of pain of difficult control by cancer in first position prescription. Further controlled studies are warranted to establish the role of oral methadone rotation and its benefits in patients with difficult pain control and other characteristics such as type of cancer, type of pain, history of addiction.
Acknowledgment
The authors thank Bruno Ocampo and Lirio Morales-Parra for data capture.
Funding
None.
Conflicts of Interest
None.
Article Info
Article Type
Research ArticlePublication history
Received: Mon 29, Jun 2020Accepted: Mon 13, Jul 2020
Published: Fri 31, Jul 2020
Copyright
© 2023 Emma Verastegui-Aviles . This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.DDA.2020.01.03
Author Info
Silvia Allende-Pérez Georgina Domínguez-Ocadio Oscar Rodríguez-Mayoral Javier Portilla-Segura Adriana Peña-Nieves Emma Verastegui-Aviles
Corresponding Author
Emma Verastegui-AvilesNational Cancer Institute, Palliative Care Service, Mexico
Figures & Tables
Table 1: Demographic and clinical characteristics of patients rotated to methadone between 2011 and 2019 (n=311).
|
Characteristics |
Absolute frequency |
Relative frequency |
|
Sex |
||
|
Male |
182 |
58.5 |
|
Female |
129 |
41.5 |
|
Age |
||
|
Median (IQR) |
54 (38-61) |
|
|
Marital status |
||
|
Married |
180 |
58.8 |
|
Single |
126 |
41.2 |
|
Monthly income |
||
|
Median (IQR) |
145.8 (100-237.5) |
|
|
Place of Origin |
||
|
Mexico City |
109 |
35.6 |
|
Other** |
202 |
64.4 |
|
Cancer diagnoses |
|
|
|
Cervicouterine |
32 |
10.3 |
|
Germinal Tumors |
26 |
8.4 |
|
Breast |
25 |
8.0 |
|
Prostate |
23 |
7.4 |
|
Rectum |
17 |
5.5 |
|
Kidney |
12 |
3.9 |
|
Lung |
11 |
3.6 |
|
Other types |
165 |
53.0 |
|
Clinical stage ɣ |
|
|
|
I |
3 |
1.0 |
|
II |
18 |
5.9 |
|
III |
46 |
15.0 |
|
IV |
183 |
59.8 |
|
Type of pain ɣ |
|
|
|
Somatic |
28 |
9.1 |
|
Neuropathic |
14 |
4.6 |
|
Visceral |
54 |
17.6 |
|
combinations of different types of pain |
210 |
68.6 |
* Marital status (Other): unmarried couple, separated and divorced.
**Place of origin (Other): Oaxaca, Puebla, Guerrero, Hidalgo, Michoacán, Morelos, Nuevo León, Coahuila and Sinaloa.
ɣ In these variables figures do not match the total since not all information was available.
IQR: Interquartile range.
Table 2: Major indications for opioid rotation in cancer patients
|
Indications |
Frequency (%) |
|
Difficult control pain |
135 (53.6) |
|
History of substance abuse |
13 (5.2) |
|
High dose (MEDD) |
10 (4.0) |
|
Clinical status
|
16 (6.3) |
|
Adverse effects |
5 (2.0) |
|
Practical considerations
|
26 (10.3) |
MEDD: Oral morphine equivalent daily dose.
Table 3: Opioid treatment prior to and at the beginning of rotation.
|
Diagnosis |
Prior opioid (MEDD) |
Initial Methadone (IQR) |
|
Cervicouterine |
127.5 [83.2-232.6] |
100 [75-150] |
|
Germinal tumors |
60 [22.5-120] |
75 [50-75] |
|
Breast |
75 [32.8-157.5] |
68.2 [36.5-75] |
|
Prostate |
64.9 [45-90] |
75 [66.5-100] |
|
Rectum |
90 [60-120] |
90 [75-100] |
|
Lung |
52.5 [30-83.2] |
75 [50-100] |
|
Tongue |
52.5 [27-60] |
75 [50-110] |
|
Penis |
45 [45-45] |
62.5 [33-75] |
|
Endometrium |
38.7 [30-83.2] |
43.7 [33-66] |
|
Renal |
71.6 [36.6-119.4] |
75 [50-90] |
MEDD: Oral morphine equivalent daily dose, IQR: Interquartile range.
References
- World Health Organization (2011) Global status report on noncommunicable diseases 2010. Improving health care: Individual Interventions 176.
- Anderson R, Saiers JH, Abram S, Schlicht C (2001) Accuracy in equianalgesic dosing: Conversion dilemmas. J Pain Symptom Manage 21: 397-406. [Crossref]
- Parsons HA, de la Cruz M, Osta BE, Li Z, Calderon B et al. (2010) Methadone Initiation and Rotation in the Outpatient Setting for Patients With Cancer Pain. Cancer 116: 520-528. [Crossref]
- Watanabe S, Belzile M, Kuehn N, Hanson J, Bruera E (1996) Capsules and suppositories of methadone for patients on high-dose opioids for cancer pain: clinical and economic considerations. Cancer Treat Rev 22: 131-136. [Crossref]
- Mercadante S, Casuccio A, Calderone L (1999) Rapid Switching from Morphine to Methadone in Cancer Patients with Poor Response to Morphine. J Clin Oncol 17: 3307-3312. [Crossref]
- Mercadante S, Casuccio A, Agnello A, Serretta R, Calderone L et al. (1998) Morphine Versus Methadone in the Pain Treatment of Advanced-Cancer Patients Followed Up at Home. J Clin Oncol 16: 3656-3661. [Crossref]
- Hernández Ortiz A (2016) Construction of a nomogram to facilitate the calculation of equianalgesic doses for opioid rotation Revista Mexicana de Anestesiología. Revista Mexicana de Anestesiologia 39: 251-260.
- College Station, TX: StataCorp LP (2011) Stata Statistical Software. Release 12.
- Van den Beuken van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan Heijnen VC, Janssen DJ (2016) Update on Prevalence of Pain in Patients with Cancer: Systematic Review and Meta-Analysis. J Pain Symptom Manage 51: 1070.e9-1090.e9. [Crossref]
- Mercadante S (1999) Opioid rotation for cancer pain: Rational and clinical aspects. Cancer 86: 1856-1866. [Crossref]
- Manfredonia JF (2005) Prescribing methadone for pain management in end of life care. J Am Osteopath Assoc 105: S18-S21. [Crossref]
- Pastrana T, De Lima L, Pons JJ, Centeno C (2013) Atlas de Cuidados Paliativos de Latinoamérica. cartográfica 2013. Houston: IAHPC Press.
- College of physician and surgeons of British Columbia (2019) Methadone for Analgesia Guidelines.
- Goodman Meza D, Medina Mora ME, Magis Rodríguez C, Landovitz RJ, Shoptaw S et al. (2019) Where is the opioid use epidemic in mexico? A cautionary tale for policymakers south of the US-Mexico border. Am J Public Health 109: 73-82. [Crossref]
- Cherny NJ, Chang V, Frager G, Ingham JM, Tiseo PJ et al. (1995) Opioid Pharmacotherapy in the management of cancer pain: a survey of strategies used by pain physicians for the selection of analgesic drugs and routes of administration. Cancer 76: 1288-1293. [Crossref]
- Rhondali W, Tremellat F, Ledoux M, Ciais JF, Bruera E et al. (2013) Methadone Rotation for Cancer Patients with Refractory Pain in a Palliative Care Unit: An Observational Study. J Palliat Med 16: 1382-1387. [Crossref]
- Nersesyan H, Slavin KV (2007) Current aproach to cancer pain management: Availability and implications of different treatment options. Ther Clin Risk Manag 3: 381-400. [Crossref]
- World Health Organization. Cancer pain relief : with a guide to opioid availability [Internet]. 2nd ed. Geneva.
- Riley J, Ross JR, Rutter D, Wells AU, Goller K et al. (2006) No pain relief from morphine? Individual variation in sensitivity to morphine and the need to switch to an alternative opioid in cancer patients. Support Care Cancer 14: 56-64. [Crossref]
- McPherson ML, Walker KA, Davis MP, Bruera E, Reddy A et al. (2019) Safe and Appropriate Use of Methadone in Hospice and Palliative Care: Expert Consensus White Paper. J Pain Symptom Manage 57: 635-645. [Crossref]
- Mercadante S, Ferrera P, Villari P, Casuccio A, Intravaia G et al. (2009) Frequency, indications, outcomes and predictive factors of opioids switching in an acute palliative care unit. J Pain Symptom Manage 37: 632-641. [Crossref]
- Leppert W (2009) The role of methadone in opioid rotation a Polish experience. Support Care Cancer 17: 607-612. [Crossref]
- Mercadante S, Casuccio A, Fulfaro F, Groff L, Boffi R et al. (2001) Switching from Morphine to Methadone to improve analgesia and tolerability in cancer patients: A Prospective Study. J Clin Oncol 19: 2898-2904. [Crossref]
