Occult Breast Cancer with Axillary Involvment in Breast with Scattered Fibroglandular Densities – It Just May Not Appear as It Used to Do: Case Report
A B S T R A C T
Occult breast cancer (OBC), which is defined as clinically recognizable axillary metastatic carcinoma from an undetectable primary breast tumor, occult from conventional breast cancer screening imaging methods. This case reveals an unexpected OBC in a patient with predominantly adipose breasts, with only a few scattered areas of fibroglandular density tissue (BI-RADS® breast composition B), in which the mammographic sensitivity is approximately 90% for the diagnosis of primary breast câncer.
Keywords
Breast, occult, occult breast cancer, axillary metastases, MRI
Introduction
Occult breast cancer (OBC), which is defined as clinically recognizable axillary metastatic carcinoma from an undetectable primary breast tumor, occult from conventional breast cancer screening imaging methods, comprising approximately 0.3% to 1% of all breast cancer (BC) cases [1, 2]. Despite advances in diagnostic imaging that can identify a greater number of primary tumors, numerous incidences continue to occur in which imaging studies fail to locate the primary tumor site. Although criticized for high false positive rate in BC diagnosis, the role of magnetic resonance imaging (MRI) is crucial in the investigation of OBC. Its sensitivity for detecting the disease is 70 to 86% [3-5]. This case reveals an unexpected OBC in a patient with predominantly adipose breasts, with only a few scattered areas of fibroglandular density tissue (BI-RADS® breast composition B), in which the mammographic sensitivity is approximately 90% for the diagnosis of primary breast cancer.
Case Report
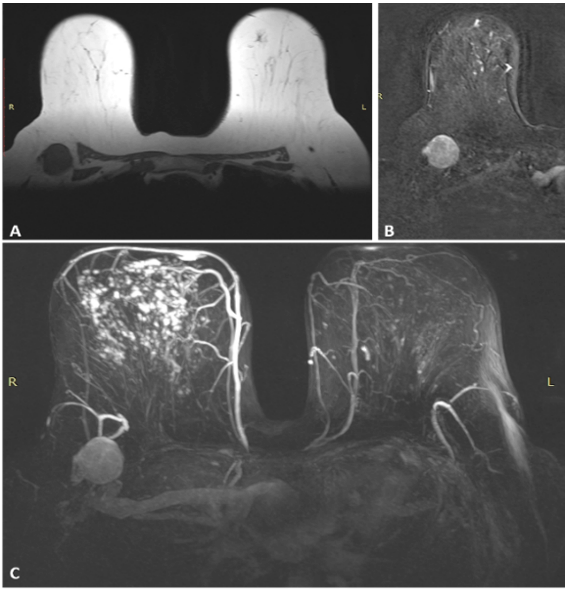
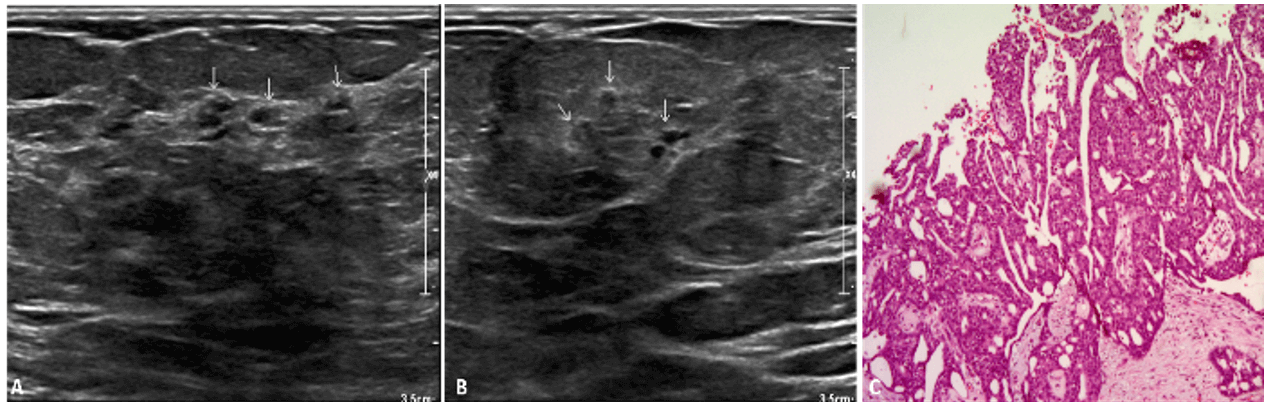
A 69‐year‐old patient underwent screening mammography, that showed the presence of right axillary atypical lymph node (LN), without breast lesion, leading to further investigation (Figure 1). Clinically, she had palpable axillary LN. The admission ultrasound (US) suggested metastatic disease with atypical LN, without breast lesion. US-guided biopsy revealed invasive ductal carcinoma. Immunohistochemistry was positive for HER2 and negative for estrogen and progesterone receptors, suggested being an OBC with axillary nodal metastasis. Further investigation including a MRI of the breast confirmed right axillary lymphadenopathy and also demonstrated a heterogeneous non mass enhancement area, extending for about 50% of the right breast (Figure 2). Therefore, a second look US was performed and a breast suspicious lesion was located. A biopsy proved the location of the primary tumor site (Figure 3).
Figure 1: A & B) Screening mammography shows an axillary lymph node on the right, hyperdense and enlarged (4.0 cm) and breast with scattered areas of fibroglandular density tissue, without any radiological signs of malignancy.
Figure 2: MRI shows: A) T1-weighted image shows a 4.0 cm, enlarged LN with loss of the fatty hila in the right axilla and B) early and heterogeneous enhancement after gadolinium administration. C) Maximum intensity projection (MIP) image of contrast-enhanced MRI shows regional and heterogeneous non mass enhancement in the right breast, involving the medial breast as well as the upper outer quadrant, BI-RADS category 4.
Figure 3: A & B) Second look US shows heterogeneous focal area (non mass lesion) with cystic áreas at upper outer quadrante (arrows). C) Biopsy revealed invasive ductal carcinoma.
Discussion
When metastatic tumors are detected in the axillary lymph nodes, 90% of the primary le¬sions of origin are breast tumors; other possible primary lesions in¬clude melanoma, lymphoma, lung cancer, thyroid cancer, gastrointestinal adeno¬carcinoma, and ovarian carcinoma [6]. Histological examination of the axillary lymph nodes is critical for diagnosis; the primary lesion can be diagnosed as breast cancer if estrogen receptor expression is detected by immunohistochemical staining [7]. OBC is an uncommon presentation of a common disease and even in cases of breasts composition B of BI-RADS®, the role of MRI stands out, proving to be a useful and powerful tool that increases the chance of detection and predicts local extension disease, thus contributing to better therapeutic planning. Finally, breast biopsy remains essential for diagnostic confirmation and second look US should be the preferred method for its guidance, in the presence of a positive correlation between imaging methods.
Conflicts of Interest
None.
Article Info
Article Type
Case ReportPublication history
Received: Mon 02, Nov 2020Accepted: Thu 03, Dec 2020
Published: Mon 21, Dec 2020
Copyright
© 2023 Gustavo Machado Badan. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Hosting by Science Repository.DOI: 10.31487/j.JSO.2020.05.04
Author Info
Gustavo Machado Badan Ana Cristina Lessa Marcos Lessa Guilherme Novita Amanda Neves Machado
Corresponding Author
Gustavo Machado BadanBreast Imaging Service of Radiology Department, United Health Group Brazil, São Paulo, Brazil
Figures & Tables

References
- Oualla K, Elm’rabet F, Arifi S, Mellas N, Melhouf MA et al. (2012) Occult Primary Breast Cancer Presenting With Axillary Nodal Metastasis: Report of 3 Cases. J Clin Gynecol Obstet 1: 85-88.
- Wang X (2007) Presentation of Axillary Metastases from Occult Breast Carcinoma. Chin J Clin Oncol 4: 1-5.
- Bresser J, Vos B, Ent F, Hulsewe K (2010) Breast MRI in clinically and mammographically occult breast cancer presenting with an axillary metastasis: A systematic review. Eur J Surg Oncol 36: 114-119. [Crossref]
- Aguillar VLN, Tucunduva TCM, Carvalho FM, Mazucato MB, Viana MP et al. (2020) Tattoo pigment mimicking calcifications in axillary lymph nodes: A pitfall in mammographic imaging evaluation. Breast J 26: 764-766. [Crossref]
- Navarro LC, Falcao Junior PC, Rezende ASM, Vieira RAC (2020) Occult breast cancer associated with lymph node microcalcifications. Breast J 26: 784-785. [Crossref]
- Kim Y, Kim H, Cho J, Kwon S, Yeo S et al. (2016) The Results of Occult Breast Carcinoma Treated with Axillary Node Dissection Only: Five Cases Reports. J Breast Dis 4: 24-27.
- Montagna E, Bagnardi V, Rotmensz N, Viale G, Cancello G et al. (2011) Immunohistochemically defined subtypes and outcome in occult breast carcinoma with axillary presentation. Breast Cancer Res Treat 129: 867-875. [Crossref]
