Journals
Omental Infarction: A Case Treated with Laparoscopic Surgery
A B S T R A C T
Omental infarct is a rare cause of an acute abdomen that arises from an interruption of blood supply to the omentum. Here, we present a case of omental infarct in a 67-year-old gentleman with background history of diabetes mellitus who present unusually with a severe acute onset right hypochondrium pain. Examination revealed that he was tender to touch at the right and was having localized guarding. His inflammatory markers were normal. He was successfully treated with laparoscopy surgery and he was subsequently discharged the following day. Omental infarct cases with right hypochondrium pain can sometimes mimicked acute cholecystitis and management includes laparoscopic surgery which can hasten symptoms resolution and reduces hospital stay, however recommendation for surgery has to be balanced with anesthetics risk and complication of the surgery itself.
Keywords
Omental infarction, right hypochondrium pain, laparoscopic surgery
Introduction
Omental infarct is a rare cause of an acute abdomen that arises from an interruption of blood supply to the omentum and may be caused by torsion of the omentum around its vascular pedicle or venous outflow obstruction or vasculitis or thrombosis of the omental vessel [1]. Depending on the location of the infarction, presentation is typically localized to right lower quadrant, right upper quadrant and left lower quadrant and can sometimes clinically it is often indistinguishable from acute cholecystitis and appendicitis [2]. Omental infarct can be classified as primary or secondary and can occur with or without torsion [3]. Primary Omental infarct, with or without torsion occur commonly in obese patient and is associated with congenital anatomic variation [4]. We present a case of a 67-year-old gentleman without any significant medical history, recent trauma or previous surgery who came into the Emergency Department with an acute abdomen and was found to be having an infarcted omentum and was successfully treated with laparoscopy. His pain improves significantly after the surgery. As there was no clear trigger for his infarcted omental and it’s presentation including location of pain that can varies and often mimic other causes for acute abdomen, we would like to highlight the importance of infarcted omentum as a differential diagnosis in acute abdomen and how surgical management can hasten symptoms resolution and reduce the days of hospital stay.
Case report
67-year-old gentleman with background history of diabetes mellitus presented to Emergency Department with 1 day history of severe acute onset right hypochondrium pain, pain score -8/10. He described the pain as being dull in nature, non- radiating, constantly present throughout the day. He is still opening his bowel regularly and has no nausea, vomiting, constipation, diarrhea and anorexia. He has also denies any previous trauma to the abdomen or any recent surgery or any recurrent episodes in the past. The pain was getting more intense for him throughout the day and any movement seems to aggravate it. Examination revealed that he was tender to touch at the right hypochondriac area, with rebound tenderness and localized guarding. His pain was mainly localized around the right upper quadrant of the abdomen and the other quadrants of the abdomen were soft and non-tender. Bowel sounds was present and hernia orifices were clear. He only had one previous abdominal surgery done in the past- an open appendectomy done 50 years ago. His past medical history includes a type 2 Diabetes mellitus patient on insulin. His inflammatory markers and lactate were within normal range. He has a BMI of 32.7
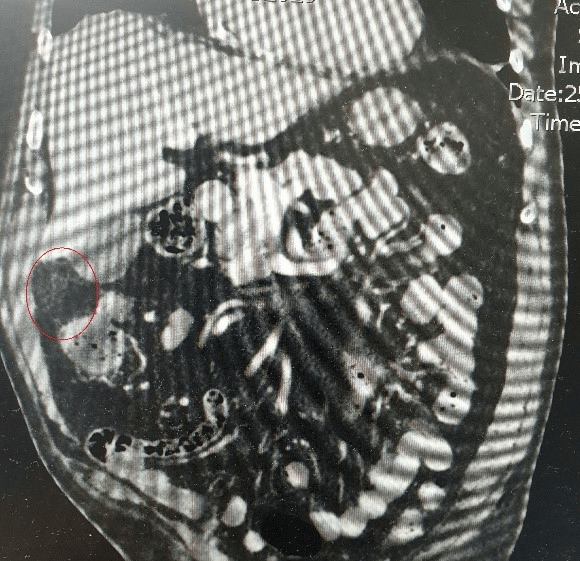
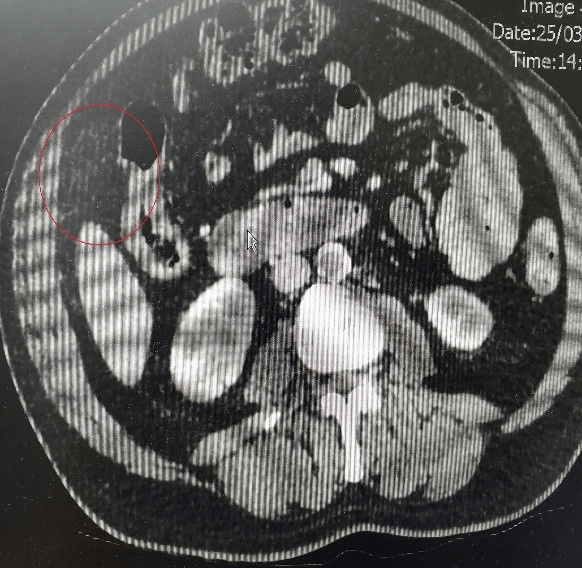
The severity of his pain was a mystery to us and hence an ultrasound was requested to rule out any gallbladder pathology. The ultrasound merely revealed gravel within the gallbladder with no calculi demonstrated, with gallbldder wall normal in thickness and no associated vascularity however there is probe tenderness on examination of the gallbladder. Concern was raising for a missed pathology or a perforated viscus because of the atypical presentation for biliary colic and hence a CT scan of the abdmomen and pelvis were requested. A nonspecific subtle focal fat stranding was noted in the right anterior upper quadrant between the hepatic flexure and fundus of gallbladder which may reflect the omentum or mesentery was noted from the CT scan (Figure 1 & 2). The working diagnosis included an early omental/mesentery ischemia /infarction. The patient was started on Iv antibiotics.
Figure 1: Coronal view on Ct scan. Circle in red - fat stranding in the right anterior upper quadrant.
Figure 2: Axial view on Ct scan. Circle in red- fat stranding in the right anterior upper quadrant.
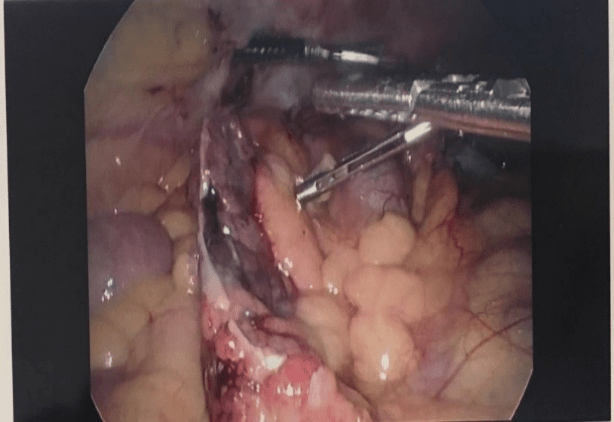
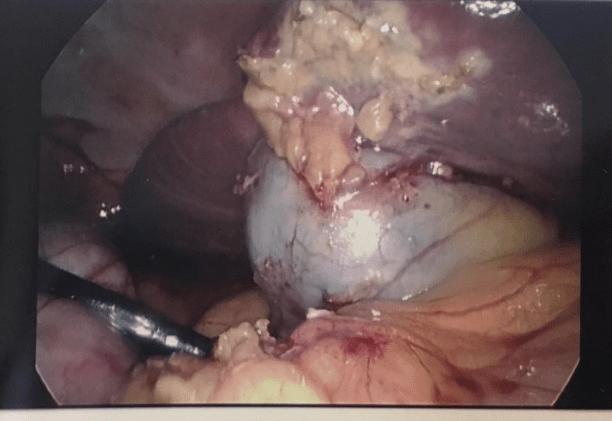
Despite on Iv antibiotics for 24 hours, his pain has not improved, and hence was booked in for a diagnostic laparoscopic in theatre. The images in the operative findings were as below. Intra-operatively there were a piece of infarcted omentum attached to the anterior rim of the liver overlying the gallbladder A few adhesions were noted between the anterior abdominal wall and the omentum and were subsequently divided. The gallbladder appeared normal and there was no other obvious pathology seen. The infarcted omentum were resected with a Harmonic energy device. Photo was taken intraoperatively (Figure 3 & 4). His pain improved significantly post op and was discharged on the second post-operative day.
Figure 3: Omental infarction intra-operative.
Figure 4: Normal Gallbladder
Discussion
Omental infarct in most instances is seen in male patients affecting the right side of the abdomen. Because of its uncommonness, omental infarct depending on the area of infarction can mimicked acute appendicitis, acute cholecystitis, or even acute diverticulitis. Availability of Ct scan in recent years has improved the detection of omental infarct which are most often detected after CT scan these days. OI can be divided into 2 classes -primary and secondary and are commonly associated with risk factors such as anatomic variation in blood supply to the end of omental, obesity, trauma, coughing, sudden body movement and even overeating. Secondary causes for OI include hypercoagulability, polycythaemia, vasculitis and adhesions. Primary cause is classified when there are no recognizable causes found otherwise known as idiopathic. In the above case, we think that this is likely a secondary omental infarct case with torsion likely from adhesion
The exact pathogenesis of the OI is still unclear but there has been many theories of how it occurs. Some authors have suggested that it is due to a different embryonic origin of the right sided omentum as the right sided omentum consist of more fragile blood vessel and are more succeptible to occlusion. Some have also observed that OI typically occurs after a heavy meal and is caused by venous engorgement and similarly in an obese patient whereby excessive weight of the omentum cause venous engorgement and elongation [5].
Till date there is still no studies comparing significant difference between conservative management and surgical management and with limited evidence, management of omental infarct can varies according to the clinician’s experience. A study comparing 10 cases of omental infarction in children showed average stay in hospital for children treated conservatively was 4 days while those treated with laparoscopy was 2 days and required less narcotics [6]. If a patient symptom has not improved after 24 hours of conservative management, laparoscopic management can be considered as it presents with a method for exploration and treatment. At the same time, laparoscopic management overall reduce hospital stay and it is thought to prevent complication of conservative management such as abscess formation [7]. The advantages of operation have to be balanced with the disadvantages of anesthetic risk in treating a patient with OI laparoscopically.
Acknowledgement
None.
Article Info
Article Type
Case ReportPublication history
Received: Wed 07, Aug 2019Accepted: Thu 29, Aug 2019
Published: Thu 12, Sep 2019
Copyright
© 2023 Bertrand Ng. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.IJSCR.2019.02.03
Author Info
Corresponding Author
Bertrand NgGeneral Surgical Department, Hervey Bay Hospital, Associate Lecturer University of Queensland, Australia
Figures & Tables
References
- Scott Kizy, Sayeed Ikramuddin (2019) Abdominal Wall, Omentum, Mesentery, and Retroperitoneum. 1557-1560.
- Lapsia S, Ghai S (2009) Omental infarction: a rare cause of acute abdominal pain. BMJ Case Rep 2009: bcr2006042226. [Crossref]
- Leitner MJ, Jordan CG, Spinner MH, Reese EC (1952) Torsion, infarction and hemorrhage of the omentum as a cause of acute abdominal distress. Ann Surg 135: 103-110. [Crossref]
- Sang Yun Lee, Dong Won Kim, Jin Han Cho, Hee Jin Kwon, Dong Ho Ha et al. (2016) CT Findings of Benign Omental Lesions Following Abdominal Cancer Surgery. J Korean Soc Radiol 75: 1-11.
- Battaglia L, Belli F, Vannelli A, Bonfanti G, Gallino G et all. (2008) Simultaneous idiopathic segmental infarction of the great omentum and acute appendicitis: a rare association. World J Emerg Surg 3: 30. [Crossref]
- Nubi A, McBride W, Stringel G (2009) Primary omental infarct: conservative vs operative management in the era of ultrasound, computerized tomography, and laparoscopy. J Pediatr Surg 44: 953-956. [Crossref]
- Sánchez Fuentes PA, López López V, Febrero B, Ramírez P, Parrilla Paricio P (2015) Omental Infarction: Surgical or Conservative Management? Cir Esp 93: 475-477. [Crossref]
